Key Points
-
Root filled teeth are often compromised by incomplete root formation, secondary caries around posts, inappropriate post space preparation, and internal resorption.
-
Traditional methods of restoration using metal posts and pins are often unsatisfactory.
-
Instead of waiting for the formation of a calcific bridge during apexification, mineral trioxide aggregate can be placed as an immediate apical seal.
-
Weakened roots can be reinforced using dentine bonding agents, composite resin and quartz-fibre posts.
Key Points
Restoration of the endodontically treated tooth
-
1
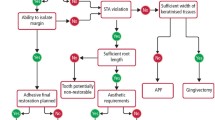
Restoration of the root-filled tooth: pre-operative assessment
-
2
Tooth preparation for post-retained restorations
-
3
Post and core systems, refinements to tooth preparation and cementation
-
4
Weakened anterior roots – intraradicular rehabilitation
Abstract
This paper highlights the fact that many anterior teeth requiring restoration are severely weakened having wide, flared canal spaces, and thin dentinal walls that are prone to fracture. Traditionally these teeth have been restored using metal posts and are often unsuccessful because of lack of retention or root fracture. This paper describes how mineral trioxide aggregate (MTA) can be used to form an immediate apical seal rather than waiting months for apexification. Weakened roots can be reinforced using dentine bonding agents and composite resin and if insufficient coronal tooth structure is present a quartz-fibre post can be placed to retain a composite core.
Similar content being viewed by others
Introduction
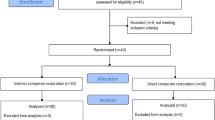
The majority of endodontically treated single-rooted teeth with a lack of coronal tooth structure can be restored using posts and cores and the techniques described in this series of papers. However, many anterior teeth that require post-retained restorations are severely weakened as a result of recurrent caries extending into the radicular dentine around pre-existing posts or the fact that the pulp has become necrotic prior to the completion of root formation in a young patient (Figs 1 and 2 respectively). Other, less-common conditions include developmental anomalies such as fusion and germination, internal resorption, and iatrogenic damage resulting in large access preparations.1 The resulting large, flared root canals have thin dentinal walls leaving them too weak to withstand normal masticatory forces and prone to fracture as a result.2 Such teeth may also lack sufficient coronal tooth structure and pose a problem to the restorative dentist.
These compromised teeth are difficult to restore for a variety of reasons. Restoration with cast metal posts can cause wedging forces coronally that may result in irreversible failure because of fracture of an already weakened root.3,4 The geometry of the flared canal also results in a very wide, tapered and unretentive post. In these situations, if a prefabricated post is used, the excess space within the root canal would be taken up with a bulk of luting cement. This results in a potentially weak area in the restoration.1 Placement of dentine pins to help retain the core is also not feasible because there is likely to be insufficient dentine present at the coronal portion of the root.5 Thus, these traditional methods of restoration are unsatisfactory and often result in extraction of the tooth. In a child patient this can mean wearing a partial denture until the time when options such as bridges or implants can be considered. This paper therefore describes the development of an alternative technique that has been successfully implemented for the treatment of such teeth.
