Abstract
An increasing body of evidence supports the important role of adhesion to bone marrow microenvironment components for survival and drug resistance of multiple myeloma (MM) cells. Previous studies suggested that stimulation of Toll-like receptors by endogenous ligands released during inflammation and tissue damage may be pro-tumorigenic, but no studies have been performed in relation to modulation of cell adhesion and drug cytotoxicity. Here, we investigated the effect of TLR1/2 activation on adhesion of human myeloma cells to fibronectin, and their sensitivity to the proteasome inhibitor Velcade. It was found that TLR1/2 activation with Pam3CSK4 increased the cytotoxicity of Velcade in L363, OPM-2 and U266 human myeloma cells. This effect was not related to a decreased adhesion of the cells to fibronectin, but TLR1/2 activation stimulated the caspase-3 activity in Velcade-treated myeloma cells, which may be responsible for the enhanced cell death. Inhibitors of NF-κB and MAPK reduced the stimulatory effect. These findings indicate that TLR activation of MM cells could bypass protective effects of cell adhesion and suggest that TLR signaling may also have antitumorigenic potential.
Similar content being viewed by others
Introduction
Signal transduction following integrin binding increases survival, invasion and resistance to apoptosis in many cancer cells.1, 2, 3, 4, 5 In multiple myeloma (MM), this interaction is primarily seen in the bone marrow microenvironment where malignant plasma cells adhere to fibronectin (FN) or stromal cells contributing to induction of cytokines involved in angiogenesis and osteoclastogenesis,6, 7 and tumor cells survival, invasion and drug resistance.5, 7, 8, 9, 10 Although the detailed molecular mechanism(s) underlying this resistance has yet to be delineated, most recent studies have documented VLA-4 (CD49d/CD29, α4β1) and to a lesser extent VLA-5 (CD49d/CD29, α5β1) integrin molecules on MM cells to be involved in their adhesion to FN, and hence induce the so called ‘cell adhesion-mediated drug resistance’.11, 12, 13, 14, 15, 16, 17 Notably, increase in drug resistance of MM cells correlates with their increased adhesion to FN and overexpression of VLA-4.11, 12 Moreover, cytokines secreted by bone marrow stromal cells (BMSCs) could enhance adhesion of MM cells to FN, contributing to MM cell survival and drug resistance.18 Thus, modulating MM cell adhesion to stroma or FN may have beneficial therapeutic effects in combination with anti-neoplastic drugs.
In recent years, a special focus has been made on the role of Toll-like receptor (TLR)-mediated signaling effects in MM cells and human myeloma cell lines (HMCLs) biology. TLRs are germ line encoded and conserved receptors detecting pathogen-associated molecular patterns (PAMPs) to elicit innate immune responses and shape the adaptive immunity.19 Following triggering by their relevant exogenous or endogenous ligands, TLRs provoke secretion of a variety of pro-inflammatory cytokines, which if takes place in a tumor environment might optimize or derange tumor activity, a feature designated as ‘double edged sword’ of innate immunity.20 The function of TLRs may be of particular interest linking inflammation to MM pathogenesis.21 A few recent studies have reported higher levels of TLR expression on MM cells compared with normal plasma cells, and induction of survival, proliferation, drug resistance and immune escape upon TLR triggering in stroma-free conditions.22, 23, 24, 25, 26, 27 However, current knowledge suggests that TLR activation of B-cell neoplasia can result in both positive and negative outcomes.28 In this study, we investigated the effect of TLR1/2 triggering on survival and drug resistance of adhered MM cells. We show that Pam3CSK4, a well-known TLR1/2 agonist,19, 29 has differential effects on adhesion of HMCLs to FN, but TLR1/2 stimulation combined with Velcade increases the cell death of FN-adhered MM cells.
Materials and methods
Cell lines and cell culture
Human myeloma cell lines (HMCLs), Fravel, L363, UM-6, OPM-1, OPM-2, U266, RPMI-8226 and NCI-H929, were obtained from American Type Culture Collection (Manassas, VA, USA). UM-6 had been established by the Department of Clinical Chemistry & Hematology, Utrecht University Medical Center, The Netherlands. The cell lines were maintained in RPMI medium containing 2 mM L-glutamine, supplemented with 5% fetal bovine serum (FBS) and intermittently with 100 U/ml penicillin and 100 μg/ml streptomycin at a humidified 37 °C incubator providing 5% CO2. To UM6 cell line was added 1 ng/ml of recombinant human IL-6 (from eBioscience, San Diego, CA, USA). NCI-H929 cell line was also treated with 1 mM sodium pyruvate and 50 μM 2-mercaptoethanol. Cells were cultured for maximal 15 passages after thawing.
Reagents and antibodies
TLR1/2 ligand (Pam3CSK4) was obtained from Invivogen and dissolved in sterile water according to manufacturer’s instructions to make a 1 mg/ml stock. Velcade (Bortezomib) was from LC laboratories (Woburn, MA, USA) and dissolved in DMSO to prepare 100 mM stocks. Pathway inhibitors, Bay 11–7082 (inhibitor NF-κB), Doramapimod (inhibitor MAPK) and NVP-BEZ235 (inhibitor PI3K/mTOR), were obtained from Invivogen (San Diego, CA, USA) and LC Laboratories, respectively. They were dissolved in DMSO (Bay 11–7082 and Doramapimod) and dimethylformamide (NVP-BEZ235) to make 100 mM stocks.
