Abstract
STAT3 has been known as a mediator for gene expression induced by many important cytokines. Recent studies have suggested that STAT3 has important functions in regulation of both innate and adaptive immunity. Loss of STAT3 in immune cells caused severe inflammation in response to pathogens. This review discusses the recent progress and suggests directions for the future research on this interesting molecule.
Similar content being viewed by others
The STAT signaling pathway
It is known that growth factors or cytokines can activate signaling cascades 1. For example, many growth factor receptors are associated with, or have intrinsic tyrosine kinase activity. Through some adapters, activation of tyrosine kinases can further signal to the Ras protein, then to downstream serine/threonine kinases, such as the members of MAP kinase family. These serine/threonine kinases in turn can stimulate effectors such as transcription factors in the cytoplasm and nucleus. A vast amount of evidence indicates that both the second messenger and kinase cascade pathways play important roles in mediating intracellular signal transduction.
The STAT proteins initially recognized in the interferon system 2, 3, 4, 5, 6. JAK belongs to a family protein tyrosine kinases that are activators of STAT proteins 7, 8, 9. STAT proteins can interact with the receptor/tyrosine kinase complex through its SH2 domain 10, 11, 12. Many cytokines beside IFNs can activate STAT proteins to regulate gene expression 13, 14, 15. In addition to JAK kinase, a variety of tyrosine kinases, such as Src, and EGF receptor tyrosine kinase have been found to activate STAT proteins 16, 17, 18, 19. Therefore, STAT proteins mediate downstream signal transduction of a variety of protein tyrosine kinases (PTKs) 14. Studies from our laboratory showed that STAT proteins are regulators of cell growth and apoptosis through regulation of p21 and caspases 19, 20, 21 . Many other laboratories have further shown that cyclins and the Bcl-2 family of proteins may also be regulated by STAT proteins (reviewed in 14, 22). STAT proteins are also known to be involved in tumorigenesis 15, 18, 23.
STATs are major mediators of signaling during immune responses, and also have roles in development and cell differentiation 14, 19, 22, 24, 25, 26. It is well established that many cytokines and STATs are involved in multiple steps in adaptive immune responses 15. For example, STAT4 knockout mice have normal hematopoiesis, but are unable to respond to IL-12: IL-12-induced mitogenesis and enhancement of natural killer cytolytic function are defective. Most interestingly, T cell differentiation is affected by STAT4 mediated IL-12 signaling: Th1 differentiation is abrogated in STAT4-deficient mice 27, 28. Additionally, STAT1 is essential for the function of IFN-γ as well as Th1 cell differentiation 15, 29, 30. It was also reported recently that STAT1 is involved in Inflammatory bowel disease (IBD) 31.
Inflammatory bowel disease (IBD): Breakdown of immune tolerance
The innate immune system initiates immediate host responses to microbial antigens and acts as an effector by stimulating adaptive immune responses 32. The mucosal immune system in the digestive tract is among the first lines of defense against microbial pathogens, which involves both innate and adaptive immune responses 33. The digestive tract is not normally affected by inflammation despite its exposure to many diverse foreign antigens, indicating that there must be an essential mechanism that can suppress initiation of inflammation by enabling the mucosal immune system to tolerate foreign antigens. One important question is how the mucosal immune system in the gastrointestinal tract responds to a variety of antigens and how the decision is made between tolerance and antigen clearance. Disruption of this balance can lead to disorders in the mucosal immune system that cause severe human diseases 34.