Apical seal
Irrespective of the aetiology of the weakened root, emphasis should also be placed on achieving an apical seal during root canal treatment. Teeth that require intraradicular reinforcement are frequently accompanied by a large communication between the root canal and the periodontal ligament. This classically happens, for example, when a large root canal has been over-prepared apically, leading to damage to the apical constriction and loss of an apical stop for conventional obturation (Fig. 3). Conventional root canal treatment is also unsuitable for the treatment of non-vital, permanent teeth with wide open immature apicies, as it is impossible to achieve an apical hard tissue barrier against which a root canal filling can be compacted (Fig. 2).6
Apexification
Apexification is a technique that induces apical closure by the formation of mineralised tissue. Once this barrier has been established the root canal can be obturated with thermoplastic gutta-percha. Calcium hydroxide in the form a non-setting aqueous suspension has been recommended as the material of choice for this treatment.7 Although it is still not clear how calcium hydroxide induces the formation of the calcific bridge, it has been suggested that this is the result of a high pH, the presence of calcium and hydroxyl ions, and its antibacterial properties. What is known is that it prevents the ingress of granulation tissue into the root canal and inhibits periradicular osteoclastic activity. Prior to placement of the calcium hydroxide it is essential that the root canal is thoroughly cleaned of all necrotic debris and bacteria. The root canal must be completely filled with calcium hydroxide to ensure that the material is in contact with the periapical tissues otherwise a calcific barrier may not occur, or occur at a more coronal level.8
This widely accepted technique has its disadvantages including the fact that the calcium hydroxide paste must be changed every three to six months until a calcific barrier can be detected.6,8 The time taken for closure is variable, ranging from five to 19 months.9 This requires multiple visits over a long period of time, which some younger patients may find inconvenient. Despite this, the success rate of apexification has been reported as 74–96%.9,10,11 It has been suggested by some authors that an apical barrier will form quicker in cases where the calcium hydroxide is changed more often,8 while others believe that this may in fact disturb the mineralisation process.9 According to Ghose et al. (1987)9 and Kleier and Barr (1991)6 the rate of closure does not appear to be related to the size of the apical opening. Closure may not happen at all in cases that have suffered displacement injuries7 or when a periapical abscess develops.8 Undiagnosed horizontal or vertical root fractures may also prevent successful treatment.6
One-visit apexification
An alternative to apexification over multiple visits has been the placement of a biocompatible material into the apical part of the root canal. The formation of an instant apical barrier allows immediate obturation of the canal space. Materials that have previously been tried are calcium phosphate ceramic,12,13,14 surgicel with amalgam,15 freeze-dried cortical bone,16 freeze-dried dentine17 and dentinal shavings.18,19 However, these have been largely experimental and are not commonly used.
Mineral trioxide aggregate (MTA, ProRoot, Dentsply Tulsa Dental, Tulsa OK) (Fig. 4), is a relatively new dental material that has been recommended for use in endodontic procedures such as root-end fillings following periradicular surgery, perforation repairs and vital pulp capping.20 Its use as an apical barrier material for root-end closure has also been described20,21,22,23,24,25,26,27,28 and Buchanan29 has also recommended the use of MTA in conventional root canal treatment to repair large apices (>0.7mm), such as those that have been over-zealously prepared during endodontic treatment, so loosing the apical constriction. The material consists of fine hydrophilic particles of tricalcium silicate, tricalcium aluminate, tricalcium oxide and silicate oxide. When mixed with sterile water it forms a colloidal gel that sets within three to four hours. In microleakage studies carried out in vitro it has been shown to be superior to IRM, SuperEBA and amalgam.30,31,32,33 It is a very biocompatible material and histological assessment carried out on Cynomolgus monkeys following periradicular surgery and root-end filling with MTA has showed no signs of periradicular inflammation.34 MTA has been shown to stimulate cytokine release35 and the production of interleukins36 which suggests that it is a bioactive material capable of promoting hard tissue formation, unlike other existing root-end filling materials. It is little surprise therefore that the production of new cementum and regeneration of the periodontal ligament over the resected root end has been reported.34
Shabahang et al. (1999)37 compared the use of MTA, osteogenic protein-1 and calcium hydroxide for apexification in dogs. The MTA formed an apical barrier more frequently than the other materials and was therefore considered an ideal material for one-visit apexification in immature teeth. The sealing ability and retention characteristics of MTA in a model of apexification was tested in an in vitro study using human, extracted, single-rooted teeth.38 Some leakage was recorded in this study, but this was thought to be as a result of the intracanal delivery technique rather than the material itself.
Clinical procedure
Placement of apical MTA plug
Teeth with open apicies require relatively large access cavities as these teeth also have large pulp horns, which can harbour necrotic, infected tissues. This debris needs to be removed and adequate access has to be gained. Under rubber dam, the root canal system can be instrumented and irrigated with sodium hypochlorite solution. However, instrumentation leads to the production of a smear layer, within which bacteria can survive. The smear layer may also block dentinal tubules and lateral accessory canals with bacterial colonies within. Thus it is beneficial to remove the smear layer by either irrigating with EDTA (17%) solution or citric acid (10%). This allows the final rinse with hypochlorite access to these previously hidden organisms.
