Abstract
Purpose
To evaluate the efficacy of Ahmed valve (AV) implantation in patients with uveitic glaucoma.
Methods
In total, 18 patients (19 eyes) with glaucoma secondary to chronic uveitis, who underwent AV implantation were retrospectively reviewed. Visual acuity, intraocular pressure (IOP), and glaucoma medications at the most recent examination prior to surgery, were compared with those of last postoperative examination. The surgical success was defined as IOP less than 21 mmHg and greater than 4 mmHg without loss of light perception and visually devastating complications at the last postoperative examination. Decrease in the number of glaucoma medications was also a criterion for surgical success.
Results
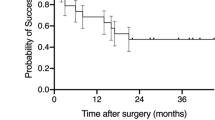
The mean follow-up period was 26±9.7 months. The mean preoperative and postoperative IOPs were 33.3±9.7 (range, 20–57) mmHg and 17.3±10.8 (range, 6–40) mmHg respectively (P<0.0001). The mean number of antiglaucoma medications was 3.5±0.8 (range, 2–5) preoperatively and 1.4±1.3 (range, 0–4) postoperatively (P<0.0001). Valve occlusion (five eyes, 26.3%) was the most commonly observed complication. Surgical success was achieved in 13 eyes (68.4%). The cumulative probability of success was 94.4% at 1 year and 60% at 2 years. Five eyes (26.3%) with IOP greater than 21 mmHg and one (5.3%) with corneal decompensation requiring penetrating keratoplasty were considered as failures.
Conclusions
The implantation of AV is an effective surgical procedure for the management of uveitic glaucoma. The inflammatory background might contribute to the occurrence of valve occlusion, which is the most common complication. Prevention of this complication is an essential factor for improving the surgical outcome.
Similar content being viewed by others
Introduction
The management of uveitic glaucoma may be difficult because of the numerous mechanisms involved in the pathogenesis.1 The condition becomes more challenging when the elevated intraocular pressure (IOP) is unresponsive to medical treatment. To improve the surgical outcome of these cases, alternative approaches such as trabeculectomy with antiproliferative agents,2, 3, 4, 5, 6, 7 aqueous drainage devices with or without trabeculectomy,8, 9, 10, 11, 12, 13, 14 trabeculodialysis,15, 16 and transscleral diode laser cyclophotocoagulation17 have been proposed. Most studies suggest using antiproliferative agents in terms of long-term IOP control in those patients.4, 6 Stavrou and Murray18 observed a high rate of trabeculectomy survival (53%) after 5 years without antiproliferatives. A higher success rate (67%) at 5 years was obtained by Towler et al6 by using intraoperative 5-fluorouracil. However, even with adjunctive antiproliferative use, increased inflammatory cells and fibroblasts in uveitic patients result in significant inflammatory response and excessive fibrosis. Furthermore, antiproliferative agents have potential complications such as corneal epithelial defects, increased incidence of bleb rupture, late bleb leak, bleb-related endophthalmitis, and chronic hypotony.10 To minimize these complications and the risk of trabeculectomy failure due to excessive scarring and fibrosis, shunting devices may be considered as a primary surgical procedure for IOP control in uveitic patients.
Postoperative hypotony and related complications appear to be less frequent in Ahmed valve (AV) implant, which has a one-way valve mechanism, compared to other valved and nonvalved drainage devices. The immediate postoperative IOP has been found to be much more predictable with this valve.19 The present study evaluates the efficacy of AV implantation, mostly as a primary glaucoma surgery in patients with uveitic glaucoma.
Patients and methods
The records of 18 patients (19 eyes) with glaucoma secondary to chronic uveitis, who underwent AV implantation (Figure 1) between March 2000 and April 2002 and had at least 6 months of follow-up, were retrospectively reviewed. All eyes had glaucoma, which could not be controlled by medications and/or previous glaucoma surgery.
The biomicroscopic and fundoscopic evaluation, visual acuity assessment, IOP measurement with applanation tonometry were performed at each preoperative and postoperative visit. Visual acuity, IOP, and glaucoma medications at the most recent examination prior to surgery were recorded and compared with those of last postoperative examination.