For example, in Crohn's disease (CD) and other IBD such as colitis, chronic inflammation can occur in parts of the gastrointestinal tract. Molecular etiopathology of Crohn's disease and other IBDs have been extensively studied, and abnormalities in both innate and adaptive immune responses have been suggested 33, 35, 36. It is likely that the loss of tolerance and uncontrolled responses to microbial antigens in the mucosal immune system is a major cause of Crohn's disease and other IBDs 37. Recently, several groups have shown that the NOD2 gene on chromosome 16 is implicated in Crohn's disease 38, 39, 40. NOD2 is a member of a new gene family that may mediate response to bacterial LPS and other innate signals 41, 42, 43. Thus disruption of the innate immune response is a key factor in Crohn's disease. NOD2 is expressed in monocytes and in intestinal epithelial cells (IECs) but is most strongly expressed in Paneth cells in the terminal ileum. The NOD2 gene is expressed in monocytes, but not in lymphocytes 39, suggesting specific abnormalities of myeloid cells have decisive functions in the development of Crohn's disease. Furthermore, Crohn's disease is a complex disorder of the gut that appears to involve several associated genetic susceptibility factors, priming by the enteric microflora, and immune-mediated tissue injury 37, 44, 45. The disease is distinguished from ulcerative colitis, by its earlier onset (average age of diagnosis is 18 years), and by the non-colon-specific granulomatous inflammation affecting any part of the gastrointestinal tract but particularly the ileocecal area. The two diseases also differ in their response to therapy: TNF-α blockade usually yields an excellent response in Crohn's disease 46, 47.
It is well established that cytokines such as TNF-α and IFN-γ are of crucial importance in the normal homeostasis of the mucosal immune system and pathogenesis of CD/IBDs 33, 48. In particular, cytokines involved in Th1 differentiation may have a very critical role. A typical phenotype in IBDs in either human or mouse, is an exaggerated Th1 type response with excess generation of IFN-γ and TNF-α, which may result in tissue injury 33, 49, 50, 51, 52, 53, 54. Th1 cells are induced by the differentiation of activated T-cells in the presence of IL-12. During a balanced response, these effector T-cells are inhibited by IL-10-dependent regulatory T-cells 54. Th1 cells are a major source of IFN-γ and activate cytotoxic T-cells. Thus, changes affecting the interplay between effector and regulatory T-cells could cause tissue-damage during IBD, and progression and chronic inflammation of Crohn's disease requires the adaptive immune system 45, 49. The major questions in IBDs include how antigen/pathogen is presented by APCs, such as by dendritic cells, and whether there is a co-ordinate mechanism regulating signals from DCs to T regs and T reactive/effector cells. These two questions are important not only for understanding mechanisms of IBDs, but also for most inflammatory disorders. The major focus of our current research is to address these two questions about how mucosal immune tolerance is systematically regulated by STAT3, possibly through dendritic cells and T regulatory cells.
It is interesting to note that STAT3 was also found to be highly tyrosine phosphorylated in epithelial and lamina propria cells of human ulcerative colitis and Crohn's disease patients as well as in dextran sulfate sodium (DSS)-induced colitis in mice 55, possibly indicating a potential role of STAT3 in epithelial cells during colitis generation.
STAT3, initiation of inflammation and mammalian disorders involving cytokines
STAT3 was originally discovered as a transcription factor activated by IL-6 family cytokines through gp130 56, 57. The IL-6 receptor system consists of two chains: the 80 kD IL-6 receptor for ligand binding and a 130 kD co-receptor (gp130) for signal transduction. It is clear that this gp130 signaling chain is used in signal transduction by several other members of this cytokine family including IL-6, LIF, CT-1, oncostatin M (OSM), ciliary neurotrophic factor (CNTF) and IL-11 58. These cytokines are believed to play roles in development and normal functions of some important organs and tissues, such as heart, liver and lymphocyte differentiation. For example, disruption of gp130 leads to disorders in these systems and causes embryonic lethality 59. Interestingly, more and more evidence have implicated STAT3 in myeloid differentiation. A number of cytokines, such as G-CSF and GM-CSF, which act in part through activation of the STAT3, are involved in myeloid differentiation. Thus STAT3 may have many important functions for hematopoiesis and immune responses.