Whilst using paper points to dry root canals in teeth with open apicies or large communications with the periodontium, it is easy to inadvertently push the paper point into the periradicular tissues causing trauma and haemorrhage. To avoid this, the use of a large paper point is recommended, measured to the correct working length. The root canal can then be dressed with a non-setting calcium hydroxide paste for a period of one to two weeks. During this period granulation tissue will form at the apex of the tooth. Calcium hydroxide paste can easily be introduced into the canal with a disposable, plastic syringe tip. It is important that the temporary restoration is durable, so that potential loss and bacterial recontamination may be prevented. With this in mind it is important that the restoration is of adequate thickness.
At the subsequent appointment, following rubber dam placement and re-access, the calcium hydroxide can easily be removed from within the root canal by irrigating with citric acid solution. Citric acid will readily dissolve the alkaline calcium hydroxide as it also acts as a chelating agent. Finally, irrigate with sodium hypochlorite and dry the canal again. The MTA can then be mixed with sterile water to a thick slurry consistency and then placed into the canal as close to the apex as possible by using a Dovgan carrier (Fig. 5). The MTA should then be condensed with a suitable instrument such as a Buchanan plugger (Fig. 6), using a gentle apical tamping technique. A rubber stop should be placed on the plugger to about 1 mm short of the working length, to ensure that the MTA is not pushed through the apex into the periradicular tissues. It is thought that an apical plug of 3–4 mm is sufficient to create a satisfactory apical seal and resist displacement (Fig. 7).38 This should then be evaluated radiographically and if the MTA appears poorly condensed it can be rinsed out with sterile water and the procedure repeated. Any traces of excess MTA on the post preparation wall can be removed with a moist paper point. A moist cotton pellet should then be placed in the remaining post space and sealed in place with an appropriate temporary restoration, until the MTA has set (four hours setting time). A moist environment was originally recommended for the setting reaction of MTA to take place, however, it is now thought that this is not necessary.
Root reinforcement
The problem in restoring weakened roots is the fact that the remaining root dentine is thin and therefore prone to fracture. Should this occur, the tooth is almost certainly unrestorable. Many of these teeth are upper incisors and in young patients the treatment options for replacement are limited. Strengthening the root in some way should help reduce the risk of fracture. Lui (1994 and 1987)1,39 described a technique of root reinforcement where the internal aspect of the thin canal walls were etched, dentine bond applied and then lined with a chemically cured composite. Following this a passive, parallel-sided, metal post was cemented in place. The disadvantage of this system was the lack of control over the polymerisation reaction of the composite placed in the apical portion of the root canal. Although it was recognised that a visible-light activated composite would allow greater time for correct placement in the root canal, the disadvantage of this material was its limited depth of cure. It is accepted that this is only 4–5 mm because of partial transmission of light through the composite. The setting of composite relies on the ability of the light to access and initiate the curing at all depths.40
In an attempt to overcome this problem, clear, plastic, light-transmitting posts (Luminex, Dentatus, Weissman Technology) were introduced that could be placed through the composite in the root canal to allow the transmission of light along its entire post length (Fig. 8).1,5,39 This permitted polymerisation of the composite resin along the entire length and circumference of the post space preparation (Fig. 9). These clear plastic posts are smooth and parallel sided except for the pointed tip. Their removal from the root canal results in a patent post space that was suitable for restoration with a size-matched, passive, parallel-sided, metal post system.1
It is recognised that the purpose of a metal post is only to retain the core and crown. It does not strengthen the tooth itself.41 Therefore the greater the composite thickness bonded to the internal aspect of the root canal the greater the potential to reinforce it. With this in mind it is recommended that a plastic post is selected that will result in a post space within the composite with a small diameter. The plastic posts are available in six diameters: 1.05 mm, 1.20 mm, 1.35 mm, 1.50 mm, 1.65 mm and 1.80 mm. The only possible disadvantage of using a smaller diameter light-transmitting post, is that it has been shown that the larger the post diameter the greater the depth of cure of the composite resin.42 However, in this laboratory study, all post sizes were shown to be capable of achieving a depth of cure exceeding 11 mm, which is a satisfactory length for most post systems.42