AMC (7-Amino-4-methylcoumarin) powder and caspase-3 substrate acetyl-Asp-Glu-Val-Asp-7-amido-4-methylcoumarin (Ac-DEVD-AMC) were obtained from Sigma (Munich, Germany) and Bachem (Bubendorf, Switzerland), respectively, and also dissolved in DMSO. The final concentration of solvents in all experimental conditions never exceeded 0.1%. The antibodies used in western blotting experiments were as follows: rabbit monoclonal, anti-human cleaved caspase-3 (clone D3E9, Cell Signaling Technology, Danvers, MA, USA), rabbit monoclonal anti-human pro-caspase-3 (clone E83–103, Epitomics, Burlingame, CA, USA), rabbit polyclonal anti-human p53, p73, BCL-2, Bax (GeneTex, Irvine, CA, USA), HRP-conjugated goat anti-rabbit immunoglobulins from DAKO (Glostrup, Denmark), or anti-rabbit IgG and IgG1 from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Mouse anti-human β-actin Ab was also from Santa Cruz Biotechnology.
Fluorometric adhesion assay
Adhesion to FN was measured as described previously.30 In detail, cells were treated with or without Pam3CSK4 (1–5 μg/ml) for 24 h, washed and added to FN-coated 96-well plates for adhesion assay as follows. Ninety-six-well plates (Costar) were coated with 10 μg/ml FN (human plasma-derived, Sigma) in HBSS, and left for 1 h at 37 °C. To block non-specific binding, heat-denatured BSA (10 mg/ml) in PBS was added after removing FN, and plates were left for 30 min at 37 °C or room temperature. Immediately before use, plates were washed once with HBSS buffer. Then, one million cells out of each condition (treated or untreated) were harvested, washed twice in PBS buffer and suspended in 1 ml of room temperature RPMI medium without any additive. Cell suspensions were labeled with Calcein-AM (1-2 μM) for 30 min at room temperature with gentle mixing after 15 min. To stop labeling, samples were washed/spun twice with ice cold PBS at 4 °C. One milliliter of RPMI plus 2% FBS was added to all samples and 105 cells were seeded on FN-coated 96-well plates, which were incubated at 37 °C for 1 h. At the end of the incubation time, total and spontaneous fluorescence were measured with a plate reader (Mithras LB 940; Berthold Technologies; Germany). For measuring adhered fluorescence, non-adhered cells were removed with two gentle washes using warm RPMI, 100 μl RPMI was added to each well and the plate was read as above. For background readings, fluorescence of the wells containing cells adhered only to BSA was considered. The following formula was used to calculate percentage of adhesion: (Fluorescence reading of adhered cells−background reading) × 100/(Total fluorescence reading−spontaneous reading).
Cell viability: growth inhibition assay (drug cytotoxicity)
Drug cytotoxicity studies were modified after a previously described protocol for acute drug exposure.12 In detail, 1 day before drug exposure, 96-well plates (Costar) were coated overnight (4 °C) with 20 μg/ml FN in HBSS buffer, and blocked with 10 mg/ml sterile heat denatured BSA in PBS at 37 °C for 30 min. HMCLs were first stimulated with 2.5 μg/ml (OPM-2) or 5 μg/ml (L363 and U266) Pam3CSK4 for 24 h. Cells were washed with PBS twice and 5 × 104cells from each cell line were treated with different concentrations of Velcade in RPMI +5%FBS in separate 96-well round bottom plates for 1 h at a 37 °C incubator, with gentle shaking after 30 min. Cells were then washed with RPMI, resuspended in RPMI+FBS and transferred to the 96-well flat bottom plates pre-coated as above. The plates were further incubated for 48 h. At the last 4 h of incubation, 25 μl from XTT reagent with phenazinemethosulfate (PMS) was added to each well, and after 4 h the absorbance (at 450 nm) of each well was measured using a plate reader. The percent survival of the cells was calculated by using non-linear regression. In each plate run, wells for solvent control (medium+cells+DMSO), blank (medium+DMSO) and growth control (medium+cells) were also included. The readings of the blank wells were subtracted from those of all test samples.
Cell viability: annexin-V apoptosis assay
Myeloma cells were incubated in the presence or absence of Pam3CSK4 for 24 h, washed and transferred to FN-coated 12-well plates for 1–2 h. Unattached cells were removed, fresh medium was added and after 8–12 h incubation, Velcade (5 nM) was added and the incubation was extended for another 48 h (chronic exposure). In parallel, cells were seeded in uncoated wells and treated similarly.
For FACS analysis, cells were removed with cold 5 mM EDTA in PBS, washed once with normal FACS buffer (cold PBS containing 1% BSA and 0.01% sodium azide) and once with binding buffer (eBioscience). The cell pellets were then suspended in 200 μl binding buffer containing 5 μl FITC-conjugated annexin-V and incubated for 10 min at room temperature. After washing with binding buffer, 5 μl propidium iodide in 200 μl buffer was added to each well and samples were analyzed using a Becton Dickinson FACSCantoII flow cytometer (San Jose, CA, USA). The percent-specific apoptosis was calculated using the following formula (adopted from Saha et al.31): (Test−control) × 100/(100−control). Test refers to the treatment with Pam3CSK4, Velcade or Pam3CSK4+Velcade, and control is the cells without any stimulation (baseline).