Since classical knock-out (KO) of the STAT3 gene in mice resulted in early embryonic lethality 59, it was difficult to study physiological roles of STAT3 in mouse models. Various cell type specific STAT3 knockouts have been established including T-cells 60 and keratinocytes 61. Loss of STAT3 has been shown to increase sensitivities to apoptosis and certain defect in wound healing. Takeda et al. 62 also deleted the STAT3 gene from macrophages and neutrophils by using the macrophage-specific lysozyme promoter. STAT3 ablation in these mice results in an increased sensitivity to endotoxin/LPS shock, chronic inflammation and chronic enterocolitis with age. These mice have an over-abundance of pro-inflammatory cytokines. Th1 activity was enhanced. The phenotypes of this enterocolitis have been attributed to a block in the IL-10 signaling pathway: Only in the presence of STAT3 did IL-10 down regulate inflammatory cytokine TNF-α in macrophages 63. Th1 activity was over-activated, although IL-10-dependent regulatory T-cells are expected to be normal in these mice, implying that the possible limitations of this system. It is likely that other cells such as dendritic cells, are also involved in directing regulatory T-cells in this regulation of Th1 cells.
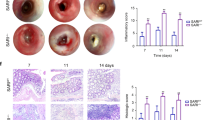
In my laboratory, we have obtained conditional and tissue specific STAT3 null mice. Our evidence has shown that one strain of mice with bone marrow cell specific STAT3 KO have developed IBD/Crohn's disease (CD)-like pathogenesis 64. Importantly, STAT3 deletion in dendritic cells in our mice may also have contributed in the development of these syndromes of inflammation. I believe that these mice provide a useful in vivo model system for studies of pathogenesis of inflammatory disorders and the molecular mechanism of regulation of both innate and adaptive immunity, which involve macrophages as well as dendritic cells.
The NOD2 and IL-10 genes and inflammatory bowel diseases
A number of animal models dealing with IBDs have been previously established (recently reviewed in 65). As mentioned above, mutations in the gene encoding NOD2 result in susceptibility to Crohn's disease, particularly small intestinal disease 38, 39. Recently, three groups have generated mice with deletions or mutations in the NOD2 gene (reviewed in 65). Intriguingly, none of these mouse strains developed spontaneous intestinal inflammation. Even more puzzling, some of these mutant mice exhibit increased NF- B activation in response to MDP, a NOD2 ligand, which appeared to be an opposite result from what had been reported in the mice with an absence of NOD2. Recent data derived from one of the NOD2 strains have implicated an interaction between TLR2 and NOD2 as a potential explanation for the association of NOD2 and IBD.
A more interesting model of IBD is IL-10-deficient mice 66. IL-10 is believed to be generated by regulatory T cells and plays a major role in immune suppression. IL-10 is also expressed in B cells, dendritic cells, and macrophages 67. IL-10-deficient mice develop anemia, growth retardation, and chronic IBD with transmural leukocyte infiltration 66. It was shown that over-produced IL-12, IFN and polarized Th1 cell activation are major mediators of inflammation in IL-10 deficient mice. When IL-10-deficient mice are raised under germ-free conditions, IBD does not occur, indicating the importance of innate interactions. A seminal finding by Akira's group revealed that STAT3 is the mediator of IL-10 for immune suppression 62. However, the detailed mechanism is unclear. Thus, to further study mechanisms of immune suppression by IL-10, we have to address the question about how STAT3 is functioning in immune tolerance. I expect that this line of important investigations will be a direction for the future research.
The roles of T regulatory cells and dendritic cells in IBDs and immune tolerance
As discussed above, IBDs, including Crohn's disease and ulcerative colitis, are resulted from breakdown of mucosal immune tolerance 33, 54, 65. Loss of immune tolerance may occur when self-reactive lymphocytes are not eliminated or inactivated during their development. In particular, a deregulated CD4 T cell response to a variety of antigens in the lumen may be responsible for chronic inflammation 33, 68. Activation and expansion of self-reactive T lymphocytes can be suppressed in the periphery by CD4+CD25+ T regulatory cells (T regs). The majority of T regs constitutively expresses CD25 (IL-2 receptor α-chain) 69. CD25+CD4+ T regs can be produced by the thymus as a functionally mature T cell subpopulation, and their defects could lead to the development of various organ-specific autoimmune diseases. T regs are also believed to maintain a balanced response to environmental antigens, thereby, preventing IBD and allergy in rodents 54. A striking example of T regs in IBD was shown when adoptive transfer of T regs can “cure” a kind of induced colitis 70. Further understanding of the biology of T regs and the mechanisms that control T regs differentiation may be of key importance for the development of new therapeutic strategies.