The surgery was performed by the same surgeon (JD). Following topical anaesthesia with tetracaine, 2 cm3 of xylocaine 2% was injected subconjunctivally. The superotemporal quadrant was preferred in all cases and a limbal conjunctival incision was performed. The sclera was exposed by blunt dissection and hemostasis was obtained with wet field cautery. A single plate, silicone AV implant (Model S-2, New World Medical, Rancho Cucamonga, CA, USA) was used in all cases. Before the implantation, AV was tested and primed by using balanced salt solution (BSS). The tube was trimmed to extend 1–2 mm beyond the limbus. A side port was created temporally in order to inject a viscoelastic material. The valve plate was secured 9–10 mm posterior to the limbus with two 9–0 nylon sutures. Parallel to the iris plane, a 23-gauge needle was used to enter the anterior chamber at the limbus. Then the tube was inserted into the anterior chamber through this needle track and secured to the sclera with one 8-0 vicryl suture. A scleral patch graft was prepared using a 7-mm corneal trephine and sutured to cover the drainage tube with four interrupted 8-0 vicryl sutures. The conjunctiva was then closed with 8-0 vicryl sutures. All patients were given 1 g of intravenous methylprednisolone intraoperatively and topical corticosteroids and antibiotics postoperatively.
Postoperative evaluation was scheduled according to the patient's clinic. The general concept was to see the patient 1 day, 1 week, 1 month, and 3 months after the surgery and then every 3 months. IOP and glaucoma medications were recorded at each visit. The surgical success was defined as IOP less than 21 mmHg and greater than 4 mmHg without loss of light perception (LP) and visually devastating complications at the last postoperative examination. Decrease in the number of glaucoma medications was also a criterion for surgical success.
The Student's t-test and Mann–Whitney U-test were used to compare preoperative and postoperative IOPs and the number of medications. P-values less than 0.05 level were considered significant. The cumulative probability of success was analysed by Kaplan–Meier life-table analysis.
Results
Of the patients, 11 (61.1%) were women and seven (38.9%) were men. The mean age was 43.4±17.2 (range, 12–72) years and the mean follow-up period was 26±9.7 (range, 7–43) months. All patients but one had follow-up period longer than 12 months. The age, sex, follow-up period, diagnosis, laterality, previous surgeries, preoperative and postoperative IOP, visual acuity, number of medications, and surgical complications for each patient are summarized in Table 1. The uveitic etiologies were idiopathic in five eyes of which two had neovascular glaucoma (NVG) (26.3%), juvenile rheumatoid arthritis in five eyes (26.3%), Fuch's heterochromic iridocyclitis in four eyes (21%), herpetic keratouveitis in three eyes (15.8%), ankylosing spondylitis in one eye (5.3%), and Chron's disease in one eye (5.3%). A total of 14 eyes (73.7%) underwent an intraocular surgery prior to AV implantation. A previous filtering surgery was performed in only three eyes. The implantation of AV was the primary glaucoma surgery in remaining 16 eyes.
The mean preoperative and postoperative IOPs were 33.3±9.7 (range, 20–57) mmHg and 17.3±10.8 (range, 6–40) mmHg respectively. Thus, a mean decrease of 16 mmHg was achieved. This decrease was statistically significant (P< 0.0001). The mean IOPs at various times after the implantation of AV are shown in Table 2. The lowest mean IOP (12.1±10.8 mmHg) was achieved at the first postoperative day. From postoperative first month to the end of follow-up period (26 months), the mean IOP did not show a significant difference (P>0.1 to P>0.5).
The mean number of antiglaucoma medications used was 3.5±0.8 (range, 2–5) preoperatively and 1.4±1.3 (range, 0–4) postoperatively (P<0.0001). The IOP was postoperatively controlled without medication in six eyes (31.6%) and with one antiglaucoma medication in five eyes (26.3%).
The visual acuity ranged from LP to 20/20 prior to surgery. Even though the range stayed the same after surgery, the visual acuity had improved more than one line in three eyes (15.8%), decreased more than one line in five eyes (26.3%), and not changed in 11 eyes (57.9%).
The complications that we observed were valve occlusion (five eyes, 26.3%), hypotony which resolved spontaneously within postoperative 3 days (three eyes, 15.8%), choroidal detachment which resolved with oral corticosteroids treatment within 10 days (one eye, 5.3%), hyphema which resolved spontaneously within 5 days (one eye, 5.3%), and corneal decompensation due to corneal-tube touch which required shortening of the tube and then penetrating keratoplasty (one eye, 5.3%). One of the occluded valves was also extruded from the conjunctiva and had been removed. Occluded valves were irrigated with BSS (two eyes), fenestrated with Nd:YAG laser (one eye), or replaced (one eye). The irrigation of the valve worked well and IOP stayed under control in one eye. The eye that underwent valve replacement achieved an IOP control without medication following the second operation and was considered successful. Thus, the valve occlusion was finally observed in overall three eyes (15.8%) of which two had NVG and one had glaucoma secondary to JRA associated uveitis. The eye with NVG, in which we removed the valve because of valve occlusion and extrusion, lost the LP within few weeks after valve removal and was associated with pain and uncontrolled inflammation. An evisceration of this eye was performed.