In separate experiments, HMCLs were first treated with subtoxic concentrations of inhibitors for 1–2 h. Then without washing, Pam3CSK4 was added, the incubation was extended to 24 h and procedure was continued as above. Subtoxic concentrations of inhibitors were determined separately after 24-h incubation and Calcein-AM labeling assay was performed, as previously described.32
Caspase-3 enzymatic activity
Cleaved caspase-3 enzymatic activity was measured as described previously.33 The assay is based on the release of the fluorescent 7-amino-4-methylcoumarin (AMC) moiety following hydrolysis of the peptide substrate acetyl-Asp-Glu-Val-Asp-7-amido-4-methylcoumarin by the activated enzyme. Briefly, cells were lysed in a buffer consisting of 10 mM HEPES (pH 7.5), 1% IGEPAL, 10% sucrose, 50 mM NaCl, 40 mM β-glycerophosphate, 2 mM MgCl2, 5 mM EDTA and supplemented with a cocktail of protease inhibitors (Complete Mini, Roche (West Sussex, UK)), and left on ice for 30 min. After spinning the samples at 10 000g for 15 min at 4 °C, supernatants were collected and incubated with 1 μM of caspase-3 substrate Ac-DEVD-AMC in each well of a 96-well plate. The plate was placed in a fluorescent plate reader with a built-in 37 °C incubator (Fluoroskan Ascent FL, Thermo Labsystem, Waltham, MA, USA) for 1 h. During this time, substrate was cleaved (AMC release) by active caspase-3 and the fluorescent signals were recorded (excitation 340 nm, emission 460 nm). The activity of caspase-3 was determined as nM AMC/min/ml of cell lysate. A calibration curve was also created using free AMC.
Immunoblotting
Myeloma cells (treated in the same way as for FACS analysis) were lysed in RIPA buffer (150 mM NaCl, 1% IGEPAL, 0.5% sodium deoxycholate, 0.1% SDS, 50 mM Tris and pH 8.0) containing a cocktail of protease inhibitors (Complete Mini, Roche). After determining the protein concentration with a BCA kit (Pierce, Rockford, IL, USA), 20–30 μg total protein was fractionated using 12% SDS gel electrophoresis. Proteins were transferred to a PVDF membrane and probed with indicated primary antibodies (1:1000–1:2000) followed by specific secondary antibodies (1:2000–1:4000). The signals were finally developed with ECL (Amersham, Diegem, Belgium).
Gene expression profiling of the p53 signaling pathway
RT2Profiler PCR Array kit (PAHS-027, SABiosciences, QIAGEN Benelux B.V., KJ Venlo, the Netherlands) was used to analyze the expression pattern of an array of 84 genes involved in tumor suppressor protein p53 signaling pathway, including five different housekeeping genes (B2M, HPRT1, RPL13A, GAPDH and ACTB). Briefly, OPM-2 cells were stimulated with 2.5 μg/ml of Pam3CSK4 for 8 h; cells were washed and exposed to FN-coated wells of a six-well plate. After 90 min the unattached cells were removed and fresh medium was added to the wells, and incubation was extended to 24 h. For the last 8 h, 10 nM of Velcade was added and finally total RNA was isolated with RNeasy Mini kit (Invitrogen, Paisley, UK) for cDNA synthesis, which was then applied to the array plate according to the manufacturer’s instructions. The same protocol was also applied to cells without Pam3 stimulation and considered as control group in the assay. For data analysis, threshold cycle values (Ct values) were obtained and fold regulations (up or down) of the test group were calculated over the control group using 2−ΔΔCt algorithm.
Real-time PCR
To confirm differential gene expression detected in the profiling array expression of changed genes in p53 pathway was analyzed by real-time PCR. OPM-2 cells were treated as indicated above and total RNA was isolated using RNeasy Mini kit (Invitrogen). About 500 ng RNA was reverse transcribed using iScript first strand cDNA synthesis kit (Biorad, Hercules, CA, USA) and amplified using the following primers (Isogen, De Meern, The Netherlands): EGR-1, GML, TP63, CDKN1A, IFNB1, FASLG and GAPDH, the primer sequences are given in Supplementary Table S1. We used a two-step protocol in real-time PCR with the following thermal profiles for the primers. For EGR-1, CDKN1A, and IFNB1 primers: 95 °C, 3′ for initial denaturation, 40 cycles of (95 °C, 10′′; 65 °C, 30′′), for P63, FASLG and GML primers, 40 cycles of (95 °C, 10′′; 60 °C, 30′′). A melting curve to validate the amplification was applied to each run and only one peak was observed in all assays.
Statistics
Analysis of variance (one way) and unpaired t-test were performed using GraphPad software (version 5.0; La Jolla, CA, USA). P-values <0.05 were considered as significant.
Results
TLR-1 triggering in HMCLs has differential modulatory effects on their adhesion to FN
Increase in drug resistance of MM cells correlates with their increased adhesion to FN.10, 12, 13, 18 We first tested the effect of Pam3CSK4 on HMCLs adhesion to FN. TLR1/2 stimulation with Pam3CSK4 resulted in a decrease of adhesion to FN by Fravel, OPM-1, OPM-2, RPMI-8226 and NCI-H929 cell lines in a dose-dependent manner (Figure 1). The concentration for optimal inhibition of adhesion varied between 1 and 5 μg/ml for these cell lines. In contrast, three HMCLs L363, UM-6 and U266 showed an increased adhesion in response to Pam3CSK4. In next experiments OPM-2, L363 and U266 were used as representative cell lines of both groups to further investigate the functional consequences of TLR1/2 stimulation.
