Abstract
In uncomplicated pregnancies, first trimester androgen, oestrogen and prolactin concentrations were higher in nulliparous (n=160) than parous (n=260) mothers. Androgens and estrogens were higher in younger than older mothers. These data are consistent with elevated hormone concentrations mediating the breast cancer protection from a first pregnancy and pregnancies occurring at younger ages.
Similar content being viewed by others
Main
There are few opportunities to directly evaluate the hypothesis that the pregnancy hormonal milieu influences cancer risk in the mother and offspring. Investigations have instead used proxies to reflect the endocrine environment such as birth weight which is associated with a modestly elevated breast cancer risk in the daughter (Michels and Xue, 2006). Whereas age at first and last pregnancy and parity are established maternal breast cancer risk factors (National Cancer Institute, 2003), associations have been less consistent for other pregnancy characteristics with regard to the mother (Cnattingius et al, 2005) and offspring (Potischman et al, 2004).
The few studies on hormone variations by maternal and pregnancy characteristics have focused on maternal measures in mid- or late pregnancy, primarily estrogens. Because the timing of carcinogenic events is unknown, characterising hormones over the entire pregnancy may provide additional insights into the biological mechanisms for maternal and perinatal breast cancer risk factors.
Materials and methods
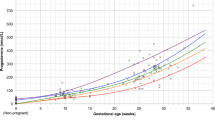
Data derived from an obstetrical study at the Massachusetts General Hospital (MGH) in Boston, Massachusetts that began in 1998 (Thadhani et al, 2001). Women were recruited at their first prenatal visit (ranging from 6.4 to 19.9 weeks gestation (median 11) with over 90% in the first 13 weeks), interviewed, and asked to provide a blood sample. Participants gave informed consent and the study was approved by the MGH Institutional Review Board.
The study sample, described previously (Potischman et al, 2005), includes 109 Hispanic, 56 African American and 255 Caucasian women 18–42 years of age (median 29.6), who delivered a live, singleton birth in an uncomplicated pregnancy. A total of 38% of the women were nulliparous.
Laboratory assays
Sample handling, storage and assays were described previously (Potischman et al, 2005). Intra-class correlation coefficients from repeated measures of blind quality control samples were 97% for oestradiol, 92% for SHBG, 90% for oestrone, 85% for androstenedione, 76% for prolactin, 76% for testosterone, 60% for progesterone and <50% for DHEAS. Hormone medians and ranges have been published (Potischman et al, 2005).
Statistical methods
Spearman correlation coefficients were calculated using continuous data. All pregnancy factors associated with the hormones in unadjusted analyses were entered with gestational age at blood collection (excluding pregnancies with 14+ weeks' gestation) into linear regression models with logarithm-transformed hormones as dependent variables. Exponentiated β estimates (−1.0) from these models are presented for factors which remained significantly associated with the hormones, or changed <10% from the unadjusted models. Interactions between maternal age (<30, 30+ years) and parity (nulliparous, parous) were tested by including the main effects and cross-product terms in a regression model. Additional interactions between all pregnancy factors and hormones by offspring sex and race were evaluated. Statistical significance was defined as P<0.05.
Results
Gestational age at blood collection was inversely correlated with the androgens and positively correlated with the estrogens, progesterone, prolactin and SHBG (Table 1). Correlations with first trimester hormones were demonstrated for maternal age, weight and BMI, but not maternal height or birth weight.
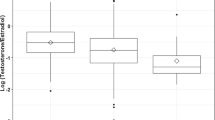
In analyses mutually adjusted for the pregnancy factors and including gestational age, androgen and oestrogen concentrations were lower in older mothers (Table 2); the greatest incremental difference was between those <30 and 30+ years (e.g., P<0.001 for androstenedione; other data not shown). In contrast, maternal age was positively associated with progesterone. The androgens, estrogens and prolactin were higher in the 160 nulliparous than in the 260 parous women. Maternal BMI (and maternal weight; data not shown) was positively associated with the androgens and inversely associated with progesterone and SHBG, and maternal height was inversely associated with the estrogens and SHBG though not with the other hormones. Current smokers had lower progesterone and prolactin concentrations, whereas alcohol users had lower oestradiol only.