Besides T regs, dendritic cells (DCs) also play essential roles in both immune responses and tolerance 71, 72. The primary function of dendritic cells is thought as antigen presentation, and to play a pivotal role at the intersection of innate and adaptive immunity. Recent data have shown that DCs can determine whether non-responsiveness (tolerance) or an active immune response occurs. Similarly intestinal DCs are critical for regulation of immune reaction or tolerance in the gut. The balanced actions of DCs in tolerance and active immunity to bacterial flora in the gut may be required for a healthy condition, while loss of DC mediated tolerance results in inflammatory responses, including Crohn's disease and ulcerative colitis 73.
In human peripheral blood, two major DC populations can be classified, namely CD11c+ DCs and CD11c- DCs. CD11c+ DCs are termed DC1 or myeloid DC. They express high levels of the granulocyte macrophage-colony stimulating factor (GM-CSF) receptor and respond to GM-CSF. In contrast, CD11c- DCs are designated as plasmacytoid or lymphoid DC 74. They express high levels of IL-3 receptor (CD123) but little GM-CSF receptor and require activation before displaying characteristic stimulatory activity in vitro. They are sometimes called precursors of DC2 (pDC2) because of their relative immaturity 73. However, mice are somewhat different: there are three major DC populations, myeloid, plasmacytoid and "lymphoid" DCs. All mouse DCs are CD11c+. DC differentiation from hematopoietic precursors has been extensively examined using in vitro systems. DC progeny generated in vitro by GM-CSF or Flt3L are now well defined: DC derived from GM-CSF-supplemented cultures express cell surface antigens typically associated with CD11c+ CD11b+, or called “myeloid” DC 75, while DC derived from Flt3L-supplemented cultures exhibit characteristics typically associated with plasmacytoid CD11c+ CD11b- DC (pDC) 76, 77. In my laboratory we have used this approach and directly compared the activity of Flt3L versus GM-CSF on DC differentiation in the absence of STAT3 and we will continue this line of investigation.
Different DC subsets are thought to have particular functions, such as Th1/Th2 differentiation or tolerance induction. An important cytokine generated by pDC is type1 interferons (IFN-α/β), which become a characteristic of plasmacytoid DC in both humans and mice 78, 79, 80. Mouse lymphoid DC population is characterized by expression of a homodimer of the CD8 molecule. In contrast to pDC, murine CD8+ DC is associated with elevated IL-12 production and the following induction of IFN-γ, leading to differentiation of Th1 cells 81, 82. Understanding how these DC subsets are differentiated should provide critical information on how immune tolerance is maintained or getting breakdown in mucosal immunity. However, little was known about how these subsets of DCs are generated until recently. It is interesting to point out that we have recently shown that in the mice with STAT3 knock out in bone marrow cells, IL-12 and IFN-γ were all elevated 64, which resembles possible selective activation of CD8+ DCs. or /and absence of pDCs 83. We found that STAT3 is an essential factor for DC differentiation in response to Flt3L. We have demonstrated that loss of STAT3 in DCs blocked Flt3, but not GM-CSF signaling for DC differentiation, which consequently significantly affects T cell differentiation and activation (unpublished results). In consistency with this idea, a recent report revealed that STAT3 in DCs is involved in production of T regs during tumorigenesis 84.
In the future, it is necessary to continue our studies on roles of STAT3 in DC differentiation and T cell function, and to define mechanisms of STAT3-controlled regulatory events in immune tolerance. The key is to reveal how STAT3 controls the immunity through DCs or T regs. It is warranted that there will be more data supporting the hypothesis and concept that STAT3 mediates function and differentiation of T regs and DCs that are responsible for maintaining intestinal immune homeostasis.
References
Schlessinger J, Ullrich A . Growth factor signaling by receptor tyrosine kinases. Neuron 1992; 9:383–391.