The effect of Pam3CSK4 on adhesion of HMCLs to FN. Calcein-AM labeled cells were seeded on FN-coated 96-well plates, which were incubated at 37 °C for 1 h. At the end of incubation time, total and spontaneous fluorescence were measured with a plate reader. Data represent the results (mean±s.e.m.) of at least three separate experiments, *P<0.05, **P<0.01, ***P<0.001.
Pam3CSK4 sensitizes HMCLs to Velcade in the context of FN
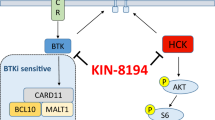
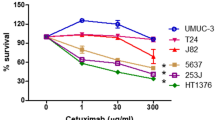
To investigate the effect of TLR-1/2 activation on cell adhesion-mediated drug resistance, Pam3CSK4-stimulated HMCLs were incubated in uncoated vs FN-coated plates, and then exposed to different concentrations of Velcade. In line with previous studies,12, 13 the IC50 of Velcade was higher for cells adhered to FN compared to that for non-adhered cells, suggesting the induction of a cell adhesion-mediated drug resistance (Figure 2). Although TLR-1/2 activation by Pam3CSK4 induced some toxicity, combination of Pam3CSK4+Velcade increased the cell death in all cell lines, as illustrated by a lower IC50 for Velcade compared with control-treated conditions (Figure 2).
Stimulation of TLR1/2 by Pam3CSK4 in combination with Velcade results in increased cell death of HMCLs. HMCLs were treated with Pam3CSK4 or solvent (control) for 24 h, exposed to different concentrations of Velcade for 1 h, washed and seeded in uncoated or FN-coated 96-well plates. Cells were incubated for 72 h, and at the last 4 h XTT containing PMS was added. IC50 for Velcade were determined from the concentration-cell death curves. L363: IC50 (control, non-adhered)=6.8 μM, IC50 (control, adhered)=13.3 μM; IC50 (+Pam3, non-adhered=1.0 μM), IC50 (+Pam3, adhered)=3.5 μM; OPM-2: IC50 (control, non-adhered)=2.75 μM, IC50 (control, adhered)=6.55 μM; IC50 (+Pam3, non-adhered=0.06 μM), IC50 (+Pam3, adhered)=0.288 μM; U266: IC50 (control, non-adhered)=2.35 μM, IC50 (control, adhered)=5.49 μM, IC50 (+Pam3, non-adhered=1.45 μM), IC50 (+Pam3, adhered)=0.88 μM. Data represent calculated mean±s.e.m. of two separate experiments with duplicate measurements in each.
Pam3CSK4 increases the level of apoptosis following exposure to Velcade
Next we investigated whether enhancing the cytotoxic effect of Velcade following Pam3CSK4 stimulation was due to the induction of apoptosis. HMCLs were stimulated with Pam3CSK4 and exposed to Velcade for 24 h as described in Materials and Methods. As depicted in Figure 3, Pam3CSK4 alone caused a substantial level of apoptosis in all HMCLs, but combination of TLR1/2 stimulation with Velcade further increased apoptosis. These findings indicated that TLR-1/2 activation in HMCLs increased their apoptotic response to Velcade treatment.
Pam3CSK4 enhances apoptotic response of L363 (a), OPM-2 (b) and U266 (c) to Velcade in the presence or absence of FN. Left panel shows the FACS analysis of annexin-V FITC staining of L363, OPM-2 and U266. HMCLs were stimulated with Pam3CSK4 for 24 h, washed, incubated in non-coated or FN-coated wells for 8–12 h, and subsequently exposed to 5 nM Velcade for 48 h. Right panel: percent specific apoptosis was determined with annexin-V/PI staining as described in Materials and Methods. Data represent calculated mean±s.e.m. of at least three separate experiments. *P<0.05, **P<0.01, ***P<0.001.
Apoptosis triggered by Pam3CSK4 is paralled by increased caspase-3 activity
We next asked whether the increased apoptotic response induced by Pam3CSK4 was accompanied by activation of the caspase cascade. Intracellular levels of cleaved and pro-enzyme forms of caspase-3 were measured using immunoblotting (Figure 4). Pam3CSK4 alone weakly induced procaspase-3 cleavage in OPM-2 and U266 cell lines but not in L363. A prominent upregulation of cleaved caspase-3 protein was observed in Velcade-treated or Pam3CSK4+Velcade HMCLs, which was accompanied by a complete disappearance of procaspase-3 protein. Next, to understand if Pam3CSK4 alone or its combination with Velcade influenced the enzymatic activity of caspase-3, we assayed its activity using a specific peptide substrate. The enzymatic activity was not significantly increased by Pam3CSK4 alone, while it was most prominently increased in Pam3CSK4+Velcade-treated cells (Figure 5).
The effect of Pam3CSK4 and Pam3CSK4+Velcade on cleavage of pro-caspase-3 protein in the presence or absence of FN in L363 (a), OPM-2 (b) and U266 (c) HMCLs. After treatment with Pam3CSK4 with or without Velcade, non-adhered and FN-adhered HMCLs were analyzed for cleaved and pro-enzyme forms of caspase-3 using western blotting as described in Materials and Methods. β-Actin was used as a housekeeping protein.
