Abstract
The neonatal brain is extremely vulnerable to injury during periods of hypoxia and/or ischemia. Risk of brain injury is increased during neonatal cardiac surgery, where pre-existing hemodynamic instability and metabolic abnormalities are combined with long periods of low cerebral blood flow and/or circulatory arrest. Our understanding of events associated with cerebral hypoxia-ischemia during cardiopulmonary bypass (CPB) remains limited, largely due to inadequate tools to quantify cerebral oxygen delivery and consumption non-invasively and in real-time. This pilot study aims to evaluate cerebral blood flow (CBF) and oxygen metabolism (CMRO2) intraoperatively in neonates by combining two novel non-invasive optical techniques: frequency-domain near-infrared spectroscopy (FD-NIRS) and diffuse correlation spectroscopy (DCS). CBF and CMRO2 were quantified before, during and after deep hypothermic cardiopulmonary bypass (CPB) in nine neonates. Our results show significantly decreased CBF and CMRO2 during hypothermic CPB. More interestingly, a change of coupling between both variables is observed during deep hypothermic CPB in all subjects. Our results are consistent with previous studies using invasive techniques, supporting the concept of FD-NIRS/DCS as a promising technology to monitor cerebral physiology in neonates providing the potential for individual optimization of surgical management.
Similar content being viewed by others
Introduction
Given its critical functions, the brain is the ultimate organ whose outcome must be optimized in any operating room or intensive care setting. All surgical and medical management strategies must be designed to prevent or at least minimize brain injury. Neonates undergoing cardiac surgery with cardiopulmonary bypass (CPB) are particularly vulnerable to hypoxic-ischemic brain injury1,2,3. Since CPB requires periods of reduced systemic flow and/or circulatory arrest, cerebral hypothermia is routinely used with a primary goal to reduce cerebral oxygen consumption, such that the risk of hypoxic-ischemic brain injury is minimized. Laboratory and human studies have shown that hypothermia produces a significant neuroprotective reduction in cerebral oxygen consumption4,5. Despite the fact that hypothermia and new surgical techniques have led to a significant improvement in survival rates, infants undergoing cardiac surgery continue to show abnormal long term neurodevelopmental outcomes6. To date there is no information to demonstrate that current neuromonitoring methods prevent brain injury and improve neurodevelopmental outcomes7,8,9,10,11. Our understanding of perioperative cerebral hypoxia-ischemia in neonates undergoing complex cardiac surgery remains limited, primarily due to the lack of adequate tools to quantify cerebral oxygen delivery and consumption non-invasively, in real-time, and at the bedside.
Seminal work by Greeley and colleagues showed that cerebral metabolism is exponentially related to temperature during hypothermic CPB in neonates, infants and children12. They also showed that long periods of deep hypothermic circulatory arrest (DHCA) alter cerebral metabolism and blood flow after the arrest period despite adequate hypothermic suppression of metabolism13. Antegrade regional cerebral perfusion (RCP) has been proposed as a better perfusion technique to avoid or minimize duration of circulatory arrest and maximize oxygen delivery to the brain14. However, clinical outcomes available so far do not provide strong evidence of the superiority of RCP over DHCA15. This has led to a wide variation in practice and the fundamental question of whether it is possible to optimize cerebral oxygen delivery to match cerebral oxygen consumption in individual patients. Yet, optimizing cerebral oxygen delivery first requires a technique for monitoring cerebral metabolism with minimal risk for the patient.
The techniques used by Greeley et al. 25 years ago to measure cerebral metabolism are invasive and/or require exposure to radioactive Xenon12,13. Greeley’s methods are also technically challenging to perform in the operating room, and are not feasible in routine clinical practice. As a result, these experiments have not been repeated. Currently, intraoperative brain health is assessed by monitoring oxygenation with continuous-wave near infrared spectroscopy (CW-NIRS). CW-NIRS is limited to work as a trend monitor, as it cannot measure absolute concentrations of oxy- (HbO2) and deoxy-hemoglobin (HbR). Consequently, it cannot provide absolute cerebral oxygen saturation (SO2) but only relative changes (rSO2). This lack of quantification limits the estimation of normative values and undermines comparisons between normal and at-risk neonates. Recently, the advanced non-invasive optical techniques of frequency-domain near-infrared spectroscopy (FD-NIRS) and diffuse correlation spectroscopy (DCS) have demonstrated the ability to not only measure absolute cerebral oxygen saturation but also provide quantitative measures of cerebral blood volume (CBV) and a quantitative index of cerebral perfusion (CBFi), enabling a quantitative index of cerebral oxygen consumption (CMRO2i) to be calculated16,17,18,19. These advanced optical technologies have the potential to provide similar quantitative information regarding brain health as the invasive methods of Greeley with the advantages of lower risk to the patient and the same ease of use as current commercial NIRS devices.