The manufacturers of the plastic light-transmitting posts (Luminex, Dentatus, Weissman Technology) used in these studies advocate the use of their own metal tapered post within the reinforced root. However, these are not tooth coloured and will compromise the aesthetics when an all-ceramic crown is subsequently placed. Also, parallel-sided posts have been shown to be more retentive and more effective in resisting tensile forces than tapered posts.43 A root-filled tooth reinforced in such a way as described in this paper is therefore better restored with a parallel-sided post which is sufficiently strong to support a post crown. In addition, a tooth-coloured, clear or white post which can be bonded to the composite with an adhesive resin luting cement would also be advantageous. The clinician is free to decide which post type to place within the reinforced root, but whichever one is used the post space left when the light-transmitting post is removed will require slight modification to its shape. Weakened teeth restored in this manner have been shown to be 50% more resistant to fracture than those without composite resin reinforcement.44,45
One potential problem of using composite resin within the root canal is the possibility of polymerisation shrinkage of the composite resin away from the dentinal walls towards the plastic post leaving a gap at the composite dentine interface. This can be avoided if careful attention to dentine bonding is adhered to. A suitable dentine conditioner is first required to remove the smear layer from the root canal walls. The conditioner will also open up the dentinal tubules to a depth of 4 μm. Despite the greater number of clinical stages, a three-stage system consisting of a dentine conditioner, primer and sealer has been recommended as the bond strength appears higher than with single-stage dentine bonding agents.46
Choice of post
Previous studies that have described the use of resin composite for internal rehabilitation of the root canal walls have suggested subsequent restoration with a metal post.1,5,39 Whilst favourable clinical results using this system have been reported,5 the introduction of quartz-fibre post systems and adhesive resin cements has allowed the advantages of these newer materials to be incorporated into this internal rehabilitation technique. This is particularly advantageous when there is insufficient coronal tooth tissue and a post is required to retain a tooth-coloured core and an all-ceramic crown. The obvious aesthetic advantage is the transmission of light through tooth-coloured materials in a manner similar to natural tooth structure, thus preventing the 'shine-through' effect that occurs with metal post systems. The fibre posts are also more flexible, therefore the stresses transmitted to the weakened root in function will be less, decreasing the risk of root fracture.47,48 Because quartz-fibre posts contain silica similar to the filler particles in composite resin, bonding of the post to composite using adhesive resin cement should result in high bond strength.
Clinical procedures
Internal rehabilitation of the root canal
Adequate coronal tooth structure – no post required (Fig. 10).
Non-vital tooth 21 seen in Figure 7 with adequate coronal tooth structure not requiring a post for restoration.
Once the MTA has set, the weakened root can be internally reinforced using a composite resin restorative material which will bond to the internal aspects of the root canal. Most composite resins in use today are light cured and this poses a potential problem in achieving adequate cure of the material in the apical extent of the root canal. To ensure this a light-transmitting plastic post can be used to direct light to the entire root canal (Luminex, Dentatus) (see Fig. 8).
The Luminex post system has a number of components, but only the smooth plastic light-transmitting post is required for this technique. It is important to ensure that the Luminex post is tried into the post space and is inserted to the full length of the root canal/post space preparation. A rubber stop can be placed over the post and set at the correct length. The diameter of the post should be considerably narrower than the root canal to allow an adequate volume of composite resin to surround it. Once satisfied with the selected post, the internal aspect of the root canal can be etched However, when etchant gel is placed inside the root canal it is difficult to ensure that all traces are removed at the rinsing stage. The rinsing therefore has to be thorough and any remnants of etching gel may be detected by placing paper points into the canal. This also ensures that the post space walls are dried adequately. Once this has been carried out, a suitable dentine bonding agent can be placed using a microbrush (eg Prime and Bond). Alternatively, a self-etching bonding system can be applied to the internal aspect of the root canal walls (eg PromptLPop 3M ESPE). This will eliminate the etching, rinsing and drying stages.
Once the dentine bonding agent has been placed, a restorative composite resin material is dispensed and packed into the root canal. The Luminex light-transmitting post should be lightly coated in Vaseline and inserted centrally into the root canal to its full depth (Fig. 11). Excess material is removed from the access cavity and a light-curing tip is placed at the end of the plastic post. The light will be transmitted along the entire length of the post, so polymerising the surrounding composite (see Fig. 9). The post is then removed with a rotating and pulling motion, using an instrument such as a Spencer Wells forceps (Fig. 12). The access cavity is finally restored with composite resin.