The effect of Pam3CSK4 and Pam3CSK4+Velcade on caspase-3 enzymatic activity in the presence or absence of FN in L363 (a), OPM-2 (b) and U266 (c) HMCLs. Caspase-3 activity was determined by the release of the fluorescent 7-amino-4-methylcoumarin (AMC) moiety following hydrolysis of the peptide substrate acetyl-Asp-Glu-Val-Asp-7-amido-4-methylcoumarin (Ac-DEVD-AMC) by the activated enzyme. Data represent calculated mean±s.e.m. of two separate experiments. *P<0.05.
p53 pathway may be indirectly involved in apoptosis-enhancing effect of Pam3CSK4
It has recently been demonstrated that the transcription factor NF-κB and tumor suppressor protein p53 crosstalk to control apoptotic or survival signals transduced through NF-κB.34, 35 As many TLRs activate NF-κB pathway,36 we explored if p53 signaling pathway was involved in controlling the increased apoptosis by Pam3CSK4 in OPM-2 cells. For this purpose, we first determined using a gene array the expression of 84 genes involved in the p53 signaling pathway after treatment with Velcade of control- and Pam3CSK4-stimulated OPM-2 cells. Fourteen genes, which were involved in apoptosis, cell cycle and proliferation, displayed 1.5- to 37-fold upregulation in Pam3CSK4+Velcade-treated cells compared with Velcade-treated only (Supplementary Table S2). Real time PCR analysis of six of these genes (IFNB1, EGR1, GML, FASLG, TP63 and CDKN1A) confirmed the upregulation for EGR1 (4.0-fold) and CDKN1A (3.88-fold). Other genes showed partial upregulation (Supplementary Figure S1).
Interestingly, some other genes related to p53 function also displayed at least 1.5-fold upregulation. These genes included GML (glycosylphosphatidylinositol-anchored molecule-like protein,37, 38, 39), RPRM (REPRIMO, TP53-dependent G2 arrest mediator candidate,40) and KAT2B (lysine acetyltransferase 2B orP300/CBP-associated factor (PCAF)41, 42).
Three genes MYC (cell cycle/proliferation), SESN1 (cell cycle) and TNF (apoptosis) displayed 1.55-, 1.66- and 1.50-fold downregulation, respectively. TP53 and some of its related or target genes such as BCL2, BIRC5, MDM2 and BAX were unchanged, whereas TP73, a p53 family member, showed a 27-fold upregulation.
Analysis at protein level indicated that TLR1/2 stimulation with Pam3CSK4 downregulated p53 and p73 proteins in L363 and OPM-2 cell lines, whereas in U266 it had no effect on p53 and p73 protein levels. Velcade and more significantly Pam3CSK4+Velcade decreased the level of p53 protein in FN-adhered and non-adhered cells. This is in contrast to the recent finding that Velcade would upregulate p53 protein in MM cells in stroma-free conditions.31 Interestingly, in all cell lines Velcade alone or its combination with Pam3CSK4 increased the level of p73 protein. Next, we analyzed BCL-2 and Bax proteins whose balance have a critical role in controlling apoptosis, with upregulation of Bax and downregulation of BCL-2 signifying an apoptotic response.43, 44 As illustrated in Figure 6, in all HMCLs stimulation with Pam3CSK4 did not change BCL-2 and Bax proteins compared with the baseline. Velcade and more significantly Pam3CSK4+Velcade downregulated both proteins. Taken all together, these findings imply that TLR-1/2 triggering could amplify the Velcade-induced expression of genes, which mostly inhibit cell cycle (cell proliferation) or control apoptosis, in part through the p53 signaling pathway.
Apoptosis promoting effect of Pam3CSK4 in HMCLs is inhibited by MAPK and NF-κB inhibitors
Activation of PI3K/Akt, MAPK and NF-κB pathways occurs downstream to integrin engagement, and adhesion-induced drug resistance could partly be explained by activation of prosurvival signals through Ras/MEK/MAPK pathway.7 We tested if interplay of these pathways could explain the apoptosis inducing effect of Pam3+Velcade in FN-adhered cells. HMCLs were first pre-treated with pathway inhibitors before TLR-1/2 stimulation and Velcade exposure as outlined in Materials and Methods. Blocking of PI3K (NVP-BEZ235) pathway inhibited apoptosis in U266, but had no effect on L363 or even increased apoptosis in OPM-2 (Figure 7). Most consistent inhibitory response in all HMCLs was found with the MAPK inhibitor doramapimod, which decreased the level of apoptosis induced by Pam3+Velcade to that induced by Velcade only. Inhibition of the NF-κB pathway with Bay-11–7082 also reduced the Pam3CSK4-induced increase in apoptosis in all HMCLs.
Involvement of MAPK and NF-κB pathway in apoptosis promoting effect of Pam3CSK4 in HMCLs. L363, OPM-2 and U266 were treated with inhibitors of NF-κB (Bay 11–7082), MAPK (Doramapimod) and PI3K/Akt (BEZ235) before Pam3CSK4 treatment and drug exposure. Apoptosis was determined by FACS analysis of annexin-V FITC staining as described in Materials and Methods. Data represent calculated mean±s.e.m. of at least three separate experiments.