According to the described criteria, a successful outcome was achieved in overall 13 out of 19 eyes (68.4%). The cumulative probability of success was 94.4% at 1 year, 88.9% at 18 months, and 60% at 2 years. Of the six eyes that were considered as failures, five (83.3%) had IOP greater than 21 mmHg and one (16.7%) had corneal decompensation requiring penetrating keratoplasty. Out of 5 eyes with IOP greater than 21 mmHg, two had NVG, two had herpetic keratouveitis, and one had JRA associated uveitis.
Data comparing preoperative and postoperative periods are shown in Table 3.
Discussion
It is widely accepted that surgical success of uveitic glaucoma differs from other cases of glaucoma. Considering the fact that initially successful glaucoma procedures usually end in failure due to fibrosis,10 the threshold for glaucoma drainage device (GDD) implantation might be lower in uveitic cases. GDD implantation is an appropriate primary surgical procedure in particularly glaucoma secondary to JRA associated uveitis,20 which made up 26.3% of our patients.
Owing to its unidirectional valve mechanism preventing early postoperative hypotony and related complications, AV implant is one the most commonly used glaucoma implants worldwide. The study of Taglia et al21 comparing the AV, the Krupin eye valve with disc and double-plate Molteno implant demonstrated that the AV implant is less likely to create problems leading to reoperations or visual acuity loss. A significant amount of IOP decrease has been reported in all studies evaluating AV implant's success.9, 10, 11, 19, 22, 23 In large and heterogeneous series of glaucoma treated with AV implantation, a mean decrease of 16.8 mmHg in IOP and a decrease of 1.6 in the number of antiglaucoma medications were achieved. A success rate of 87% at 1 year and 75% at 2 years after surgery were reported.22 Cumulative probabilities of success were reported as 87, 82, 76, and 76% at 1, 2, 3, and 4 years, respectively, in a study of Topouzis et al23 evaluating long-term results of AV implant in complicated glaucoma cases.
Regarding the use of GDD in uveitic glaucoma, Molteno et al13 recently reported a success rate of 76% for the long-term IOP control. A success rate of 79% 2 years after Molteno implantation have been reported by Hill et al. Additionally, they emphasized that in situations with marked inflammation, Molteno implant achieved a higher success rate comparing to trabeculectomy.8 On the other hand, a relatively high rate of complications such as peripheral choroidal effusion, shallow anterior chamber, hypotony, and obstruction of the tube have been reported with Molteno implant.24 Success rate of Baerveldt implant at 2-year follow-up was 60% in uveitic group consisted of five patients only.14 There are few studies that have evaluated the efficacy of AV in uveitic glaucomas. Gil-Carasco et al successfully treated eight of 14 uveitic eyes (57%) with AV implantation over an average follow-up period of 14 months. IOP was reduced from a mean of 32.6 mmHg with 2.8 antiglaucoma medications preoperatively to 17.6 mmHg with 0.7 antiglaucoma medications postoperatively.9 A surgical success was achieved in 13 of 19 eyes (68.4%) in our series, within an average follow-up period of 26 months. Five eyes (26.3%) having postoperative IOP greater than 21 mmHg and one (5.3%) having corneal decompensation due to corneal-tube touch were considered as failures. IOP was reduced from a mean of 33.3 mmHg to a mean of 17.3 mmHg with a mean pressure reduction of 16 mmHg (P<0.0001). The average number of medications required was reduced from 3.5 to 1.4 (P<0.0001) and the number of eyes requiring no medication was six (31.6%). De Mata et al obtained a success rate of 93%10 and 94%11 at 1 year with AV implantation. The average pressure reduction was 21.4 mmHg10 and 23.7 mmHg11 and the average number of medications required was 0.710 and 0.611 after surgery. In total, 60–67% of the eyes required no medications. They suggested that AV implantation may be more effective than trabeculectomy in uveitic glaucoma.10, 11 Even though the cumulative probability of success at 1 year (94.4%) was similar to that of De Mata et al's study;11 the cumulative probability of success at 2 years (60%) was relatively low in our study.