Insufficient coronal tooth structure - post required
When insufficient coronal tooth tissue remains in a single rooted tooth, a post is likely to be required to retain the core material. Some quartz-fibre posts are light transmitting (eg Luscent Anchor Posts) and can be used to direct the curing light to the entire extent of the post space as above, however, others are more opaque (ParaPost - Fibre White, Coltene Whaldent) and will not result in complete cure of the composite resin. In this case the root is reinforced as before using the Luminex light-transmitting plastic post (Figs 13 and 14). Removal of the plastic post leaves a reinforced root with a patent post channel. A quartz-fibre system can then be selected and the appropriate twist drill chosen to modify the post space. A slightly larger diameter twist drill is therefore required which also effectively removes any residues of Vaseline that could potentially interfere with bonding of the luting cement. A post of corresponding size is selected and tried in place, checking the occlusion and adjusting the post if necessary with a high-speed handpiece and diamond bur. A chemically or dual-cure adhesive resin cement is then used to bond the post in place. A composite core can now be constructed retaining as much coronal tooth structure as possible to provide a ferrule.
The discolouration seen is due to corrosion products, which resulted from the previous use of a non-precious metal post onto which gold was cast. This tooth has now been restored by the placement of a MTA apical plug. At a second appointment the remaining post space is etched, rinsed and dried, and a dentine bonding agent applied.
The Luminex post is removed and the space left is modified, so removing the Vaseline and preparing the tooth for an appropriate quartz-fibre post which is cemented with an adhesive resin luting cement. Finally a composite core is built up, either by free hand or with the use of a core former, to receive a crown.
Summary
In summary, whilst MTA appears to be an excellent alternative to the multiple visit apexification technique with calcium hydroxide, the traditional method of obturating the wide root canal using thermoplastic gutta-percha does not strengthen the root in any way. Should the tooth require future restoration with a post-retained crown, the weakened root could potentially fracture. This paper describes a technique that incorporates the advantages of using MTA as an apical barrier and internal rehabilitation of the root canal with composite resin. A quartz-fibre post subsequently bonded in place, allows the retention of a composite core, if required, and allows continued use of adhesive and aesthetic technology.
Conclusions
Endodontic treatment has progressed significantly over the last two decades leading to a greater knowledge, clinical success and concomitant cost of endodontic treatment. Failure in teeth that have been root canal treated is more likely to be the result of failure of the restoration that has been placed, rather than the endodontic treatment itself.49 It is therefore important that prior to endodontic treatment, a thorough pre-operative examination is carried out, not only with the endodontic techniques in mind, but also with regard to the feasibility of successfully restoring the tooth. In the first of this series of papers, the authors have therefore revisited this pre-operative assessment in some detail together with the assessment of teeth that have existing root canal fillings.
Whilst posterior multirooted teeth rarely require restoration with a post, anterior single-rooted teeth frequently do. Restoration of such teeth with posts is notoriously difficult and is associated with a high failure rate. In the second and third of these papers, the authors have described techniques and materials that should minimise the risk of failure. For success, emphasis should be placed on adequate post length and preservation of coronal tooth tissue to enable a ferrule to be created.
Throughout this series of papers the authors have presented what they regard as the best clinical evidence to support the techniques described. This final paper describes how compromised roots, whether as a result of a non-vital immature root, secondary caries around an existing post, or over-zealous, inappropriate tooth preparation, can be reinforced, thus maintaining a functional unit within the dental arch.
References
Lui JL . Composite resin reinforcement of flared canals using light-transmitting plastic posts. Quintessence Int 1994; 25: 313–319.
Rabie G, Trope M, Garcia C, Tronstad L . Strengthening and restoration of immature teeth with an acid-etch technique. Endo Dent Traumatol 1985: 1: 246–256.
Davy DT, Dilley GL, Krejci RF . Determination of stress patterns in root-filled teeth incorporating various dowel designs. J Dent Res 1981; 60: 1301–1310.
Deutsch AS, Cavalliari J, Musikant BL, Silverstein L, Lepley J, Petroni G . Root fracture and the design of prefabricated posts. J Prosthet Dent 1985; 53: 637–640.