This pilot study aims to evaluate the ability of FD-NIRS/DCS to quantify intraoperative cerebral blood flow and oxygen metabolism non-invasively in neonates. Because of the extreme physiologic manipulations induced by changes in perfusion and temperature (CPB, deep hypothermia, and regional cerebral perfusion), neonatal cardiac surgery provides an excellent opportunity to evaluate SO2, CBFi and CMRO2i intraoperatively. If clinical translation of these technologies becomes feasible, they hold great promise in monitoring cerebral health in real-time, providing the potential for individual optimization of cerebral oxygen delivery to match cerebral metabolic demands.
Results
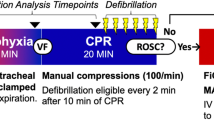
Cardiac diagnosis and CPB parameters for each patient are summarized in Table 1. Nasopharyngeal temperature was maintained less than 24 °C in all patients during hypothermic CPB. Brief DHCA was utilized in all subjects. Seven patients received RCP following brief DHCA. Two patients had continuous flow CPB instead. A timeline of the measurements is shown in Fig. 1 with measurements made at 5 time points (see Methods for a detailed description of the measurement protocol).
Table 2 summarizes the physiologic parameters at each time point, including pH and PaCO2 values uncorrected for body temperature. Hematocrit (Hct, %) was maintained in the range (27–37) % during CPB.
Cerebral hemodynamics during neonatal cardiac surgery measured by FD-NIRS/DCS
Significant changes in cerebral oxygenation and blood flow were found at the different stages of surgery (Fig. 2). In particular, SO2, (CaO2 − CvO2), CBFi and CMRO2i showed statistically significant changes with respect to baseline (PI stage) during deep hypothermia (shaded regions). After weaning from CPB, SO2, (CaO2 − CvO2), CBFi and CMRO2 were not significantly different from baseline. No significant changes were registered in CBV and CaO2.
The variability of our measurements was assessed by computing a coefficient of variation (COV). The average COV for SO2 and CBFi measurements (consisting of 3 repetitions) was 2.4% (SEM = 0.4%) and 10.7% (SEM = 0.5%), respectively.
CBFi/CMRO2i coupling
The CBFi/CMRO2i ratio provides an indicator of the coupling between both parameters at different stages (Fig. 3). During deep hypothermia, the CBFi/CMRO2i ratio showed a significant increase with respect to baseline (p < 0.005), indicating cerebral blood flow in excess of cerebral demand. This ratio decreased during rewarming (but remained significantly higher from the baseline) and returned to baseline levels after weaning from CPB (PCPB stage).
Relationship between temperature and CMRO2i
Figure 4 shows the temperature dependency of CMRO2i during CPB in a temperature range of 16 °C to 35 °C. The relationship can be described by an exponential function: CMRO2i = 0.066 e0.08T (r2 = 0.57, p = 0.0003). In order to rule out the effect of circulatory arrest, only values corresponding to baseline (PI) and early CPB (CPB1) (before circulatory arrest or RCP) were considered in the linear regression between temperature and the logarithm of CMRO2i.
Neurological complications
The intraoperative and postoperative course was uneventful in 7/9 subjects with no neurological signs or symptoms triggering a postoperative neurological consult or clinical neuroimaging. One neonate (subject ID: 8) had an unexpected decrease in CBFi in the post cardiopulmonary bypass phase (lowest observed but within one standard deviation of the group mean). This neonate required a neurological consult due to a complicated cardiac surgery, extended bypass and concern for intraoperative hypoperfusion and hypoxic ischemic injury. A post-operative research MRI obtained on this subject 13 days after surgery showed multiple foci of white matter injury of unclear etiology as a preoperative MRI was not obtained. However intraoperative white matter injury due to hypoperfusion cannot be excluded. This neonate was discharged with no focal neurological deficit but is too young for neurocognitive testing. Another neonate (subject ID: 4) required ECMO immediately after surgery. This neonate also required a neurological consult due to poor cardiac output and need for ECMO. Care was eventually withdrawn due to uncorrectable complex congenital heart disease. This neonate had high CBFi post induction but was too unstable for post bypass measures.