Levy DE, Kessler DS, Pine R, Reich N, Darnell JE Jr. Interferon-induced nuclear factors that bind a shared promoter element correlate with positive and negative transcriptional control. Genes Dev 1988; 2:383–93.
Dale TC, Imam AMA, Kerr IM, Stark GR . Rapid activation by interferon-a of a latent DNA-binding protein present in the cytoplasm of untreated cells. Proc Natl Acad Sci 1989; 86:1203–7.
Fu XY, Schindler C, Improta T, Aebersold R, Darnell JE Jr. The proteins of ISGF-3, the interferon alpha-induced transcriptional activator, define a gene family involved in signal transduction. Proc Natl Acad Sci U S A 1992; 89:7840–3.
Schindler C, Fu XY, Improta T, Aebersold R, Darnell JE Jr. Proteins of transcription factor ISGF-3: one gene encodes the 91-and 84-kDa ISGF-3 proteins that are activated by interferon alpha. Proc Natl Acad Sci U S A 1992; 89:7836–9.
Darnell JE Jr, Kerr IM, Stark GR . Jak-STAT pathways and transcriptional activation in response to IFNs and other extracellular signaling proteins. Science 1994; 264:1415–21.
Velazquez L, Fellous M, Stark GR, Pellegrini S . A protein tyrosine kinase in the interferon a/b signaling pathway. Cell 1992; 70:313–22.
Muller M, Briscoe J, Laxton C, et al. The protein tyrosine kinase JAK1 complements defects in interferon-a/b and -g signal transduction. Nature 1993; 366:129–35.
Ihle JN, Kerr IM . Jaks and Stats in signaling by the cytokine receptor superfamily. Trends Genet 1995; 11:69–74.
Fu XY . A transcription factor with SH2 and SH3 domains is directly activated by an interferon alpha-induced cytoplasmic protein tyrosine kinase(s). Cell 1992; 70:323–35.
Greenlund AC, Farrar MA, Viviano BL, Schreiber RD . Ligand-induced IFN gamma receptor tyrosine phosphorylation couples the receptor to its signal transduction system (p91). EMBO J 1994; 13:1591–600.
Stahl N, Farruggella TJ, Boulton TG, et al. Choice of STATs and other substrates specified by modular tyrosine-based motifs in cytokine receptors. Science 1995; 267:1349–53.
Larner AC, David M, Feldman GM, et al. Tyrosine phosphorylation of DNA binding proteins by multiple cytokines. Science 1993; 261:1730–3.
Darnell JE Jr. STATs and gene regulation. Science 1997; 277:1630–5.
Leonard WJ, O'Shea JJ . Jaks and STATs: biological implications. Annu Rev Immunol 1998; 16:293–322.
Fu XY, Zhang JJ . Transcription factor p91 interacts with the epidermal growth factor receptor and mediates activation of the c-fos gene promoter. Cell 1993; 74:1135–45.
Ruff-Jamison S, Zhong Z, Wen Z, et al. Epidermal growth factor and lipopolysaccharide activate Stat3 transcription factor in mouse liver. J Biol Chem 1994; 269:21933–5.
Yu CL, Meyer DJ, Campbell GS, et al. Enhanced DNA-binding activity of a Stat3-related protein in cells transformed by the Src oncoprotein. Science 1995; 269:81–3.
Su WC, Kitagawa M, Xue N, et al. Activation of Stat1 by mutant fibroblast growth-factor receptor in thanatophoric dysplasia type II dwarfism. Nature 1997; 386:288–92.
Chin YE, Kitagawa M, Su WC, et al. Cell growth arrest and induction of cyclin-dependent kinase inhibitor p21 WAF1/CIP1 mediated by STAT1. Science 1996; 272:719–22.
Chin YE, Kitagawa M, Kuida K, Flavell RA, Fu XY . Activation of the STAT signaling pathway can cause expression of caspase 1 and apoptosis. Mol Cell Biol 1997; 17:5328–37.
O'Shea JJ, Gadina M, Schreiber RD . Cytokine signaling in 2002: new surprises in the Jak/Stat pathway. Cell 2002; 109:S121–31.