Morgan et al reported a complication rate of 47% of which corneal oedema (13%) and obstruction of the tube (11%) were the most common. A transient hypotony (8%) and shallow anterior chamber which does not require additional surgery (8%) were less common.22 In cases with uveitic glaucoma, the most common complications of AV implant were encapsulated bleb and transient hypotony (42.8% for each).9 In our series, postoperative complications were observed in 11 (57.9%) eyes. The majority of these complications were resolved either spontaneously or with additional surgical procedure. Occlusion of the valve was the most common complication and occurred in five eyes, (26.3%) in which one additionally had extrusion of the valve. In one of these eyes, AV implant was replaced and the second implant worked successfully. Another one was treated with irrigation of the implant. The remaining three eyes in which two had NVG were considered as failure. A success rate in eyes with NVG has been reported to be significantly lower.22 Occlusion of the AV may occur secondary to haemorrhage, posterior capsule, iris, or vitreous blocking the tube or may be related to fibrovascular ingrowth between the AV plate and the valve cover housing.25 Another complication that required additional surgery was corneal decompensation due to corneal-tube touch and was observed in one eye (5.3%). A penetrating keratoplasty was performed in this eye. Corneal-tube touch occurred in 5% of eyes in Huang et al's study.22 This complication is mostly common in pediatric patients and its rate has been reported to be 18.5%.26 Choroidal effusion was observed in one (5.3%) and treated with systemic corticosteroid. Other complications such as hyphema (5.3%) and postoperative hypotony (15.8%) were resolved spontaneously within few days. Hypertensive phase, which has been reported to occur within postoperative 6 months,27 did not occur in our series. The mean postoperative IOP was significantly lower at all follow-up intervals. Reported complications such as motility disturbance, encapsulated bleb, shallow anterior chamber, pupillary block, retinal detachment, and suprachoroidal haemorrhage were not encountered in our patients.19, 22, 23
As a conclusion, the implantation of AV is an effective surgical procedure in the management of uveitic glaucoma and is associated with relatively few complications. Although most of our cases were high-risk patients with chronic uveitis and many of whom had already operated for diverse causes, a surgical success of 68.4% was achieved within an average of 26 months follow-up. The highest probability of success (94.4%) was attained at 1 year and decreased with time. The most common complication leading to surgical failure was the occlusion of the valve. The inflammatory background of our cases might contribute to the occurrence of this complication. Further investigations on pathophysiology of AV occlusion and prevention of this complication including the use of pharmacological agents are needed to improve the surgical outcome.
References
Moorthy RS, Mermoud A, Baerveldt G, Minckler DS, Lee PP, Rao NA . Glaucoma associated with uveitis. Surv Ophthalmol 1997; 41: 361–394.
Jampel HD, Jabs DA, Quigley HA . Trabeculectomy with 5-fluorouracil for adult inflammatory glaucoma. Am J Ophthalmol. 1990; 109: 168–173.
Kitazawa Y, Kawase K, Matsushita H, Minobe M . Trabeculectomy with mitomycin. A comparative study with fluorouracil. Arch Ophthalmol 1991; 109: 1693–1698.
Patitsas CJ, Rockwood EJ, Meisler DM, Lowder CY . Glaucoma filtering surgery with postoperative 5-fluorouracil in patients with intraocular inflammatory disease. Ophthalmology 1992; 99: 594–599.
Prata Jr JA, Neves RA, Minckler DS, Mermoud A, Heuer DK . Trabeculectomy with mitomycin C in glaucoma associated with uveitis. Ophthalmic Surg 1994; 25: 616–620.
Towler HM, McCluskey P, Shaer B, Lightman S . Long-term follow-up of trabeculectomy with intraoperative 5-fluorouracil for uveitis-related glaucoma. Ophthalmology 2000; 107: 1822–1828.
Ceballos EM, Beck AD, Lynn MJ . Trabeculectomy with antiproliferative agents in uveitic glaucoma. J Glaucoma 2002; 11: 189–196.
Hill RA, Nguyen QH, Baerveldt G, Forster DJ, Minckler DS, Rao N et al. Trabeculectomy and Molteno implantation for glaucomas associated with uveitis. Ophthalmology 1993; 100: 903–908.
Gil-Carrasco F, Salinas-VanOrman E, Recillas-Gispert C, Paczka JA, Gilbert ME, Arellanes-Garcia L . Ahmed valve implant for uncontrolled uveitic glaucoma. Ocul Immunol Inflamm 1998; 6: 27–37.
Da Mata AP, Foster CS . Ahmed valve and uveitic glaucoma. Int Ophthalmol Clin 1999; 39: 155–167.
