Abstract
Objectives:
To assess the implications of variation in Metabolic Syndrome (MS) definition (biochemical and anthropometric indicators) on MS prevalence estimates in a population of overweight and mildly obese children.
Design:
Cross-sectional study.
Subjects:
Ninety-nine (64 girls) overweight or mildly obese, but otherwise healthy, pre-pubertal 6–9-year olds recruited for a randomized controlled trial of weight management.
Measures:
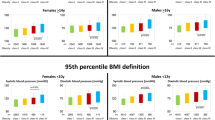
Height, weight and waist circumference were measured with BMI and waist z-scores calculated. Fasting cholesterol and fractions, glucose and insulin were measured, together with systolic and diastolic blood pressure (BP). Anthropometric and metabolic indicators were classified as normal or elevated using adult- or child-specific cut points with clustering of MS indicators also assessed using two adult and three child-specific definitions.
Results:
A total of 0–4% of subjects were classified with MS when adult definitions were applied. This increased to between 39 and 60% using child-specific definitions, varying according to whether hyperinsulinaemia was central to the MS classification. Systolic BP, triglycerides, total cholesterol, high-density lipoprotein cholesterol and waist z-score increased across insulin quartiles (P<0.05). The use of body mass index and waist circumference in the MS definition classified the same subjects.
Conclusions:
The classification of MS in children depends strongly on the definition chosen, with MS prevalence estimates higher if insulin is part of the definition and child-specific cut points for metabolic indicators are used. Hyperinsulinaemia and MS are common consequences of childhood obesity but they are not commonly part of the assessment or management plan for weight management in children. There is a need for the establishment of normal insulin ranges and consistent definition of MS in childhood and adolescence.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Chinn S, Rona RJ . Prevalence and trends in overweight and obesity in three cross sectional studies of British children, 1974–94. BMJ 2001; 322: 24–26.
Flegal KM, Troiano RP . Changes in the distribution of body mass index of adults and children in the US population. Int J Obes Relat Metab Disord 2000; 24: 807–808.
Magarey AM, Daniels LA, Boulton TJC . Prevalence of overweight and obesity in Australian children and adolescents. Assessment of 1985 and 1995 data against new standard worldwide definitions. Med J Aust 2001; 174: 561–564.
Pinhas-Hamiel O, Dolan LM, Daniles SR, Standiford D, Khoury P, Zeitler P . Increased incidence of non-insulin dependent diabetes mellitus among adolescents. J Paediatr 1996; 128: 608–615.
Freedman DS, Dietz WH, Srinivasan SR, Berenson GS . The relation of cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Paediatrics 1999; 103: 1175–1182.
Grundy SM, Brewer HB, Cleeman JI, Smith SC, Lenfant C for the National Heart, Lung, and Blood Institute/American Heart Association. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004; 109: 433–438.
Chen W, Srinivasan SR, Elkasabany A, Berenson GS . The association of cardiovascular risk factor clustering related to insulin resistance syndrome (Syndrome X) between young parents and their offspring: the Bogalusa Heart Study. Atherosclerosis 1999; 145: 197–205.
Maffeis C, Moghetti P, Grezzani A, Clementi M, Gaudino R, Tato L . Insulin resistance and the persistance of obesity from childhood into adulthood. J Clin Endicrinol Metab 2002; 87: 71–76.
Sinaiko AR, Jacobs DR, Steinberger J, Moran A, Luepker R, Rocchini AP et al. Insulin resistance syndrome in childhood: associations of the euglycemic insulin clamp and fasting insulin with fatness and other risk factors. J Pediatr 2001; 139: 700–707.
Balkau B, Charles M . Comments on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance. Diabetic Medicine 1999; 16: 442–443.
NIH. Third report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). National Institutes of Health: Bethesda, MD, 2001.
WHO. Report of a WHO consultation: definition of metabolic syndrome in definition, diagnosis, and classification of diabetes mellitus and its complications. I. Diagnosis and classification of diabetes mellitus. WHO, Department of Noncommunicable Disease Surveillance: Geneva, 1999.
Chen W, Srinivasan SR, Elkasabany A, Berenson GS . Cardiovascular risk factors clustering features of insulin resistance syndrome (Syndrome X) in a biracial (Black-White) population of children, adolescents, and young adults: the Bogalusa Heart Study. Am J Epidemiol 1999; 150: 667–674.
Raitakari OT, Porkka KV, Ronnemaa T, Knip M, Uhari M, Akerblom HK et al. The role of insulin in clustering of serum lipids and blood pressure in children and adolescents. The Cardiovascular Risk in Young Finns Study. Diabetologia 1995; 38: 1042–1050.
Lambert M, Paradis G, O'Loughlin J, Delvin EE, Hanley JA, Levy E . Insulin resistance syndrome in a representative sample of children and adolescents from Quebec, Canada. Int J Obes Relat Metab Disord 2004; 28: 833–841.
Weiss R, Dziura J, Burgert TS, Tamborlane WV, Takasali SE, Yeckel CW et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med 2004; 350: 2362–2374.
Rodriguez-Moran M, Salazar-Vazquez B, Violante R, Guerrero-Rmero F . Metabolic Syndrome among children and adolescents aged 10–18 years. Diabetes Care 2004; 27: 2516–2517.