Discussion
In this pilot study, we used a custom-made FD-NIRS/DCS system to quantify cerebral blood flow and oxygen metabolism during neonatal cardiac surgery. While several studies have employed these techniques to monitor neonatal cardiac surgical patients preoperatively and/or postoperatively18,19,20,21, this is the first report of intraoperative CBFi and CMRO2i measurements in neonates undergoing hypothermic CPB. The patterns observed in our measurements are in agreement with previous results obtained with invasive techniques in a similar population12, suggesting that FD-NIRS/DCS is a promising technology to monitor individual cerebral oxygen metabolism and hemodynamics during complex neonatal cardiac surgical procedures.
While neurological complications in adult cardiac surgery are most commonly embolic in nature, those in pediatric populations are more frequently related to hypoperfusion and hypoxia, supporting the importance of understanding the balance between cerebral oxygen delivery (provided by CBF) and consumption. Greeley et al. assessed these variables by using Xenon-clearance methods and jugular bulb oximetry12,13. In studies conducted in neonates and children, CMRO2 decreased exponentially while CBF decreased linearly during hypothermic CPB, leading to a relative excess of blood flow, a situation referred to as “luxury perfusion”. Our findings using non-invasive optical methods are consistent with these reports. Specifically, we showed a significant decrease ( >60%) of CMRO2i during hypothermic CPB relative to baseline (Fig. 2), which accompanied an exponential decay with temperature (Fig. 4). While CBFi also decreased, it exhibited a more moderate reduction (31%) during hypothermia with respect to baseline values (Fig. 2). The variability of our SO2 and CBFi measurements (COVSO2 = 2.4% and COVCBFi = 10.7%) is below the physiological changes observed at the different stages, suggesting that our observations are driven by physiological fluctuations.
Our results also show a change of coupling between cerebral blood flow and oxygen consumption (Fig. 3). This is illustrated by the CBFi/CMRO2i ratio, or the inverse of oxygen extraction, that exhibits a two fold increase of the average ratio during deep hypothermic bypass relative to baseline. Flow/metabolism coupling is a complex process influenced by many parameters (temperature, PaCO2, pH, etc.). As body temperature decreases and pH increases with hypothermia, in the pH stat strategy CO2 is added to the blood during CPB in order to maintain a pH of 7.4 at the patient’s actual body temperature. Thus, the increase in CBFi relative to CMRO2i during deep hypothermia could be partially explained by the counteracting effect between temperature and PaCO2, as it has been shown that CO2 is a strong cerebral vasodilator during hypothermic CPB and has the potential to disrupt cerebral autoregulation22,23. The mechanism and consequences of the change of coupling are still incompletely understood. The luxury perfusion is thought to provide an element of cerebral protection and hence positively influence neurodevelopmental outcome5. However, the influence of hypothermia and its interaction with other variables during CPB is complex. Hypothermia increases the O2 affinity of hemoglobin so that the fraction of CMRO2 dependent on dissolved O2 increases at deep hypothermia24. Dissolved O2 can theoretically meet the brain O2 requirements if CBF is adequate. An important question for future studies will be to improve our understanding of the implications of hypothermia itself and its relationship to physiological variables such as CBF and CMRO2 and neurodevelopmental outcomes. A potential approach for studying this question is by studying groups of patients with a similar diagnosis undergoing CPB with deep (<22 °C) versus mild-moderate (28–35 °C) hypothermia.
Commercial CW-NIRS systems have been previously used to measure cerebral oxygenation in neonates undergoing cardiac surgery25,26. As discussed above, CW-NIRS systems only provide relative measurements of cerebral oxygenation (rSO2) and are prone to inaccuracies in the high and low ends of the scale27,28.Our preliminary comparisons between SO2 and rSO2 (as measured by a commercial system Fore-Sight, CAS Medical Systems Inc., Branford, CT) show that while both measurements seem to follow a similar trend, rSO2 overestimates cerebral oxygen saturation, particularly in the lower ranges (Supplementary Figure 1). A more systematic study with a larger sample needs to be performed in order to explain this bias.