Bromberg JF, Wrzeszczynska MH, Devgan G, et al. Stat3 as an oncogene. Cell 1999; 98:295–303.
Akira S . Functional roles of STAT family proteins: lessons from knockout mice. Stem Cells 1999; 17:138–46.
Fu XY . From PTK-STAT signaling to caspase expression and apoptosis induction Cell Death Differ 1999; 6:1201–8.
Levy DE, Darnell JE Jr. Stats: transcriptional control and biological impact. Nat Rev Mol Cell Biol 2002; 3:651–62.
Kaplan MH, Sun YL, Hoey T, Grusby MJ . Impaired IL-12 responses and enhanced development of Th2 cells in Stat4-deficient mice. Nature 1996; 382:174–7.
O'Shea JJ . Jaks, STATs, cytokine signal transduction, and immunoregulation: are we there yet? Immunity 1997; 7:1–11.
Durbin JE, Hackenmiller R, Simon MC, Levy DE . Targeted disruption of the mouse Stat1 gene results in compromised innate immunity to viral disease. Cell 1996; 84:443–450.
Meraz MA, White JM, Sheehan KC, et al. Targeted disruption of the Stat1 gene in mice reveals unexpected physiologic specificity in the JAK-STAT signaling pathway. Cell 1996; 84:431–42.
Schreiber S, Rosenstiel P, Hampe J, et al. Activation of signal transducer and activator of transcription (STAT) 1 in human chronic inflammatory bowel disease Gut 2002; 51:379–85.
Medzhitov R, Janeway C A, Jr. Innate immunity: the virtues of a nonclonal system of recognition Cell 1997; 91:295–8.
Strober W, Fuss I J, Blumberg R S . The immunology of mucosal models of inflammation Annual Review of Immunology 2002; 20:495–549.
Duchmann R, Kaiser I, Hermann E, Mayet W, Ewe K, Meyer zum Buschenfelde K H . Tolerance exists towards resident intestinal flora but is broken in active inflammatory bowel disease (IBD) Clinical & Experimental Immunology 1995; 102:448–55.
Hugot J P, Zouali H, Lesage S, Thomas G . Etiology of the inflammatory bowel diseases. Int J Colorectal Dis 1999; 14:2–9.
Laroux FS, Pavlick KP, Wolf RE, Grisham MB . Dysregulation of intestinal mucosal immunity: implications in inflammatory bowel disease. News Physiol Sci 2001; 16:272–7.
Shanahan F . Crohn's disease. Lancet 2002; 359:62–9.
Hugot JP, Chamaillard M, Zouali H, et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn's disease. Nature 2001; 411:599–603.
Ogura Y, Bonen D K, Inohara N, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease Nature 2001; 411:603–6.
Hampe J, Cuthbert A, Croucher PJ, et al. Association between insertion mutation in NOD2 gene and Crohn's disease in German and British populations. Lancet 2001; 357:1925–8.
Inohara N, Ogura Y, Nunez G . Nods: a family of cytosolic proteins that regulate the host response to pathogens. Curr Opin Microbiol 2002; 5:76–80.
Murray PJ . NOD proteins: an intracellular pathogen-recognition system or signal transduction modifiers? Curr Opin Immunol 2005; 17:352–8.
Cario E . Bacterial interactions with cells of the intestinal mucosa: Toll-like receptors and NOD2. Gut 2005; 54:1182–93.
Beutler B . Autoimmunity and apoptosis: the Crohn's connection. Immunity 2001; 15:5–14.
Elson CO . Genes, microbes, and T cells—new therapeutic targets in Crohn's disease. New Engl J Med 2002; 346:614–6.
Van Deventer SJ . Immunotherapy of Crohn's disease. Scand J Immunol 2000; 51:18–22.
Srivastava MD . Immunomodulatory effects of etanercept (TNFR:Fc) and its use in a patient with Crohn's disease. Res Commun Mol Pathol Pharmacol 2001; 109:125–41.
MacDonald TT . Effector and regulatory lymphoid cells and cytokines in mucosal sites. Curr Top Microbiol Immunol 1999; 236:113–35.