Discussion
Induction of apoptotic responses by TLR activation has only been sparsely examined in lymphoid cancers. A recent study indicated that TLR3 activation of MM cells imposed an apoptotic response, which was found to be IFN-α mediated.24 Culture of MM cells with TLR 7 and 9 ligands induces IL-6 secretion, which endows them with resistance against dexamethasone or serum deprivation-induced apoptosis.25 Bohnhorst et al.26 found that stimulation of OH-2 and ANBL-6 myeloma cell lines with Pam3CSK4 induced cellular proliferation, but in this study no effects on the sensitivity to cytotoxic drugs were investigated. Our study is the first to show that cell death of MM cells can be increased by TLR triggering. We demonstrate that TLR1/2 stimulation of HMCLs increase the cytotoxicity of Velcade. Also, the partial drug resistance observed in cells adhered to FN is completely reversed by Pam3CSK4 both in drug cytotoxicity and apoptosis assays. Furthermore, increased drug sensitivity and apoptosis induced by TLR1/2 stimulation is not explained by decreased adhesion of HMCLs. For instance, activation of PI3K/Akt, MAPK and NF-κB pathways occurs downstream to integrin engagement, and adhesion-induced drug resistance could partly be explained by activation of pro-survival signals through Ras/MEK/MAPK pathway.7 Our study shows that inhibition of NF-κB and MAPK pathway greatly inhibits the TLR-1/2-induced increased drug sensitivity in HMCLs. Induction of apoptosis by Pam3CSK4 has already been confirmed in human monocytes,45, 46 but involvement of the caspase activation was not clear in these studies. Here, we demonstrate that stimulation of TLR1/2 by Pam3CSK4 potentiates apoptosis induced by Velcade, which may be regulated at least partly via an increase in caspase-3 activity. Immunoblotting experiments demonstrated that cleavage of pro-caspase-3 into activated caspase-3 is already maximal in Velcade-treated cells, and stimulation of TLR1/2 with Pam3CSK4 did increase the presence of activated caspase-3 (Figure 4). However, TLR1/2 stimulation significantly enhanced the proteolytic activity of caspase-3 in Velcade-treated cells (Figure 5). Caspase-3 activity can be regulated by changes in redox status,29 S-nitrosylation47or phosphorylation.45 Interestingly, phosphorylation by protein kinase Cδ (PKCδ) was specific to caspase-3 and phosphorylation was required to induce apoptosis in monocytes.45 TLR2 triggering has been shown to activate PKCδ in other cells,48 but whether this pathway is involved in the enhancement of caspase-3 activity via PamCSK4 in MM cells is currently under investigation.
Our study may also imply that other pathways in cell survival and apoptosis could be regulated via TLR1/2 stimulation. Recently it was shown there could be crosstalk between NF-κB and p53 pathways to control cell cycle and apoptosis in cancer cells.34, 35 To further understand the mechanism underlying enhancement of Velcade-induced apoptosis by Pam3CSK4, the expression of genes of p53 signaling pathway was compared in Velcade-treated and Pam3CSK4+Velcade-treated OPM-2 cells. p53 protein can upregulate the expression of downstream genes including CDKN1A, BAX and FAS/APO-1, which are implicated in cell growth inhibition and apoptotic cell death.49 Although no effect on BAX gene expression was found, CDKN1A showed a high upregulation (3.88-fold) implying that p53 might display at least part of its function through upregulation of CDKN1A/p21, which has been shown to mediate p53 growth inhibitory effects.50 Furthermore, we found another gene upregulated, EGR1, which exerts its apoptotic function mediated by p53 protein.49 Interestingly, a recent study demonstrated that EGR1 was activated downstream to JUN oncogene in MM cells and promoted apoptosis through interaction with JUN in these cells; furthermore, overexpression of EGR1 was associated with an increased susceptibility to Velcade and a favorable prognosis in MM patients.51
TP53 and its related genes, BCL-2, BIRC5 (survivin) and MDM2, did not change in the expression analysis, while its two family members, TP63 and TP73, were upregulated. We analyzed p53, Bax, BCL-2 and p73 proteins in western blotting to evaluate changes in expression at a post-transcriptional level. We found that TLR1/2 stimulation downregulated protein expression of p53 and p73 in L363 and OPM-2 cell lines but not in U266 indicating a heterogeneity in the response of different myeloma cells to Pam3CSK4. Combination of TLR1/2 stimulation with Velcade further decreased the expression of Bax and BCL-2 protein in all HMCls as compared with Velcade only. To what extent these changes in both pro-apoptotic and anti-apoptotic molecules contribute to the TLR1/2-induced enhanced cytotoxic response remains to be elucidated. Our study suggests that TLR1/2-induced signaling via MAPK and NF-κB may indeed integrate with apoptosis pathways in MM cells (Figure 7).
Taken together, our study indicates that stimulation of TLR1/2 results in enhanced cell death when combined with Velcade, conceivably by enhancing the caspase-3 activity in myeloma cells. Further research into the molecular mechanisms linking TLR activation to drug-induced apoptotic pathways in MM is needed to evaluate if TLR1/2 stimulation by Pam3CSK4 could be useful in the therapy of MM.
References
Aoudjit F, Vuori K . Integrin signaling inhibits paclitaxel-induced apoptosis in breast cancer cells. Oncogene 2001; 20: 4995–5004.
Hehlgans S, Haase M, Cordes N . Signalling via integrins: implications for cell survival and anticancer strategies. Biochim Biophys Acta 2007; 1775: 163–180.
de la Fuente MT, Casanova B, Moyano JV, Garcia-Gila M, Sanz L, Garcia-Marco J et al. Engagement of alpha4beta1 integrin by fibronectin induces in vitro resistance of B chronic lymphocytic leukemia cells to fludarabine. J Leukoc Biol 2002; 71: 495–502.
Aoudjit F, Vuori K . Integrin signaling in cancer cell survival and chemoresistance. Chemother Res Pract 2012; 2012: 283181.
Cordes N . Integrin-mediated cell-matrix interactions for prosurvival and antiapoptotic signaling after genotoxic injury. Cancer Lett 2006; 242: 11–19.