SO2 alone does not offer a measure of cerebral perfusion. As discussed by Elwell and colleagues, SO2 belies the complexity of the multiple processes determining cerebral oxygen delivery and consumption29. Cerebral blood flow velocity measured by TCD is a reliable surrogate of cerebral blood flow in large arteries provided that the diameter of the vessel remains constant, an assumption that might not be met during CPB. Moreover, as the TCD signal depends on the angle of insonation and is thus operator dependent, it is technically challenging to obtain consistent measurements, hindering accurate real-time assessment of cerebral blood flow. DCS is complementary to TCD as it measures cerebral blood flow in the microvasculature by measuring light intensity fluctuations caused by the movement of red blood cells30,31. While absolute CBFi does not have units of cerebral blood flow, it has shown a strong correlation with cerebral blood flow measured by bolus tracking techniques using time-domain NIRS in a neonatal pig model32 as well as in preterm neonates33, and with cerebral blood flow measured by phase-encoded velocity mapping using magnetic resonance imaging in neonates34. Since both DCS and FD-NIRS are sensitive to microvasculature underneath the optical sensor, they offer better estimates of CMRO2 than by combining SO2 NIRS with other modalities like TCD which measure blood velocity in large vessels and may not accurately reflect cortical perfusion at the site of the probe.
This pilot study has several limitations. Because of routine use of a commercial cerebral oximeter and limited space on the forehead, we only performed measurements overlying the right frontal cortex. Future studies will include additional locations such as parietal and temporal regions in order to account for potential regional variability of cerebral blood flow and metabolism.
While FD-NIRS and DCS have the ability to perform continuous measurements of SO2 and CBFi, we only considered a number of short measurements to simplify the probe design and avoid confounding effects such as motion and instrument drift. Future implementations will consider the design of ergonomic probes that can be attached to the infant’s head throughout the entire surgery and newer systems with improved stability, thus providing continuous measurements of perfusion and oxygenation.
The goal of this pilot study was to test the ability to track major metabolic changes due to extreme physiologic manipulations. Despite the small sample size (N = 9), we were able to obtain statistically significant changes at different stages of the surgery that are consistent with previous reports from larger studies. However, larger datasets will be required to answer subtler questions such as the effect of perfusion techniques (DHCA versus RCP) on cerebral blood flow and oxygenation, or metabolic variability associated with specific cardiac defects.
In summary, this pilot study demonstrated the ability to non-invasively track the extreme cerebral metabolic changes during neonatal cardiac surgery. Our results are consistent with previous reports from invasive studies and support the idea of FD-NIRS/DCS as a promising technology to monitor individual cerebral physiology in neonatal patients.
Methods
The study protocol was reviewed and approved by the Boston Children’s Hospital Committee on Clinical Investigation. The study method was designed and carried out in accordance with the BCH Committee on Clinical Investigation requirements and the regulations that govern human subjects’ research.
Subjects, anesthetic and CPB management
Nine neonates (median gestational age: 39 weeks; median weight: 3.1 kg) admitted to the Cardiac Intensive Care Unit at Boston Children’s Hospital were enrolled in the study. Parents who agreed to participate were asked to read and sign an informed consent form as approved by the BCH Committee on Clinical Investigation. Only neonates undergoing cardiac surgery for congenital heart disease within 30 days of birth were considered eligible. Infants with a known or suspected syndrome, craniofacial abnormality, sepsis, metabolic disorder, brain malformation, or brain mass lesion were excluded from the study.
All patients underwent palliative or reparative cardiac surgery within the first week of life (median post-natal age at surgery: 4 days). Anesthesia consisted of high-dose opioid (fentanyl ~100 mcg/kg) and muscle relaxant, supplemented with isoflurane and/or midazolam as tolerated. CPB was non-pulsatile with a target hematocrit of 30% at initiation of bypass. Ice was placed around the head and moved aside during NIRS measurements. Temperature was monitored in the nasopharynx as a reflection of brain temperature per our routine practice. In addition, arterial and venous return temperatures during CPB were recorded. A pH-stat strategy (blood gas management with temperature correction) was used during core cooling, low-flow hypothermic bypass, and regional cerebral perfusion (RCP). Mean duration of cooling was 21 minutes (Fig. 1). CPB parameters are summarized in Table 1.