Blumberg RS, Strober W . Prospects for research in inflammatory bowel disease. JAMA 2001; 285:643–7.
Plevy SE, Landers CJ, Prehn J, et al. A role for TNF-alpha and mucosal T helper-1 cytokines in the pathogenesis of Crohn's disease. J Immunol 1997; 159:6276–82.
Kosiewicz MM, Nast CC, Krishnan A, et al. Th1-type responses mediate spontaneous ileitis in a novel murine model of Crohn's disease. J Clin Invest 2001; 107:695–702.
Parronchi P, Romagnani P, Annunziato F, et al. Type 1 T-helper cell predominance and interleukin-12 expression in the gut of patients with Crohn's disease. Am J Pathol 1997; 150:823–32.
Mariani P, Bachetoni A, D'Alessandro M, et al. Effector Th-1 cells with cytotoxic function in the intestinal lamina propria of patients with Crohn's disease. Dig Dis Sci 2000; 45:2029–35.
Coombes JL, Robinson NJ, Maloy KJ, Uhlig H H, Powrie F . Regulatory T cells and intestinal homeostasis. Immunol Rev 2005; 204:184–94.
Suzuki A, Hanada T, Mitsuyama K, et al. CIS3/SOCS3/SSI3 plays a negative regulatory role in STAT3 activation and intestinal inflammation. J Exp Med 2001; 193:471–81.
Zhong Z, Wen Z, Darnell JE Jr. Stat3: a STAT family member activated by tyrosine phosphorylation in response to epidermal growth factor and interleukin-6. Science 1994; 264:95–8.
Akira S, Nishio Y, Inoue M, et al. Molecular cloning of APRF, a novel IFN-stimulated gene factor 3 p91-related transcription factor involved in the gp130-mediated signaling pathway. Cell 1994; 77:63–71.
Akira S . IL-6-regulated transcription factors. Int J Biochem Cell Biol 1997; 29:1401–18.
Takeda K, Noguchi K, Shi W et al. Targeted disruption of the mouse Stat3 gene leads to early embryonic lethality. Proc Natl Acad Sci U S A 1997; 94:3801–4.
Takeda K, Kaisho T, Yoshida N, et al. Stat3 activation is responsible for IL-6-dependent T cell proliferation through preventing apoptosis: generation and characterization of T cell-specific Stat3-deficient mice. J Immunol 1998; 161:4652–60.
Sano S, Itami S, Takeda K, et al. Keratinocyte-specific ablation of Stat3 exhibits impaired skin remodeling, but does not affect skin morphogenesis. EMBO J 1999; 18:4657–68.
Takeda K, Clausen BE, Kaisho T, et al. Enhanced Th1 activity and development of chronic enterocolitis in mice devoid of Stat3 in macrophages and neutrophils. Immunity 1999; 10:39–49.
Riley JK, Takeda K, Akira S, Schreiber RD . Interleukin-10 receptor signaling through the JAK-STAT pathway. Requirement for two distinct receptor-derived signals for anti-inflammatory action. J Biol Chem 1999; 274:16513–21.
Welte T, Zhang SS, Wang T, et al. STAT3 deletion during hematopoiesis causes Crohn's disease-like pathogenesis and lethality: a critical role of STAT3 in innate immunity Proc Natl Acad Sci U S A 2003; 100:1879–84.
Elson CO, Cong Y, McCracken VJ, Dimmitt RA, Lorenz RG, Weaver CT . Experimental models of inflammatory bowel disease reveal innate, adaptive, and regulatory mechanisms of host dialogue with the microbiota. Immunol Rev 2005; 206:260–76.
Kuhn R, Lohler J, Rennick D, Rajewsky K, Muller W . Interleukin-10-deficient mice develop chronic enterocolitis. Cell 1993; 75:263–74.
Moore KW, de Waal Malefyt R, Coffman RL, O'Garra A . Interleukin-10 and the interleukin-10 receptor Annu Rev Immunol 2001; 19:683–765.
Groux H, O'Garra A, Bigler M, et al. A CD4+ T-cell subset inhibits antigen-specific T-cell responses and prevents colitis. Nature 1997; 389:737–42.