Da Mata A, Burk SE, Netland PA, Baltatzis S, Christen W, Foster CS . Management of uveitic glaucoma with Ahmed glaucoma valve implantation. Ophthalmology 1999; 106: 2168–2172.
Ceballos EM, Parrish II RK, Schiffman JC . Outcome of Baerveldt glaucoma drainage implants for the treatment of uveitic glaucoma. Ophthalmology 2002; 109: 2256–2260.
Molteno AC, Sayawat N, Herbison P . Otago glaucoma surgery outcome study: long-term results of uveitis with secondary glaucoma drained by Molteno implants. Ophthalmology 2001; 108: 605–613.
Krishna R, Godfrey DG, Budenz DL, Escalona-Camaano E, Gedde SJ, Greenfield DS et al. Intermediate-term outcomes of 350-mm(2) Baerveldt glaucoma implants. Ophthalmology 2001; 108: 621–626.
Kanski JJ, McAllister JA . Trabeculodialysis for inflammatory glaucoma in children and young adults. Ophthalmology 1985; 92: 927–930.
Williams RD, Hoskins HD, Shaffer RN . Trabeculodialysis for inflammatory glaucoma: a review of 25 cases. Ophthalmic Surg 1992; 23: 36–37.
Schlote T, Derse M, Zierhut M . Transscleral diode laser cyclophotocoagulation for the treatment of refractory glaucoma secondary to inflammatory eye diseases. Br J Ophthalmol. 2000; 84: 999–1003.
Stavrou P, Murray PI . Long-term follow-up of trabeculectomy without antimetabolites in patients with uveitis. Am J Ophthalmol 1999; 128: 434–439.
Coleman AL, Hill R, Wilson MR, Choplin N, Kotas-Neumann R, Tam M et al. Initial clinical experience with the Ahmed glaucoma valve implant. Am J Ophthalmol 1995; 120: 23–31.
Valimaki J, Airaksinen PJ, Tuulonen A . Molteno implantation for secondary glaucoma in juvenile rheumatoid arthritis. Arch Ophthalmol 1997; 115: 1253–1256.
Taglia DP, Perkins TW, Gangnon R, Heatley GA, Kaufman PL . Comparison of the Ahmed glaucoma valve, the Krupin eye valve with disk, and the double-plate Molteno implant. J Glaucoma 2002; 11: 347–353.
Huang MC, Netland PA, Coleman AL, Siegner SW, Moster MR, Hill RA . Intermediate-term clinical experience with the Ahmed glaucoma valve implant. Am J Ophthalmol 1999; 127: 27–33.
Topouzis F, Coleman AL, Choplin N, Bethlem MM, Hill R, Yu F et al. Follow-up of the original cohort with the Ahmed glaucoma valve implant. Am J Ophthalmol 1999; 128: 198–204.
Melamed S, Cahane M, Gutman I, Blumenthal M . Postoperative complications after Molteno implant surgery. Am J Ophthalmol 1991; 111: 319–322.
Hill RA, Pirouzian A, Liaw L . Pathophysiology of and prophylaxis against late Ahmed glaucoma valve occlusion. Am J Ophthalmol 2000; 129: 608–612.
Englert JA, Freedman SF, Cox TA . The Ahmed valve in refractory pediatric glaucoma. Am J Ophthalmol 1999; 127: 34–42.
Ayyala RS, Zurakowski D, Smith JA, Monshizadeh R, Netland PA, Richards DW et al. A clinical study of the Ahmed glaucoma valve implant in advanced glaucoma. Ophthalmology 1998; 105: 1968–1976.
Acknowledgements
We have not received any public or private support in the preparation of the paper. This paper does not serve the financial or proprietary interests of any individuals or institutions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Özdal, P., Vianna, R. & Deschênes, J. Ahmed valve implantation in glaucoma secondary to chronic uveitis. Eye 20, 178–183 (2006). https://doi.org/10.1038/sj.eye.6701841
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701841
Keywords
This article is cited by
-
Long-term surgical outcomes of Ahmed valve implantation in refractory glaucoma according to the type of glaucoma
BMC Ophthalmology (2022)
-
Assessing risk factors for postoperative hypotony in Ahmed glaucoma valve implantation surgery
International Ophthalmology (2021)
-
Evaluation of the outcome of long-tube shunt implant surgery in uveitic glaucoma patients by analyzing the background of uveitis
International Ophthalmology (2021)
-
Comparison of surgical outcomes of trabeculectomy, Ahmed shunt, and Baerveldt shunt in uveitic glaucoma
Journal of Ophthalmic Inflammation and Infection (2018)