Abstract
Von Hippel–Lindau disease (VHL) is an autosomal-dominant inherited condition that predisposes patients to develop renal cysts and tumors, most commonly in the second to fourth decades of life. Renal cysts and tumors have historically been a major cause of disease-related morbidity and mortality, so urologists are often called on to manage patients with VHL. Knowledge of the extrarenal manifestations of VHL (hemangioblastomas of the central nervous system and retina, endolymphatic sac tumors, pancreatic cysts, epididymal and broad-ligament cysts, and pheochromocytomas) and integration of nonurologic specialties into management teams for VHL patients will help to achieve successful outcomes. Screening for renal manifestations of VHL, by regular imaging of the abdomen, begins late in the second decade of life. Because renal tumors in VHL can be multifocal and bilateral, management can be complex. Radical nephrectomy removes all tissue at risk for forming renal tumors; however, this necessitates renal replacement therapy. In an effort to control cancer effectively while preserving native renal function and minimizing intervention, some researchers have proposed an observational strategy. Patients are screened until the largest tumor reaches 3 cm in diameter, at which time operative intervention is recommended. Nephron-sparing surgery is undertaken, whenever technically feasible, with the goal of removing all tumors in that renal unit. The role of minimally invasive technologies is currently being evaluated in selected patients with VHL renal masses. Elucidation of molecular pathways associated with VHL renal tumors may facilitate development of effective medical treatments for these lesions in the future.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Chow WH et al. (1999) Rising incidence of renal cell cancer in the United States. JAMA 281: 1628–1631
Zbar B et al. (2003) Studying cancer families to identify kidney cancer genes. Annu Rev Med 54: 217–233
Choyke PL et al. (2003) Hereditary renal cancers. Radiology 226: 33–46
Linehan WM et al. (2003) The genetic basis of cancer of the kidney. J Urol 170: 2163–2172
von Hippel E (1904) Uber eine sehr seltene Erkrankung der netzhaut. Graefes Arch Clin Exp Ophthalmol 59: 83–106
Lindau A (1926) Studien ber kleinbirncysten bau: pathogenese und beziehungen zur angiomatosis retinae. Acta Radiol Microbiol Scandinavica 1 (Suppl): 1–128
Melmon KL and Rosen SW (1964) Lindau's disease. Am J Med 36: 595–617
Lonser RR et al. (2003) von Hippel–Lindau disease. Lancet 361: 2059–2067
Latif F et al. (1993) Identification of the von Hippel–Lindau disease tumor suppressor gene. Science 260: 1317–1320
Gnarra JR et al. (1994) Mutations of the VHL tumour suppressor gene in renal carcinoma. Nat Genet 7: 85–90
Herring JC et al. (2001) Parenchymal sparing surgery in patients with hereditary renal cell carcinoma: 10-year experience. J Urol 165: 777–781
Walther MM et al. (1999) Renal cancer in families with hereditary renal cancer: prospective analysis of a tumor size threshold for renal parenchymal sparing surgery. J Urol 161: 1475–1479
Frydenberg M et al. (1993) Conservative renal surgery for renal cell carcinoma in von Hippel–Lindau's disease. J Urol 149: 461–464
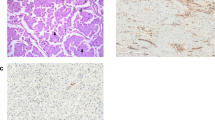
Poston CD et al. (1995) Characterization of the renal pathology of a familial form of renal cell carcinoma associated with von Hippel–Lindau disease: clinical and molecular genetic implications. J Urol 153: 22–26
Walther MM et al. (1995) Prevalence of microscopic lesions in grossly normal renal parenchyma from patients with von Hippel–Lindau disease, sporadic renal cell carcinoma and no renal disease: clinical implications. J Urol 154: 2010–2014