Sakaguchi S . Naturally arising Foxp3-expressing CD25+CD4+ regulatory T cells in immunological tolerance to self and non-self. Nat Immunol 2005; 6:345–52.
Mottet C, Uhlig HH, Powrie F . Cutting edge: cure of colitis by CD4+CD25+ regulatory T cells. J Immunol 2003; 170:3939–43.
Banchereau J, Steinman RM . Dendritic cells and the control of immunity. Nature 1998; 392:245–52.
Steinman RM, Hawiger D, Nussenzweig MC . Tolerogenic dendritic cells. Annu Rev Immunol 2003; 21:685–711.
Stagg AJ, Hart AL, Knight SC, Kamm MA . The dendritic cell: its role in intestinal inflammation and relationship with gut bacteria. Gut 2003; 52:1522–9.
Liu YJ, Kanzler H, Soumelis V, Gilliet M . Dendritic cell lineage, plasticity and cross-regulation. Nat Immunol 2001; 2:585–9.
Inaba K, Inaba M, Romani N, et al. Generation of large numbers of dendritic cells from mouse bone marrow cultures supplemented with granulocyte/macrophage colony-stimulating factor. J Exp Med 1992; 176:1693–702.
Brawand P, Fitzpatrick DR, Greenfield BW, et al. Murine plasmacytoid pre-dendritic cells generated from Flt3 ligand-supplemented bone marrow cultures are immature APCs. J Immunol 2002; 169:6711–9.
Gilliet M, Boonstra A, Paturel C, et al. The development of murine plasmacytoid dendritic cell precursors is differentially regulated by FLT3-ligand and granulocyte/macrophage colony-stimulating factor J Exp Med 2002; 195:953–8.
Siegal F P, Kadowaki N, Shodell M, et al. The nature of the principal type 1 interferon-producing cells in human blood. Science 1999; 284:1835–7.
Nakano H, Yanagita M, Gunn MD . CD11c(+)B220(+)Gr-1(+) cells in mouse lymph nodes and spleen display characteristics of plasmacytoid dendritic cells. J Exp Med 2001; 194:1171–8.
Asselin-Paturel C, Trinchieri G . Production of type I interferons: plasmacytoid dendritic cells and beyond. J Exp Med 2005; 202:461–5.
Rissoan M C, Soumelis V, Kadowaki N, et al. Reciprocal control of T helper cell and dendritic cell differentiation. Science 1999; 283:1183–6.
Pulendran B, Smith J L, Caspary G, et al. Distinct dendritic cell subsets differentially regulate the class of immune response in vivo Proc Natl Acad Sci U S A 1999; 96:1036–41.
Laouar Y, Welte T, Fu XY, Flavell RA . STAT3 is required for Flt3L-dependent dendritic cell differentiation. Immunity 2003; 19:903–12.
Kortylewski M, Kujawski M, Wang T, et al. Inhibiting Stat3 signaling in the hematopoietic system elicits multicomponent antitumor immunity. Nat Med 2005; 11:1314–21
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fu, X. STAT3 in immune responses and inflammatory bowel diseases. Cell Res 16, 214–219 (2006). https://doi.org/10.1038/sj.cr.7310029
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cr.7310029
Keywords
This article is cited by
-
An integrated analysis of mRNAs, lncRNAs, and miRNAs based on weighted gene co-expression network analysis involved in bovine endometritis
Scientific Reports (2021)
-
RETRACTED ARTICLE: Expansion of monocytic myeloid-derived suppressor cells ameliorated intestinal inflammatory response by radiation through SOCS3 expression
Cell Death & Disease (2021)
-
Gastrointestinal Disorders Associated with Primary Immunodeficiency Diseases
Clinical Reviews in Allergy & Immunology (2019)
-
Inhibition of Stat3 signaling pathway by nifuroxazide improves antitumor immunity and impairs colorectal carcinoma metastasis
Cell Death & Disease (2017)
-
The Shc1 adaptor simultaneously balances Stat1 and Stat3 activity to promote breast cancer immune suppression
Nature Communications (2017)