The positive association of maternal BMI and androstenedione was limited to mothers of female fetuses (P=0.01); there were no other interactions by offspring sex. Differences in hormones by race/ethnicity were reported in an earlier paper from this study (Potischman et al, 2005). The associations between the pregnancy factors and hormones were similar with adjustment for race/ethnicity and there were no meaningful interactions demonstrated (data not shown).
Except for progesterone, the highest hormone concentrations were generally observed in nulliparous women less than age 30 years and the lowest concentrations in parous women age 30 years and over although none of the interactions were significant (P ranged from 0.36 for SHBG to 0.79 for prolactin). In contrast, nulliparous women age 30+ years had higher progesterone concentrations than younger nulliparous women or parous women of any age (P for interaction=0.006).
Discussion
There are few previous data characterising hormone variations in the first trimester. Our results for first compared with subsequent full-term pregnancies confirm previous findings of higher oestradiol (Bernstein et al, 1986), while also demonstrating elevations in androgens and prolactin. We had limited power to assess reported oestrogen differences by smoking status (Bernstein et al, 1989), thus the lower progesterone and prolactin concentrations we observed among smokers may be noteworthy.
Birth weight, an established prenatal breast cancer risk factor (Michels and Xue, 2006), is hypothesised to be mediated by foetal oestrogen exposure (Michels et al, 1996). Third trimester maternal oestriol is elevated in high birth weight pregnancies (Kaijser et al, 2000; Mucci et al, 2003; Peck et al, 2003; Troisi et al, 2003; Nagata et al, 2006), but data for second trimester estrogens are conflicting (Kaijser et al, 2000; Wuu et al, 2002). Our data show no association of birth weight with first trimester estrogens seeming to suggest that if oestrogen explains the association of birth weight and breast cancer risk, the critical exposure window may be later in pregnancy. Yet associations of birth weight with cord estrogens are unclear (Simmons et al, 1994; Shibata et al, 2002; Troisi et al, 2003; Nagata et al, 2006), and breast cancer risk in women prenatally exposed to diethylstilbestrol does not differ by trimester of first exposure (Palmer et al, 2006). Other prenatal factors could act differently. For example, a more pronounced breast cancer risk is suggested for women who were in utero during the Dutch famine in early compared with later gestation (Painter et al, 2006).
Long-term maternal breast cancer risk is reduced with a full-term pregnancy, particularly when it occurs at a young age (National Cancer Institute, 2003). Epidemiologic data indicate protection increases with gestational length (Vatten et al, 2002), suggesting that the important hormonal events must occur late in pregnancy. However, protection from a full-term pregnancy would also be consistent with cumulative dose effects of specific hormones throughout the pregnancy, or early hormonal events which require the subsequent action of others to induce the relevant molecular changes. Descriptive data characterising the hormonal profile of the entire pregnancy are lacking with regard to parity. The elevated first trimester oestradiol we observed in first compared with subsequent pregnancies has also been shown for the second (Wuu et al, 2002; Arslan et al, 2006) and early third trimesters (Wuu et al, 2002), but perhaps not at delivery (Troisi et al, 2003). The elevated prolactin concentrations in our data for first pregnancies have also been noted in the second trimester (Xu et al, 2003; Arslan et al, 2006), but not later in the pregnancy (Xu et al, 2003), and the first trimester androgen elevations have not been shown at delivery (Troisi et al, 2003). Our data also indicate that oestrogen and androgen concentrations are higher in pregnancies that occur in younger than in older women. There is limited and conflicting information for maternal estrogens by age at any point during the pregnancy (Panagiotopoulou et al, 1990; Kaijser et al, 2002; Troisi et al, 2003), whereas the androgen findings are consistent with studies using measurements made later in the pregnancy (Carlsen et al, 2003; Troisi et al, 2003).
The explanation for the protective effect of a first pregnancy and the inverse relationship of this protection with the age at which the pregnancy occurs remains speculative. The hypothesis most commonly invoked is that irreversible molecular changes (driven by hormonal exposures) to the breast that prevent tumour initiation (Medina, 2005) must occur early in life to precede the initial stage of breast carcinogenesis, and that most of these changes occur with the first pregnancy. An alternative explanation, however, is that the operative hormonal influences may be different in first pregnancies, particularly those occurring at young ages. Our finding of higher circulating estrogens, androgens and prolactin in both a first pregnancy and, independently, in those occurring at younger ages could be consistent with this latter explanation. Subsequently reduced concentrations of these hormones in the pregnant and non-pregnant state may also be involved.