Stolle C et al. (1998) Improved detection of germline mutations in the von Hippel–Lindau disease tumor suppressor gene. Hum Mutat 12: 417–423
Choyke PL et al. (1995) von Hippel–Lindau disease: genetic, clinical, and imaging features. Radiology 194: 629–642
Eisenhofer G et al. (1999) Plasma normetanephrine and metanephrine for detecting pheochromocytoma in von Hippel–Lindau disease and multiple endocrine neoplasia type 2. N Engl J Med 340: 1872–1879
Maher ER et al. (1990) Clinical features and natural history of von Hippel–Lindau disease. Q J Med 77: 1151–1163
Choyke PL (2003) Imaging of hereditary renal cancer. Radiol Clin North Am 41: 1037–1051
Novick AC and Streem SB (1992) Long-term followup after nephron sparing surgery for renal cell carcinoma in von Hippel–Lindau disease. J Urol 147: 1488–1490
Goldfarb DA et al. (1997) Results of renal transplantation in patients with renal cell carcinoma and von Hippel–Lindau disease. Transplantation 64: 1726–1729
Pearson JC et al. (1980) A plea for conservation of kidney in renal adenocarcinoma associated with von Hippel–Lindau disease. J Urol 124: 910–912
Levine E et al. (1983) Diagnosis and management of asymptomatic renal cell carcinomas in von Hippel–Lindau syndrome. Urology 21: 146–150
Loughlin KR and Gittes RF (1986) Urological management of patients with von Hippel–Lindau's disease. J Urol 136: 789–791
Spencer WF et al. (1988) Surgical treatment of localized renal cell carcinoma in von Hippel–Lindau's disease. J Urol 139: 507–509
Lund GO et al. (1994) Conservative surgical therapy of localized renal cell carcinoma in von Hippel–Lindau disease. Cancer 74: 2541–2545
Steinbach F et al. (1995) Treatment of renal cell carcinoma in von Hippel–Lindau disease: a multicenter study. J Urol 153: 1812–1816
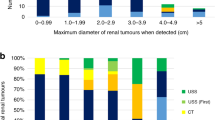
Duffey BG et al. (2004) The relationship between renal tumor size and metastases in patients with von Hippel–Lindau disease. J Urol 172: 63–65
United States Renal Data System 1997 Annual Data Report (1997) Washington, D.C., United States Department of Health and Human Services. [Online at http://www.usrds.org/adr_1997.htm]
Walther MM et al. (1995) Parenchymal sparing surgery in patients with hereditary renal cell carcinoma. J Urol 153: 913–916
Turner KJ et al. (2001) von Hippel–Lindau disease: renal tumors less than 3 cm can metastasize. J Urol 165: 1207
Walther MM et al. (1995) Enucleation procedures in patients with multiple hereditary renal tumors. World J Urol 13: 248–250
Walther MM et al. (1994) Evaluation of color Doppler intraoperative ultrasound in parenchymal sparing renal surgery. J Urol 152: 1984–1987
Choyke PL et al. (2001) Intraoperative ultrasound during renal parenchymal sparing surgery for hereditary renal cancers: a 10-year experience. J Urol 165: 397–400
Shingleton WB and Sewell PE Jr (2002) Percutaneous renal cryoablation of renal tumors in patients with von Hippel–Lindau disease. J Urol 167: 1268–1270
Pavlovich CP et al. (2002) Percutaneous radio frequency ablation of small renal tumors: initial results. J Urol 167: 10–15
Gervais DA et al. (2003) Renal cell carcinoma: clinical experience and technical success with radio-frequency ablation of 42 tumors. Radiology 226: 417–424
Su LM et al. (2003) Percutaneous computed tomography-guided radiofrequency ablation of renal masses in high surgical risk patients: preliminary results. Urology 61: 26–33
Farrell MA et al. (2003) Imaging-guided radiofrequency ablation of solid renal tumors. AJR Am J Roentgenol 180: 1509–1513
Hwang JJ et al. (2004) Radio frequency ablation of small renal tumors: intermediate results. J Urol 171: 1814–1818
