Abstract
Study design:
Single-blind randomized, controlled clinical study.
Objectives:
To evaluate, using kinematic gait analysis, the results obtained from gait training on a treadmill with body weight support versus those obtained with conventional gait training and physiotherapy.
Setting:
Thirty patients with sequelae from traumatic incomplete spinal cord injuries at least 12 months earlier; patients were able to walk and were classified according to motor function as ASIA (American Spinal Injury Association) impairment scale C or D.
Methods:
Patients were divided randomly into two groups of 15 patients by the drawing of opaque envelopes: group A (weight support) and group B (conventional). After an initial assessment, both groups underwent 30 sessions of gait training. Sessions occurred twice a week, lasted for 30 min each and continued for four months. All of the patients were evaluated by a single blinded examiner using movement analysis to measure angular and linear kinematic gait parameters. Six patients (three from group A and three from group B) were excluded because they attended fewer than 85% of the training sessions.
Results:
There were no statistically significant differences in intra-group comparisons among the spatial–temporal variables in group B. In group A, the following significant differences in the studied spatial–temporal variables were observed: increases in velocity, distance, cadence, step length, swing phase and gait cycle duration, in addition to a reduction in stance phase. There were also no significant differences in intra–group comparisons among the angular variables in group B. However, group A achieved significant improvements in maximum hip extension and plantar flexion during stance.
Conclusion:
Gait training with body weight support was more effective than conventional physiotherapy for improving the spatial–temporal and kinematic gait parameters among patients with incomplete spinal cord injuries.
Similar content being viewed by others
Introduction
One of the priorities in rehabilitation programs for spinal cord injuries (SCIs) is the restoration of functional locomotion, either while a patient is in a wheelchair or while he/she is standing on his/her feet.1 Estimates of the incidence of SCI vary widely. An annual incidence of between 15 and 30 SCIs per million inhabitants was reported for most countries,2 and the highest incidence occurred between 20 and 40 years of age. Owing to the improvement of health services, the incidence of incomplete paraplegia has increased.3
The level of the injury (paraparesis or tetraparesis), the time since the injury (acute or chronic injury) and the motor–sensory impairment are the main determinants of the final outcome.2 Among the technologies used for locomotion while standing on their feet, functional electrical stimulation seemed promising,4 but has not become commonplace. Gait training with body weight support has provided a new, prospective therapy for patients with incomplete SCIs, beginning with the work of Barbeau and Rossignol,5 studying the recovery of locomotion among cats with chronic SCIs, and continuing with the work of Wernig and Phys6 and Dietz et al.,7 comparing the electromyographic patterns of healthy individuals and SCI patients during and after training with weight support. Body weight reduction replaces uncontrolled spinal cord reflex patterns and compensates for motor losses. Gait training on a treadmill reinforces the principles of motor learning, thereby favoring specific tasks based on repetitive movements.8
Studies have indicated that gait training with weight support can potentially promote the improvement of gait in patients with an incomplete SCI.7, 9, 10, 11, 12, 13 However, there is no proof that the strategies used for gait training, with and without weight support, improve locomotion for patients with a SCI while standing on their feet.14
The aim of the present study is to compare the impact of gait training on a treadmill with body weight support and conventional physiotherapy (TBWS) with training with conventional physical therapy only.
Materials and methods
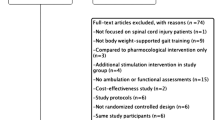
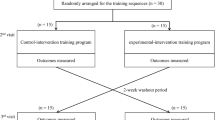
Thirty adult patients with incomplete SCIs (ASIA C and D) of traumatic origin that had occurred <12 months before enrollment were included in this study. The study included two arms: first arm (Group A), gait training on a treadmill with body weight support combined with conventional physiotherapy; and second arm (Group B), conventional physiotherapy alone. Participants were divided into two groups of 15 patients each and were randomized by drawing opaque envelopes containing the names of the two groups.
The sample size estimation calculations were based on a pilot study with the first 10 patients, based on gait velocity parameters assuming a two-tailed test, an alpha level equal to 0.05 and 80% power. This method generated a sample size of 10 patients per group.
Allowing for a conservative dropout rate and the inclusion of two groups, we recruited 30 patients to participate in the study to provide adequate protection against type II error.
The study patients were between 23 and 40 years of age who were able to walk (reciprocal gait pattern), had mild spasticity (score ⩽2 on the modified Ashworth scale) and had medical authorization to participate in supervised physical activities. Patients were not included if they were not able to walk (reciprocal gait pattern), were using a cardiac pacemaker or if they had unstable angina, any other decompensated heart disease, chronic obstructive pulmonary disease, uncontrolled autonomic dysreflexia, fractures of the lower limb bones, tracheostomy, deformity and rigidity of the hip and knee joints (20° of flexion or more) or of the ankle joints (10° of plantar flexion or more) or pressure ulcers. Patients who did not attend more than 85% of the training sessions were also excluded.
All volunteers were informed of the procedures for the study, and they signed informed consent forms written in accordance with the National Health Council Resolution CNS-196/96. This study was approved by the HC-FMUSP Research Ethics Committee. After selection of the participants, a single examiner was responsible for the administration of all evaluations (physical exam and gait analysis) performed before and after the intervention. This examiner was blind to the group assignments of the patients and did not participate in the intervention. The assignment of patients in the two groups was performed randomly using opaque and sealed envelopes containing the names of the groups: Group A or Group B. The envelopes were selected by an individual were not involved in this study. Group assignment was performed following the initial evaluation and just minutes before the initial treatment session. Two therapists trained on the exercise protocol for the study provided all treatment.