Hideshima T, Mitsiades C, Tonon G, Richardson PG, Anderson KC . Understanding multiple myeloma pathogenesis in the bone marrow to identify new therapeutic targets. Nat Rev Cancer 2007; 7: 585–598.
Podar K, Chauhan D, Anderson KC . Bone marrow microenvironment and the identification of new targets for myeloma therapy. Leukemia 2009; 23: 10–24.
Shain KH, Yarde DN, Meads MB, Huang M, Jove R, Hazlehurst LA et al. Beta1 integrin adhesion enhances IL-6-mediated STAT3 signaling in myeloma cells: implications for microenvironment influence on tumor survival and proliferation. Cancer Res 2009; 69: 1009–1015.
Vacca A, Ria R, Presta M, Ribatti D, Iurlaro M, Merchionne F et al. alpha(v)beta(3) integrin engagement modulates cell adhesion, proliferation, and protease secretion in human lymphoid tumor cells. Exp Hematol 2001; 29: 993–1003.
Ria R, Vacca A, Ribatti D, Di Raimondo F, Merchionne F, Dammacco F . Alpha(v)beta(3) integrin engagement enhances cell invasiveness in human multiple myeloma. Haematologica 2002; 87: 836–845.
Noborio-Hatano K, Kikuchi J, Takatoku M, Shimizu R, Wada T, Ueda M et al. Bortezomib overcomes cell-adhesion-mediated drug resistance through downregulation of VLA-4 expression in multiple myeloma. Oncogene 2009; 28: 231–242.
Damiano JS, Cress AE, Hazlehurst LA, Shtil AA, Dalton WS . Cell adhesion mediated drug resistance (CAM-DR): role of integrins and resistance to apoptosis in human myeloma cell lines. Blood 1999; 93: 1658–1667.
Damiano JS, Dalton WS . Integrin-mediated drug resistance in multiple myeloma. Leuk Lymphoma 2000; 38: 71–81.
Shain KH, Landowski TH, Dalton WS . The tumor microenvironment as a determinant of cancer cell survival: a possible mechanism for de novo drug resistance. Curr Opin Oncol 2000; 12: 557–563.
Hazlehurst LA, Damiano JS, Buyuksal I, Pledger WJ, Dalton WS . Adhesion to fibronectin via beta1 integrins regulates p27kip1 levels and contributes to cell adhesion mediated drug resistance (CAM-DR). Oncogene 2000; 19: 4319–4327.
Meads MB, Hazlehurst LA, Dalton WS . The bone marrow microenvironment as a tumor sanctuary and contributor to drug resistance. Clin Cancer Res 2008; 14: 2519–2526.
Shain KH, Dalton WS . Environmental-mediated drug resistance: a target for multiple myeloma therapy. Expert Rev Hematol 2009; 2: 649–662.
Holt RU, Baykov V, Ro TB, Brabrand S, Waage A, Sundan A et al. Human myeloma cells adhere to fibronectin in response to hepatocyte growth factor. Haematologica 2005; 90: 479–488.
Kawai T, Akira S . The role of pattern-recognition receptors in innate immunity: update on Toll-like receptors. Nat Immunol 2010; 11: 373–384.
Salaun B, Romero P, Lebecque S . Toll-like receptors' two-edged sword: when immunity meets apoptosis. Eur J Immunol 2007; 37: 3311–3318.
Mantovani A, Garlanda C . Inflammation and multiple myeloma: the Toll connection. Leukemia 2006; 20: 937–938.
Liu J, Hamrouni A, Wolowiec D, Coiteux V, Kuliczkowski K, Hetuin D et al. Plasma cells from multiple myeloma patients express B7-H1 (PD-L1) and increase expression after stimulation with IFN-{gamma} and TLR ligands via a MyD88-, TRAF6-, and MEK-dependent pathway. Blood 2007; 110: 296–304.
Chiron D, Jego G, Pellat-Deuceunynck C . Toll-like receptors: expression and involvement in multiple myeloma. Leuk Res 2010; 34: 1545–1550.
Chiron D, Pellat-Deceunynck C, Amiot M, Bataille R, Jego G . TLR3 ligand induces NF-{kappa}B activation and various fates of multiple myeloma cells depending on IFN-{alpha} production. J Immunol 2009; 182: 4471–4478.
Jego G, Bataille R, Geffroy-Luseau A, Descamps G, Pellat-Deceunynck C . Pathogen-associated molecular patterns are growth and survival factors for human myeloma cells through Toll-like receptors. Leukemia 2006; 20: 1130–1137.
Bohnhorst J, Rasmussen T, Moen SH, Flottum M, Knudsen L, Borset M et al. Toll-like receptors mediate proliferation and survival of multiple myeloma cells. Leukemia 2006; 20: 1138–1144.
Xu Y, Zhao Y, Huang H, Chen G, Wu X, Wang Y et al. Expression and function of toll-like receptors in multiple myeloma patients: toll-like receptor ligands promote multiple myeloma cell growth and survival via activation of nuclear factor-kappaB. Br J Haematol 2010; 150: 543–553.
Chiron D, Bekeredjian-Ding I, Pellat-Deceunynck C, Bataille R, Jego G . Toll-like receptors: lessons to learn from normal and malignant human B cells. Blood 2008; 112: 2205–2213.
Ueda S, Nakamura H, Masutani H, Sasada T, Yonehara S, Takabayashi A et al. Redox regulation of caspase-3(-like) protease activity: regulatory roles of thioredoxin and cytochrome c. J Immunol 1998; 161: 6689–6695.