Linehan WM et al. (2004) Genetic basis of cancer of the kidney: disease-specific approaches to therapy. Clin Cancer Res 10: 6282S–6289S
Duan DR et al. (1995) Inhibition of transcription elongation by the VHL tumor suppressor protein. Science 269: 1402–1406
Pause A et al. (1997) The von Hippel–Lindau tumor-suppressor gene product forms a stable complex with human CUL-2, a member of the Cdc53 family of proteins. Proc Natl Acad Sci USA 94: 2156–2161
Maxwell PH et al. (1999) The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature 399: 271–275
Kaelin WG Jr (2004) The von Hippel–Lindau tumor suppressor gene and kidney cancer. Clin Cancer Res 10: 6290S–6295S
Isaacs JS et al. (2002) Hsp90 regulates a von Hippel Lindau-independent hypoxia-inducible factor-1 alpha-degradative pathway. J Biol Chem 277: 29936–29944
Grubb RL et al. (2005) Management of inherited forms of renal cancer. In: Comprehensive Textbook of Genitourinary Oncology (Eds Vogelzang NJ et al.) Baltimore: Lippincott, Williams and Wilkins, in press
Linehan WM and Zbar B (2004) Focus on kidney cancer. Cancer Cell 6: 223–228
Acknowledgements
Thanks to R Dreyfuss (Medical Arts and Photography Branch, National Institutes of Health) and L Errington (Urologic Oncology Branch, National Cancer Institute) for their assistance in the preparation of figures and text for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- HEMANGIOBLASTOMAS
-
Tumors, generally benign, made up of blood vessels, commonly located in the cerebellum and spinal cord
- ANGIOMAS
-
Tumors composed primarily of lymphatic or blood vessels
- PHEOCHROMOCYTOMAS
-
Tumors of the adrenal gland, derived from chromaffin cells, that cause excessive adrenaline production and hypertension
- FUHRMAN GRADE
-
A 4-point scale that grades malignant potential of renal cancer cells based on the appearance of the nuclei
- CRYOABLATION
-
Destruction of tissue by freezing with argon gas or liquid nitrogen (−140°C to −195°C) delivered via a cryoprobe; cell death occurs in two stages: immediate cellular necrosis from the freeze/thaw cycles followed by microcirculatory insufficiency and resultant ischemic necrosis
- RADIOFREQUENCY ABLATION (RFA)
-
Heat-induced tissue destruction using an electrical current that is passed through a needle electrode placed directly into the tissue
- HYPOXIA-INDUCIBLE FACTORS (HIF)
-
Proteins that activate transcription ('transcription factors') of genes involved in tumorigenesis; HIF degradation is regulated by the VHL gene product in an oxygen-dependent manner
- HEAT-SHOCK PROTEIN 90 (HSP90)
-
A molecular chaperone that activates several protein kinases; inhibitors of HSP90 have antiproliferative and antitumor activities
Rights and permissions
About this article
Cite this article
Grubb, R., Choyke, P., Pinto, P. et al. Management of von Hippel–Lindau-associated kidney cancer. Nat Rev Urol 2, 248–255 (2005). https://doi.org/10.1038/ncpuro0179
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpuro0179
This article is cited by
-
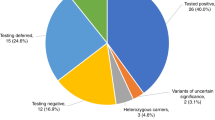
Evaluation of tumour surveillance protocols and outcomes in von Hippel-Lindau disease in a national health service
British Journal of Cancer (2022)
-
Expression profile and bioinformatics analysis of COMMD10 in BALB/C mice and human
Cancer Gene Therapy (2020)
-
Hereditary leiomyomatosis and renal cell cancer (HLRCC): renal cancer risk, surveillance and treatment
Familial Cancer (2014)
-
Active surveillance of renal masses in von Hippel-Lindau disease: growth rates and clinical outcome over a median follow-up period of 56 months
Familial Cancer (2012)
-
Laparoscopic Organ‐Sparing Resection of Von Hippel‐Lindau Disease‐Associated Pancreatic Neuroendocrine Tumors
World Journal of Surgery (2011)