Misra A, Vikram N, Arya S, Pandey RM, Dhingra V, Chatterjee A et al. High prevalence of insulin resistance in postpubertal Asian Indian children is associated with adverse truncal body fat patterning, abdominal adiposity and excess body fat. Int J Obes Relat Metab Disord 2004; 28: 1217–1226.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1–6.
Cole TJ, Freeman JV, Preece MA . Body mass index reference curves for the UK, 1990. Arch Diseases of Children 1995; 73: 25–29.
Tanner J . Growth at Adolescence: with a general consideration of the effects of hereditary and environmental factors upon growth and maturation from birth to maturity (2nd edn). Oxford: Blackwell Scientific Publications, 1962.
Jureidini KF, Baghurst PA, Hogg RJ, Van Renen MJ, Adams PS, Burnell RH et al. Blood pressure in schoolchildren measured under standardized conditions. Med J Aust 1988; 149: 132–134.
Goodman E, Daniels SR, Morrison JA, Huang B, Dolan LM . Contrasting prevalence of and demographic disparities in the World Health Organization and National Cholesterol Education Program Adult Treatment Panel III definitions of metabolic syndrome among adolescents. J Pediatr 2004; 145: 445–451.
Anonymous. Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: a working group report from the National High Blood Pressure Education Program. Paediatrics 1996; 98: 649–658.
NCEP. National Cholesterol Education Program (NCEP): highlights of the report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Paediatrics 1992; 89: 495–501.
McCarthy HD, Ellis SM, Cole TJ . Central overweight and obesity in British youth aged 11–16 years: cross sectional surveys of waist circumference. BMJ 2003; 326: 624–627.
McCarthy HD, Jarrett KV, Crawley HF . The development of waist circumference percentiles in British children aged 5.0–16.9 y. Eur J Clin Nutr 2001; 55: 902–907.
Duncan G, Li S, Zhou X-H . Prevalence and trends of a Metabolic Syndrome phenotype among US adolescents, 1999-2000. Diabetes Care 2004; 27: 2438–2443.
Viner RM, Segal TY, Lichtarowicz-Krynska E, Hindmarsh P . Prevalence of the insulin resistance syndrome in obesity. Arch Dis Child 2005; 90: 10–14.
Savva SC, Tornaritis M, Savva ME, Kourides Y, Panagi A, Silikiotou N et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obes Relat Metab Disord 2000; 107: 1453–1458.
Higgins PB, Gower BA, Hunter GR, Goran MI . Defining health-related obesity in prepubertal children. Obesity Res 2001; 9: 233–240.
NHMRC. Clinical Practice Guidelines for the Management of Overweight and Obesity in Children and Adolescents. Commonwealth of Australia: Canberra, 2003.
Ebbeling CB, Leidig MM, Sinclair KB, Hangen JP, Ludwig DS . A reduced-glycemic load diet in the treatment of adolescent obesity. Arch Pediatr Adolesc Med 2003; 157: 773–779.
Lambert M, Delvin EE, Paradis G, O'Loughlin J, Levy E . C-reactive protein and features of the metabolic syndrome in a population-based sample of children and adolescents. Clin Chem 2004; 50: 1762–1768.
Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, Criqui M et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the CDC and AHA. Circulation 2003; 170: 499–511.
Bacha F, Saad R, Gungor N, Janosky J, Arslanian SA . Obesity, regional fat distribution and syndrome X in obese black versus white adolescents: race differential in diabetogenic and atherogenic risk factors. J Clin Endo Metab 2003; 88: 2534–2540.
Mehta S, Mahajan D, Steinbeck K, Bermingham MA . Relationship between measures of fatness, ethnicity and lipids in a cohort of adolescent boys. Ann Nutr Metab 2002; 46: 192–199.
Acknowledgements
This research was carried out at the Department of Nutrition and Dietetics, Flinders University, Adelaide, Australia and was funded by the Australian Health Management Group Assistance to Health and Medical Research Fund. Rebecca Golley is supported by an Australian National Health and Medical Research Council Postgraduate Research Scholarship (No. 229978). We thank the children and their families for participating in the study including blood sample collection. We thank Ms Sarah Garnett, Institute of Endocrinology, The Children's Hospital at Westmead and Ms Margie Gruca, Lab Manager James Fairfax Institute Paediatric Nutrition, The Children's Hospital at Westmead for calculation of waist circumference z-scores; Division of Laboratory Medicine, Women's and Children's Hospital, Adelaide; and Diagnostic Laboratory, Department of Endocrinology Royal Prince Alfred Hospital (RPAH), Sydney for assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Golley, R., Magarey, A., Steinbeck, K. et al. Comparison of metabolic syndrome prevalence using six different definitions in overweight pre-pubertal children enrolled in a weight management study. Int J Obes 30, 853–860 (2006). https://doi.org/10.1038/sj.ijo.0803195
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803195
Keywords
This article is cited by
-
Effect of cardiometabolic risk factors on the relationship between adiposity and bone mass in girls
International Journal of Obesity (2018)
-
Prevalence of metabolic syndrome in children aged 5-9 years from southwest colombia: a cross-sectional study
World Journal of Pediatrics (2016)
-
Epicardial adipose tissue and signs of metabolic syndrome in children
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2016)
-
Metabolic Syndrome: A Construct with Limited Relevance to Children
Current Cardiovascular Risk Reports (2014)
-
Waist circumference percentiles among Turkish children under the age of 6 years
European Journal of Pediatrics (2013)