Study protocol
A total of 5 measurements were performed on each patient (Fig. 1). First, a baseline measurement (post-induction; PI) was made under stable conditions following induction of anesthesia, endotracheal intubation, and placement of arterial and venous lines, shortly before skin incision. The second measurement (CPB1) was performed at the end of core cooling, i.e., when the patient reached the cooling target temperature (mean ± SD: 21 ± 4 minutes after initiation of CPB). The third measurement was made after 15 minutes of RCP (RCP; n = 7; 16 ± 5 minutes after start of RCP) or after an hour of continuous flow bypass (CPB2; n = 2; 57 ± 10 minutes after onset of CPB). The timing of the third measurement for both the RCP patients and continuous flow patients was similar (~60 minutes after onset of CPB). A fourth measurement (RW) was done when the patient was rewarmed to 30 °C (nasopharyngeal temperature) and prior to cardiac ejection. Given the fast dynamics of this stage, some measurements were performed within a broader range of temperatures (27 °C–35 °C). The fifth measurement (PCPB) was performed when the patient was stable and ready to leave the OR. In all stages, the probe was placed on the right side of the infant’s forehead. A commercial cerebral oximeter was placed on the left side of the forehead as part of routine clinical use.
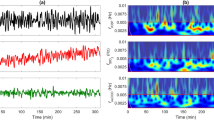
Instrumentation and optical data analysis
The FD-NIRS system (OxiplexTS, ISS Inc., Champaign, IL, USA) has two banks of laser diode sources operating at 8 wavelengths (670–830) nm and two photomultiplier tube (PMT) detectors. The laser sources are modulated at 110 MHz, and the PMT detectors operate with a modulation of 110 MHz + 5 kHz for heterodyne detection at 5 kHz. The DCS system has a long coherence length laser source operating at 785 nm and four photon-counting avalanche photodiode (APD) detectors. An eight-channel correlator is used to convert the detected light at each DCS detector channel into temporal intensity autocorrelation functions over a delay time range of (2 10−7–0.5) seconds.
A custom-made probe arranges FD-NIRS and DCS sources and detectors in a single row, allowing for FD-NIRS measurements at four source-detector (SD) distances (1.5, 2.0, 2.5, and 3.0 cm) and DCS measurements at a single SD distance (2.0 cm). Fiber bundles are used to couple FD-NIRS sources and detectors. The DCS laser is coupled to a multimode optical fiber and diffused at the fiber tip to provide power levels that comply with the ANSI standard. Each of the four DCS detectors is coupled to a single mode optical fiber. The four DCS detection single-mode fibers are placed at the same SD distance in order to increase signal-to-noise ratio of the detected DCS signal.
For FD-NIRS, absorption (μa) and scattering (μs’) of the sampled tissue were estimated from the amplitude attenuation and phase shift measured at each wavelength and SD distance using the multi-distance frequency-domain method35. Measurements taken on a phantom block with known optical properties were used to estimate coupling coefficients between tissue and optical fibers. Absolute oxygenated (HbO2) and deoxygenated (HbR) hemoglobin were derived from the wavelength-dependent absorption coefficients using hemoglobin extinction coefficients reported in the literature36 and assuming a water concentration of 75%37. Cerebral oxygen saturation was defined as  .
.
For DCS, each measured intensity autocorrelation function was fit to obtain a cerebral blood flow index (CBFi) using the analytical semi-infinite solution to the correlation diffusion equation for a homogenous medium30,38. Individual FD-NIRS derived absorption and scattering coefficients at 785 nm were used in the fitting of CBFi at each measured time point (Supplementary Figure 2). Note that the DCS technique provides a measure of microvascular perfusion by quantifying intensity fluctuations of multiply scattered light due to the movement of red blood cells inside the sampled tissue. CBFi, measured in cm2/sec, has been validated as a measure of regional cerebral blood flow32,33,34.
The optical probe was sanitized and inserted into a single use plastic cover. The FD-NIRS/DCS system was kept outside the sterile surgical site. FD-NIRS and DCS measurements were repeated three times per surgery time point on the infant’s right forehead. For each repetition, the probe was repositioned in a slightly different area to account for local inhomogeneities such as hair and superficial large vessels. FD-NIRS/DCS acquisition time was set to 20 seconds and the three repeated measurements were averaged together to obtain a single value at each time point.