The study subjects were participants in a health care plan that provides prenatal care. The MGH study's participation rate is high and thus unlikely to represent an unusual population of women who seek medical care early in pregnancy. Whereas the reproducibility data were high for oestradiol and oestrone, there was substantial laboratory imprecision for other analytes that based on the quality control data suggested sporadic, random measurement errors. Finally, it is unknown how well a single first trimester hormone measurement represents early pregnancy exposure.
Our data suggest that birth weight is not a marker of early pregnancy hormonal exposure, and that if hormones mediate any of the birth weight and breast cancer association the effect is likely to occur later in the pregnancy. Elevated first trimester oestrogen, androgen and prolactin concentrations in first full-term pregnancies, and elevated oestrogen, androgen and progesterone concentrations in pregnancies occurring at younger ages may be consistent with these hormones acting to reduce later breast cancer risk.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Arslan AA, Zeleniuch-Jacquotte A, Lukanova A, Afanasyeva Y, Katz J, Levitz M, Del Priore G, Toniolo P (2006) Effects of parity on pregnancy hormonal profiles across ethnic groups with a diverse incidence of breast cancer. Cancer Epidemiol Biomarkers Prev 15: 2123–2130
Bernstein L, Depue RH, Ross RK, Judd HL, Pike MC, Henderson BE (1986) Higher maternal levels of free estradiol in first compared to second pregnancy: early gestational differences. J Natl Cancer Inst 76: 1035–1039
Bernstein L, Pike MC, Lobo RA, Depue RH, Ross RK, Henderson BE (1989) Cigarette smoking in pregnancy results in marked decrease in maternal hCG and oestradiol levels. Br J Obstet Gynaecol 96: 92–96
Carlsen SM, Jacobsen G, Bjerve KS (2003) Androgen levels in pregnant women decrease with increasing maternal age. Scand J Clin Lab Invest 63: 23–26
Cnattingius S, Torrång A, Ekbom A, Granath F, Petersson G, Lambe M (2005) Pregnancy characteristics and maternal risk of breast cancer. JAMA 294: 2474–2480
Kaijser M, Granath F, Jacobsen G, Cnattingius S, Ekbom A (2000) Maternal pregnancy estriol levels in relation to anamnestic and fetal anthropometric data. Epidemiology 11: 315–319
Kaijser M, Jacobsen G, Granath F, Cnattingius C, Ekbom A (2002) Maternal age, anthropometrics and pregnancy oestriol. Paediatric Perinatal Epidemiol 16: 149–153
Medina D (2005) Mammary developmental fate and breast cancer risk. Endocr Relat Cancer 12: 483–495
Michels KB, Trichopoulos D, Robins JM, Rosner BA, Manson JE, Hunter DJ, Colditz GA, Hankinson SE, Speizer FE, Willett WC (1996) Birthweight as a risk factor for breast cancer. Lancet 348: 1542–1546
Michels KB, Xue F (2006) Role of birthweight in the etiology of breast cancer. Int J Cancer 119: 2007–2025
Mucci LA, Lagiou P, Tamimi RM, Hsieh C-C, Adami H-O, Trichopoulos D (2003) Pregnancy estriol, estradiol, progesterone and prolactin in relation to birth weight and other birth size variables (United States). Cancer Causes Control 14: 311–318
Nagata C, Iwasa S, Shiraki M, Shimizu H (2006) Estrogen and α-fetoprotein levels in maternal and umbilical cord blood samples in relation to birth weight. Cancer Epidemiol Biomarkers Prev 15: 1469–1472
National Cancer Institute (2003) Summary report: early reproductive events and breast cancer workshop. (http://cancer.gov/cancerinfo/ereworkshop-report)
Painter RC, De Rooij SR, Bossuyt PMM, Osmond C, Barker DJ, Bleker OP, Roseboom TJ (2006) A possible link between prenatal exposure to famine and breast cancer: a preliminary study. Am J Hum Biol 18: 853–856
Palmer JR, Wise LA, Hatch EE, Troisi R, Titus-Ernstoff L, Strohsnitter W, Kaufman R, Herbst AL, Noller KL, Hyer M, Hoover RN (2006) Prenatal diethylstilbestrol exposure and risk of breast cancer. Cancer Epidemiol Biomark Prev 15: 1509–1514