Lui JL . Enhanced post crown retention in resin composite-reinforced, compromised, root-filled teeth: A case report. Quintessence Int 1999; 30: 601–606.
Kleier DJ, Barr ES . A study of endodontically apexified teeth. Endod Dent Traumatol 1991; 7: 112–117.
Mackie IC, Hill FJ . A clinical guide to the endodontic treatment of non-vital immature permanent teeth. Br Dent J 1999; 186: 54–58.
Finucane D, Kinirons MJ . Non-vital immature permanent incisors: factors that may influence treatment outcome. Endod Dent Traumatol 1999; 15: 273–277.
Ghose LJ, Baghdady VS, Hikmat BYM . Apexification of immature apices of pulpless permanent anterior teeth with calcium hydroxide. J Endod 1987; 13: 285–290.
Thater M, Marechaux SC . Induced root apexification following traumatic injuries of the pulp in children: follow-up study. J Dent Child 1988; 55: 190–195.
Cvek M, Nord CE, Hollender L . Antimicrobial effect of root canal debridement in teeth with immature roots. A clinical and microbiologic study. Odontol Revy 1976; 27: 1–10.
Koenigs JF, Heller AL, Brilliant JD, Melfi RC, Driskell TD . Induced apical closure of permanent teeth in adult primates using a resorbable form of tricalcium phosphate cement. J Endod 1975; 1: 102–106.
Roberts SC Jr, Brilliant JD . Tricalcium phosphate as an adjunct to apical closure in pulpless permanent teeth. J Endod 1975; 1: 263–269.
Coviello J, Brilliant JD . A preliminary clinical study on the use of tricalcium phosphate as an apical barrier. J Endod 1979; 5: 6–13.
Dimashkieh MR . The problem of the open apex — a new approach: oxidized regenerated cellulose technique. J Br Endod Soc 1977; 10: 9–16.
Rossmeisl R, Reader A, Melfi R, Marquard J . A study of freeze-dried (lyophilized) cortical bone used as an apical barrier in adult monkey teeth. J Endod 1982; 8: 219–226.
Rossmeisl R, Reader A, Melfi R, Marquard J . A study of freeze-dried dentin used as an apical barrier technique in adult monkey teeth. Oral Surg Oral Med Oral Pathol 1982; 53: 303–310.
Tronstad L . Tissue reactions following apical plugging of the root canal with dentin chips in monkeys teeth subjected to pulpectomy. Oral Surg Oral Med Oral Pathol 1978; 45: 297–304.
Oswald RJ, Friedman CE . Periapical response to dentin fillings. A pilot study. Oral Surg Oral Med Oral Pathol 1980; 49: 344–355.
Torabinejad M, Chivian N . Clinical applications of mineral trioxide aggregate. J Endod 1999; 25: 197–205.
Schwartz RS, Mauger M, Clement DJ, Walker WA 3rd . Mineral trioxide aggregate: a new material for endodontics. J Am Dent Assoc 1999; 130: 967–975.
Shabahang S, Torabinejad M . Treatment of teeth with open apices using mineral trioxide aggregate. Pract Periodontics Aesthet Dent 2000; 12: 315–320.
Witherspoon DE, Ham K . One-visit apexification: technique for inducing root-end barrier formation in apical closures. Pract Proced Aesthet Dent 2001; 13: 455–460.
Giuliani V, Baccetti T, Pace R, Pagavino G . The use of MTA in teeth with necrotic pulps and open apices. Dent Traumatol 2002; 18: 217–221.
Maroto M, Barberia E, Planells P, Vera V . Treatment of a non-vital immature incisor with mineral trioxide aggregate (MTA). Dent Traumatol 2003; 19: 165–169.
Lynn EA, Einbender S . The use of mineral trioxide aggregate to create an apical stop in previously traumatized adult tooth with blunderbuss canal. N Y State Dent J 2003; 69: 30–32.
Steinig TH, Regan JD, Gutmann JL . The use and predictable placement of Mineral trioxide Aggregate in one-visit apexification cases. Aust Endod J 2003; 29: 34–42.
Linsuwanont P . MTA apexification combined with conventional root canal treatment. Aust Endod J 2003; 29: 45–49.