We assessed reproducibility of the SO2 and CBFi measurements by calculating a coefficient of variation (COV = standard deviation/mean) for each set of three measurements for each every subject included in the study.
Measurements of brain metabolism and blood values
An index of the cerebral metabolic rate of oxygen (CMRO2i, cm2/s · mL O2/dL) was calculated using Fick’s principle:

where CaO2 is the oxygen content of arterial blood and CvO2 is the oxygen content of mixed venous blood. The oxygen content CxO2 (mL O2/dL), with x = a or v denoting arterial or venous blood, was calculated according to the equation:

where Hb (g/dL) is the hemoglobin concentration in blood, SxO2 (%) is the arterial or venous oxygen saturation and PxO2 (mmHg) is the partial pressure of oxygen in arterial blood or mixed venous blood.Venous oxygen saturation, SvO2, was derived from SO2 measured with FD-NIRS and SaO2 obtained from the arterial blood sample using the following equation:

where α + β = 1, and β = 0.75 is the percent contribution of the venous compartment to the SO2 measurement39.
Cerebral blood volume (CBV, mL/100 g) was calculated as

where HbT (μMol) is the total hemoglobin concentration, MWHb (65,400 g/Mol) is the molecular weight of hemoglobin, and Dbt (1.05 g/ml) is the brain tissue density. Finally, oxygen extraction was calculated as (CaO2 − CvO2).
Statistics
All values are given as mean ± standard error of the mean (SEM) unless stated otherwise. Changes between baseline (PI) and other time points were tested using a Wilcoxon two-sided signed-rank test. The dependency of CMRO2i on brain temperature was tested by linear regression analysis. Pearson correlations were used to examine the relationship of CPB flow rate with CBFi and mean arterial pressure (MAP). A p-value < 0.05 was considered to be statistically significant. In tables and figures, *indicates p < 0.05, **indicates p < 0.005, and ***indicates p < 0.0005.
Additional Information
How to cite this article: Ferradal, S. L. et al. Non-invasive Assessment of Cerebral Blood Flow and Oxygen Metabolism in Neonates during Hypothermic Cardiopulmonary Bypass: Feasibility and Clinical Implications. Sci. Rep. 7, 44117; doi: 10.1038/srep44117 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Licht, D. J. et al. Preoperative cerebral blood flow is diminished in neonates with severe congenital heart defects. J. Thorac. Cardiovasc. Surg. 128, 841–849 (2004).
Petit, C. J. et al. Preoperative Brain Injury in Transposition of the Great Arteries Is Associated With Oxygenation and Time to Surgery, Not Balloon Atrial Septostomy. Circulation 119, 709–716 (2009).
McQuillen, P. S. et al. Temporal and anatomic risk profile of brain injury with neonatal repair of congenital heart defects. Stroke; a journal of cerebral circulation 38, 736–741 (2007).
du Plessis, A. J. et al. Cerebral oxygen supply and utilization during infant cardiac surgery. Ann. Neurol. 37, 488–497 (1995).
Sakamoto, T. et al. Interaction of temperature with hematocrit level and pH determines safe duration of hypothermic circulatory arrest. J Thorac Cardiovasc Surg 128, 220–232 (2004).
Gaynor, J. W. et al. Neurodevelopmental outcomes after cardiac surgery in infancy. Pediatrics 135, 816–825 (2015).
Andropoulos, D. B. et al. Changing Expectations for Neurological Outcomes After the Neonatal Arterial Switch Operation. Ann. Thorac. Surg. 94, 1250–1256 (2012).
Andropoulos, D. B. et al. Neurodevelopmental outcomes after regional cerebral perfusion with neuromonitoring for neonatal aortic arch reconstruction. The Annals of thoracic surgery 95, 648–654 (2013).
Andropoulos, D. B. et al. Brain immaturity is associated with brain injury before and after neonatal cardiac surgery with high-flow bypass and cerebral oxygenation monitoring. J. Thorac. Cardiovasc. Surg. 139, 543–556 (2010).
Kussman, B. D. et al. Relationship of intraoperative cerebral oxygen saturation to neurodevelopmental outcome and brain magnetic resonance imaging at 1 year of age in infants undergoing biventricular repair. Circulation 122, 245–254 (2010).
Hirsch, J. C., Charpie, J. R., Ohye, R. G. & Gurney, J. G. Near-infrared spectroscopy: what we know and what we need to know-a systematic review of the congenital heart disease literature. The Journal of thoracic and cardiovascular surgery 137, 154–159 (2009).