Panagiotopoulou K, Katsouyanni K, Petridou E, Garas Y, Tzonou A, Trichopoulos D (1990) Maternal age, parity, and pregnancy estrogens. Cancer Causes Control 1: 119–124
Peck JD, Hulka BS, Savitz DA, Baird D, Poole C, Richardson BE (2003) Accuracy of fetal growth indicators as surrogate measures of steroid hormone levels during pregnancy. Am J Epidemiol 157: 258–266
Potischman N, Troisi R, Thadhani R, Hoover RN, Dodd K, Davis WW, Sluss PM, Hsieh CC, Ballard-Barbash R (2005) Pregnancy hormone concentrations across ethnic groups: implications for later cancer risk. Cancer Epidemiol Biomarkers Prev 14: 1514–1520
Potischman N, Troisi R, Vatten L (2004) The life course approach to cancer epidemiology. In A Life Course Approach to Chronic Disease Epidemiology, Kuh D, Ben-Shlomo Y (eds) 2nd edn, pp 260–280. Oxford University Press: New York
Simmons D, France JT, Keelan JA, Song L, Knox BS (1994) Sex differences in umbilical cord serum levels of inhibin, testosterone, oestradiol, dehydroepiandrosterone sulphate, and sex hormone-binding globulin in human term neonates. Biol Neonate 65: 287–294
Shibata A, Harris DT, Billings PR (2002) Concentrations of estrogens and IGFs in umbilical cord blood plasma: a comparison among Caucasian, Hispanic, and Asian-American females. J Clin Endocrinol Metab 87: 810–815
Thadhani R, Ecker JL, Kettyle E, Sandler L, Frigoletto FD (2001) Pulse pressure and risk of preeclampsia: a prospective study. Obstet Gynecol 97: 515–520
Troisi R, Potischman N, Roberts JM, Siiteri P, Hoover RN (2003) Associations of maternal and umbilical cord hormone concentrations with maternal, gestational and neonatal factors. Cancer Causes Control 14: 347–355
Vatten LJ, Romundstad PR, Trichopoulos D, Skjærven R (2002) Pregnancy related protection against breast cancer depends on length of gestation. Br J Cancer 87: 289–290
Wuu J, Hellerstein S, Lipworth L, Wide L, Xu B, Yu GP, Kuper H, Lagiou P, Hankinson SE, Ekbom A, Carlström K, Trichopoulos D, Adami HO, Hsieh CC (2002) Correlates of pregnancy oestrogen, progesterone and sex hormone-binding globulin in the USA and China. Eur J Cancer Prev 11: 283–293
Xu B, Lipworth L, Wide L, Wuu J, Yu SZ, Lagiou P, Kuper H, Hankinson SE, Carlström K, Adami HO, Trichopoulos D, Hsieh CC (2003) Maternal and gestational correlates of pregnancy prolactin and growth hormone in USA and China. Eur J Cancer Prev 12: 35–42
Acknowledgements
The Divisions of Cancer Epidemiology and Genetics and Cancer Control and Population Sciences, National Cancer Institute, National Institutes of Health, US Department of Health and Human Services provided funding for the hormone assays, data analysis and article preparation. HD 39223 provided funding for the collection of original data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Troisi, R., Hoover, R., Thadhani, R. et al. Maternal, prenatal and perinatal characteristics and first trimester maternal serum hormone concentrations. Br J Cancer 99, 1161–1164 (2008). https://doi.org/10.1038/sj.bjc.6604639
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604639
Keywords
This article is cited by
-
Pregnancy-related risk factors for sex cord-stromal tumours and germ cell tumours in parous women: a registry-based study
British Journal of Cancer (2020)
-
Urinary mycoestrogens and age and height at menarche in New Jersey girls
Environmental Health (2019)
-
Predictors of Steroid Hormone Concentrations in Early Pregnancy: Results from a Multi-Center Cohort
Maternal and Child Health Journal (2019)
-
Hormone concentrations throughout uncomplicated pregnancies: a longitudinal study
BMC Pregnancy and Childbirth (2016)
-
Early life factors and adult mammographic density
Cancer Causes & Control (2013)