Abdi J, Engels F, Garssen J, Redegeld FA . Toll-like receptor-9 triggering modulates expression of alpha-4 integrin on human B lymphocytes and their adhesion to extracellular matrix proteins. Exp Hematol 2011; 39: 927–933.
Saha MN, Jiang H, Jayakar J, Reece D, Branch DR, Chang H . MDM2 antagonist nutlin plus proteasome inhibitor velcade combination displays a synergistic anti-myeloma activity. Cancer Biol Ther 2010; 9: 936–944.
Neri S, Mariani E, Meneghetti A, Cattini L, Facchini A . Calcein-acetyoxymethyl cytotoxicity assay: standardization of a method allowing additional analyses on recovered effector cells and supernatants. Clin Diagn Lab Immunol 2001; 8: 1131–1135.
de Heer P, de Bruin EC, Klein-Kranenbarg E, Aalbers RI, Marijnen CA, Putter H et al. Caspase-3 activity predicts local recurrence in rectal cancer. Clin Cancer Res 2007; 13: 5810–5815.
Puszynski K, Bertolusso R, Lipniacki T . Crosstalk between p53 and nuclear factor-B systems: pro- and anti-apoptotic functions of NF-B. IET Syst Biol 2009; 3: 356–367.
Schneider G, Henrich A, Greiner G, Wolf V, Lovas A, Wieczorek M et al. Cross talk between stimulated NF-kappaB and the tumor suppressor p53. Oncogene 2010; 29: 2795–2806.
Kawai T, Akira S . Signaling to NF-kappaB by Toll-like receptors. Trends Mol Med 2007; 13: 460–469.
Kagawa K, Inoue T, Tokino T, Nakamura Y, Akiyama T . Overexpression of GML promotes radiation-induced cell cycle arrest and apoptosis. Biochem Biophys Res Commun 1997; 241: 481–485.
Kimura Y, Furuhata T, Shiratsuchi T, Nishimori H, Hirata K, Nakamura Y et al. GML sensitizes cancer cells to Taxol by induction of apoptosis. Oncogene 1997; 15: 1369–1374.
Nakamura Y . Isolation of p53-target genes and their functional analysis. Cancer Sci 2004; 95: 7–11.
Takahashi T, Suzuki M, Shigematsu H, Shivapurkar N, Echebiri C, Nomura M et al. Aberrant methylation of Reprimo in human malignancies. Int J Cancer 2005; 115: 503–510.
Xenaki G, Ontikatze T, Rajendran R, Stratford IJ, Dive C, Krstic-Demonacos M et al. PCAF is an HIF-1alpha cofactor that regulates p53 transcriptional activity in hypoxia. Oncogene 2008; 27: 5785–5796.
Jin Y, Zeng SX, Dai MS, Yang XJ, Lu H . MDM2 inhibits PCAF (p300/CREB-binding protein-associated factor)-mediated p53 acetylation. J Biol Chem 2002; 277: 30838–30843.
Youle RJ, Strasser A . The BCL-2 protein family: opposing activities that mediate cell death. Nat Rev Mol Cell Biol 2008; 9: 47–59.
Zhivotovsky B, Kroemer G . Apoptosis and genomic instability. Nat Rev Mol Cell Biol 2004; 5: 752–762.
Voss OH, Kim S, Wewers MD, Doseff AI . Regulation of monocyte apoptosis by the protein kinase C delta-dependent phosphorylation of caspase-3. J Biol Chem 2005; 280: 17371–17379.
Tang CH, Hsu CJ, Fong YC . The CCL5/CCR5 axis promotes interleukin-6 production in human synovial fibroblasts. Arthritis Rheum 2010; 62: 3615–3624.
Zeigler MM, Doseff AI, Galloway MF, Opalek JM, Nowicki PT, Zweier JL et al. Presentation of nitric oxide regulates monocyte survival through effects on caspase-9 and caspase-3 activation. J Biol Chem 2003; 278: 12894–12902.
Tang CH, Hsu CJ, Yang WH, Fong YC . Lipoteichoic acid enhances IL-6 production in human synovial fibroblasts via TLR2 receptor, PKCdelta and c-Src dependent pathways. Biochem Pharmacol 2010; 79: 1648–1657.
Nair P, Muthukkumar S, Sells SF, Han SS, Sukhatme VP, Rangnekar VM . Early growth response-1-dependent apoptosis is mediated by p53. J Biol Chem 1997; 272: 20131–20138.
Lohr K, Moritz C, Contente A, Dobbelstein M . p21/CDKN1A mediates negative regulation of transcription by p53. J Biol Chem 2003; 278: 32507–32516.
Chen L, Wang S, Zhou Y, Wu X, Entin I, Epstein J et al. Identification of early growth response protein 1 (EGR-1) as a novel target for JUN-induced apoptosis in multiple myeloma. Blood 2010; 115: 61–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Blood Cancer Journal website
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Abdi, J., Mutis, T., Garssen, J. et al. Stimulation of Toll-like receptor-1/2 combined with Velcade increases cytotoxicity to human multiple myeloma cells. Blood Cancer Journal 3, e119 (2013). https://doi.org/10.1038/bcj.2013.17
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2013.17
Keywords
This article is cited by
-
Combination therapy with proteasome inhibitors and TLR agonists enhances tumour cell death and IL-1β production
Cell Death & Disease (2018)
-
Cell adhesion down-regulates the expression of vacuolar protein sorting 4B (VPS4B) and contributes to drug resistance in multiple myeloma cells
International Journal of Hematology (2015)