Greeley, W. J. et al. The effect of hypothermic cardiopulmonary bypass and total circulatory arrest on cerebral metabolism in neonates, infants, and children. The Journal of thoracic and cardiovascular surgery 101, 783–794 (1991).
Greeley, W. J., Kern, F. H., Meliones, J. N. & Ungerleider, R. M. Effect of deep hypothermia and circulatory arrest on cerebral blood flow and metabolism. The Annals of thoracic surgery 56, 1464–1466 (1993).
Pigula, F. A., Nemoto, E. M., Griffith, B. P. & Siewers, R. D. Regional low-flow perfusion provides cerebral circulatory support during neonatal aortic arch reconstruction. The Journal of thoracic and cardiovascular surgery 119, 331–339 (2000).
Algra, S. O. et al. Neurological injury after neonatal cardiac surgery: a randomized, controlled trial of 2 perfusion techniques. Circulation 129, 224–233 (2014).
Lin, P. Y. et al. Non-invasive optical measurement of cerebral metabolism and hemodynamics in infants. Journal of visualized experiments: JoVE, e4379 (2013).
Roche-Labarbe, N. et al. Noninvasive optical measures of CBV, StO(2), CBF index, and rCMRO(2) in human premature neonates’ brains in the first six weeks of life. Human brain mapping 31, 341–352 (2010).
Dehaes, M. et al. Perioperative cerebral hemodynamics and oxygen metabolism in neonates with single-ventricle physiology. Biomed Opt Express 6, 4749–4767 (2015).
Durduran, T. et al. Optical measurement of cerebral hemodynamics and oxygen metabolism in neonates with congenital heart defects. Journal of biomedical optics 15, 037004 (2010).
Buckley, E. M. et al. Validation of diffuse correlation spectroscopic measurement of cerebral blood flow using phase-encoded velocity mapping magnetic resonance imaging. Journal of biomedical optics 17, 037007 (2012).
Buckley, E. M. et al. Early postoperative changes in cerebral oxygen metabolism following neonatal cardiac surgery: effects of surgical duration. The Journal of thoracic and cardiovascular surgery 145, 196–203 (2013).
Murkin, J. M. Cerebral autoregulation: the role of CO2 in metabolic homeostasis. Seminars in cardiothoracic and vascular anesthesia 11, 269–273 (2007).
Murkin, J. M., Farrar, J. K., Tweed, W. A., McKenzie, F. N. & Guiraudon, G. Cerebral autoregulation and flow/metabolism coupling during cardiopulmonary bypass: the influence of PaCO2. Anesth Analg 66, 825–832 (1987).
Dexter, M. D. P. F. & Hindman, M. D. B. J. Theoretical Analysis of Cerebral Venous Blood Hemoglobin Oxygen Saturation as an Index of Cerebral Oxygenation during Hypothermic Cardiopulmonary BypassA Counterproposal to the “Luxury Perfusion” Hypothesis. Anesthesiology 83, 405–412. (1995).
Andropoulos, D. B., Stayer, S. A., McKenzie, E. D. & Fraser, C. D. Jr. Novel cerebral physiologic monitoring to guide low-flow cerebral perfusion during neonatal aortic arch reconstruction. The Journal of thoracic and cardiovascular surgery 125, 491–499 (2003).
Kussman, B. D. et al. Cerebral oximetry during infant cardiac surgery: evaluation and relationship to early postoperative outcome. Anesth Analg 108, 1122–1131 (2009).
Daubeney, P. E. et al. Cerebral oxygenation measured by near-infrared spectroscopy: comparison with jugular bulb oximetry. The Annals of thoracic surgery 61, 930–934 (1996).
Bickler, P. E., Feiner, J. R. & Rollins, M. D. Factors affecting the performance of 5 cerebral oximeters during hypoxia in healthy volunteers. Anesth Analg 117, 813–823 (2013).
Elwell, C. E. & Cooper, C. E. Making light work: illuminating the future of biomedical optics. Philos. Transact. A Math. Phys. Eng. Sci. 369, 4358–4379 (2011).
Durduran, T., Choe, R., Baker, W. B. & Yodh, A. G. Diffuse Optics for Tissue Monitoring and Tomography. Reports on progress in physics. Physical Society 73 (2010).