Buchanan LS . The standardized-taper root canal preparation–Part 4. GT file technique in large root canals with large apical diameters. Int Endod J 2001; 34: 157–164.
Torabinejad M, Watson TF, Pitt Ford TR . Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J Endod 1993; 19: 591–595.
Torabinejad M, Rastergar AF, Kettering JD, Pitt Ford TR . Bacterial leakage of mineral trioxide aggregate as a root-end filling material. J Endod 1995; 21: 109–112.
Bates CF, Carnes DL, del Rio CE . Longitudinal sealing ability of mineral trioxide aggregate as a root-end filling material. J Endod 1996; 22: 575–578.
Fischer EJ, Arens DE, Miller CH . Bacterial leakage of mineral trioxide aggregate as compared with zinc-free amalgam, intermediate restorative material, and super-EBA as a root-end filling material. J Endod 1998; 24: 176–179.
Torabinejad M, Pitt Ford TR, McKendry DJ, Abedi HR, Miller DA, Kariyawasam SP . Histologic assessment of mineral trioxide aggregate as a root-end filling in monkeys. J Endod 1997; 23: 225–228.
Koh ET, Torabinejad M, Pitt Ford TR, Brady K, McDonald F . Mineral trioxide aggregate stimulates a biological response in human osteoblasts. J Biomed Mater Res 1997; 37: 432–439.
Koh ET, McDonald F, Pitt Ford TR, Torabinejad M . Cellular response to mineral trioxide aggregate. J Endod 1998; 24: 543–547.
Shabahang S, Torabinejad M, Boyne PP, Abedi H, McMillan P . A comparative study of root-end induction using osteogenic protein-1, calcium hydroxide, and mineral trioxide aggregate in dogs. J Endod 1999; 25: 1–5.
Hachmeister DR, Schindler WG, Walker WA 3rd, Thomas DD . The sealing ability and retention characteristics of mineral trioxide aggregate in a model of apexification. J Endod 2002; 28: 386–390.
Lui JL . A technique to reinforce weakened roots with post canals. Endod Dent Traumatol 1987; 3: 310–314.
Pires JA, Cvitko E, Denehy GE, Swift EJ Jr . Effects of curing tip distance on light intensity and composite resin microhardness. Quintessence Int 1993; 24: 517–521.
Guzy GE, Nicholls JI . In vitro comparison of intact endodontically treated teeth with and without post reinforcement. J Prosthet Dent 1979; 42: 39–44.
Lui JL . Depth of composite polymerization within simulated root canals using light-transmitting posts. Oper Dent 1994; 19: 165–168.
Johnson JK, Sakumara JS . Dowel form and tensile force. J Prosthet Dent 1978; 40: 645–649.
Saupe WA, Gluskin AH, Radke RA Jr . A comparative study of fracture resistance between morphological dowel and cores and a resin-reinforced dowel system in the intraradicular restoration of structurally compromised roots. Quintessence Int 1996; 27: 483–491.
Katebzadeh N, Dalton BC, Trope M . Strengthening immature teeth during and after apexification. J Endod 1998; 24: 256–259.
Vichi A, Grangini S, Davidson CL, Ferrari M . An SEM evaluation of several adhesive systems used for bonding fiber posts under clinical conditions. Dent Mater 2002; 18: 495–502.
Isidor F, Odman P, Brondum K . Intermittent loading of teeth restored using prefabricated carbon fibre posts. Int J Prosthodont 1996; 9: 131–136.
Cormier CJ, Burns DR, Moon P . In vitro comparison of the fracture resistance and failure mode of fibre, ceramic and conventional post systems at various stages of restoration. J Prosthodont 2001; 10: 26–36.
Ray HA, Trope M . Periapical status of endodontically treated teeth in relation to the quality of the root filling and the coronal restoration. Int Endod J 1995; 28: 12–18.
Author information
Authors and Affiliations
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Tait, C., Ricketts, D. & Higgins, A. Weakened anterior roots – intraradicular rehabilitation. Br Dent J 198, 609–617 (2005). https://doi.org/10.1038/sj.bdj.4812351
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4812351
This article is cited by
-
Clinical application of calcium silicate-based bioceramics in endodontics
Journal of Translational Medicine (2023)
-
Rethinking ferrule – a new approach to an old dilemma
British Dental Journal (2010)