Durduran, T. & Yodh, A. G. Diffuse correlation spectroscopy for non-invasive, micro-vascular cerebral blood flow measurement. NeuroImage 85 Pt 1, 51–63 (2014).
Diop, M., Verdecchia, K., Lee, T. Y. & St Lawrence, K. Calibration of diffuse correlation spectroscopy with a time-resolved near-infrared technique to yield absolute cerebral blood flow measurements. Biomed Opt Express 2, 2068–2081 (2011).
Diop, M., Kishimoto, J., Toronov, V., Lee, D. S. & St Lawrence, K. Development of a combined broadband near-infrared and diffusion correlation system for monitoring cerebral blood flow and oxidative metabolism in preterm infants. Biomed Opt Express 6, 3907–3918 (2015).
Jain, V. et al. Cerebral oxygen metabolism in neonates with congenital heart disease quantified by MRI and optics. Journal of cerebral blood flow and metabolism: official journal of the International Society of Cerebral Blood Flow and Metabolism 34, 380–388 (2014).
Fantini, S. et al. Frequency-domain multichannel optical detector for non-invasive tissue spectroscopy and oximetry. Optical Engineering 34, 32–42 (1995).
Wray, S., Cope, M., Delpy, D. T., Wyatt, J. S. & Reynolds, E. O. Characterization of the near infrared absorption spectra of cytochrome aa3 and haemoglobin for the non-invasive monitoring of cerebral oxygenation. Biochimica et biophysica acta 933, 184–192 (1988).
Wolthuis, R. et al. Determination of water concentration in brain tissue by Raman spectroscopy. Analytical chemistry 73, 3915–3920 (2001).
Boas, D. A. & Yodh, A. G. Spatially varying dynamical properties of turbid media probed with diffusing temporal light correlation. J. Opt. Soc. Am. A 14, 192–215 (1997).
Watzman, H. M. et al. Arterial and venous contributions to near-infrared cerebral oximetry. Anesthesiology 93, 947–953 (2000).
Acknowledgements
We are grateful to the patients and families for their participation. We thank Daniel Wigmore and Erica McDavitt for assisting with recruitment. We would also like to thank Dr. Juliette Selb for her comments on the manuscript and Dr. Erin Buckley for help with analysis. This work was supported by NIH/NICHD grants R21-HD072505 (PEG) and R01-HD076258 (PEG).
Author information
Authors and Affiliations
Contributions
S.L.F. performed the data analysis, interpreted the data and wrote the manuscript; K.Y. acquired the data, interpreted the data and wrote the manuscript; R.V. acquired the data and revised the manuscript; CGHs acquired the data and revised the manuscript; F.Y. acquired the data and revised the manuscript; C.S. assisted with the statistical analysis and revised the manuscript; D.W. assisted with the statistical analysis and revised the manuscript; H.H.C. recruited patients and revised the manuscript; J.W.N. designed the study and revised the manuscript; A.K.K. interpreted the data and revised the manuscript; M.A.F. interpreted the data, assisted with the data analysis and revised the manuscript; B.D.K. acquired the data, designed the study, interpreted the data and wrote the manuscript; P.E.G. designed the study, interpreted the data and wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
Dr. Maria Angela Franceschini holds patents on the technology used in this paper. The other authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Ferradal, S., Yuki, K., Vyas, R. et al. Non-invasive Assessment of Cerebral Blood Flow and Oxygen Metabolism in Neonates during Hypothermic Cardiopulmonary Bypass: Feasibility and Clinical Implications. Sci Rep 7, 44117 (2017). https://doi.org/10.1038/srep44117
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep44117
This article is cited by
-
The incidence, risk factors and outcomes of impaired cerebral autoregulation in aortic arch surgery: a single-center, retrospective cohort study
Journal of Cardiothoracic Surgery (2023)
-
Advanced Neuromonitoring Modalities on the Horizon: Detection and Management of Acute Brain Injury in Children
Neurocritical Care (2023)
-
Assessment of cerebral autoregulation indices – a modelling perspective
Scientific Reports (2020)
-
Resuscitating the Globally Ischemic Brain: TTM and Beyond
Neurotherapeutics (2020)
-
Regional tissue oxygenation monitoring in the neonatal intensive care unit: evidence for clinical strategies and future directions
Pediatric Research (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.