Both therapists were responsible for the two intervention protocols.
Interventions
Group A
Training with body weight support was performed on a Woodway Locosystem treadmill (Woodway USA, Inc., Foster, CT, USA), which enabled coupling to the Orbitador weight support system (Expansão Ltda., São Paulo, Brazil). The training consisted of the following: (1) passive stretching for 30 s for all muscle groups of the lower limbs, taking around 8 min in total, (2) passive mobilization of the hip, knee and ankle joints for 5 min, (3) positioning the patient on the treadmill using the weight support formed by a parachute harness that stabilizes the pelvic region and trunk, (4) use of a pulley system to keep the patient suspended, thereby eliminating some of the body weight that would be placed on the lower limbs and (5) individual assessment of each patient during the first session to define the percentage of off-loaded body weight and the duration and velocity of the treadmill training. The training began with 40% off-loading of body weight. The off-loading was reduced by 10% every 10 sessions while maintaining each participant's individually self-selected velocity in each session. Each patient underwent 30 semi-weekly sessions lasting 30 min each. In all of the sessions, participants were assisted by two physiotherapists who aided the movements of the lower limbs to simulate a normal gait.
Group B
Training with conventional physiotherapy consisted of the following: (1) passive stretching for 30 s for all muscle groups of the lower limbs, taking around 8 min in total, (2) passive mobilization of the hip, knee and ankle joints for 5 min and (3) overground gait training conducted and supervised by a physiotherapist (verbal commands and manual contact for correction of movements). When necessary, the parallel bars were used to ensure the safety of the patient. All of the patient's weight was placed on the floor, and the upper limbs were used as supports on the parallel bars when necessary.
Each patient underwent 30 semi-weekly sessions lasting 30 min each.
Gait assessment
Gait was evaluated by a blinded examiner with 10 years of experience in kinematic gait analysis. All participants in Groups A and B were evaluated before and after the 30 sessions of gait training.
To gather data for the kinematic analysis, a videogrammetry system was used. The evaluation was performed in three stages: (1) acquisition of video images for kinematic analysis of the lower limb movements during gait, (2) data processing to determine the segments of the lower limbs and extract graphs of the studied variables and (3) data treatment to eliminate noise arising from data acquisition and processing.
All patients were shown the equipment and advised about the described procedures, and they were instructed on how to carry out the sequence of tasks and activities. All of the patients underwent one day of pretraining without data acquisition to simulate a normal gait assessment. During this session, the patients wore swimsuits to facilitate the placement of the markers at anatomical points.
Reflective markers were attached at 15 anatomical points that were taken as reference points for the movement analysis system (Figure 1). All patients walked barefoot at a comfortable speed, which was similar to their everyday gait, using the parallel bars when necessary. They walked on a track marked on the floor that was 90 cm in width by 4 m in length. They walked along this track three times to produce gait cycles.
Two digital video cameras meeting the National Television System Committee standards and having a capture frequency of 30 Hz were used. The MaxTRAQ3D software (Innovision Systems, Columbiaville, MI, USA) was used, and calibration was performed to determine the location and orientation of each camera. A reference structure of four markers was constructed to adjust the overall coordinate system along with a calibration bar with two markers (dynamic calibration and size of the coordinate system). All parameters (brightness; spatial and temporal resolution; focus) were calibrated, adjusted and then kept unchanged throughout the image-acquisition procedure, thereby ensuring identical camera parameters for all patients. The cameras were first positioned anteriorly/posteriorly and then laterally in relation to the patient to make it possible to view each point of interest on the lower limbs using the two cameras (Figure 2).
For each walk along the track, a single gait cycle was selected and used for linear and angular kinematic data analysis of the joints in the sagittal plane. Two groups of variables were defined for analysis:
-
Spatial–temporal variables: gait velocity (m s−1), time of gait cycle (s), time of stance (% of gait cycle), time of swing (% of gait cycle), step length (cm), distance covered (m) and cadence (steps/minute).
-
Angular variables: maximum dorsiflexion during stance (degrees), maximum plantar flexion during preswing (degrees), minimum knee extension during stance (degrees), maximum knee flexion during swing (degrees), maximum hip flexion during gait cycle (degrees) and maximum hip extension during preswing (degrees).
Descriptive statistics for the demographic data and all of the outcome measures were expressed as means (95% intraclass) and medians. Comparison between the groups was performed using a paired t-test of the two groups for age, body mass and time of injury to determine the homogeneity of the two groups at baseline. The possible differences between the groups, according to the predefined spatial–temporal parameters, were analyzed using the Wilcoxon nonparametric test for comparisons between pairs of groups. The data for the angular variables were analyzed using a two-way analysis of variance.
The factors were side (left and right) and treatment (preintervention and postintervention).
Results
There were no statistically significant differences (P>0.05) among the groups for any of the outcome variables at baseline (preintervention) (Table 1).
There were not statistically significant group-by-time interaction comparisons observed among the spatial–temporal variables for Group B (conventional gait training). However, for Group A (treated with body weight support), there were significant differences, namely, increases observed after the training, for the spatial–temporal variables of velocity, distance covered, cadence, step length, time of gait cycle and time of swing phase. There was also a decrease in the time of stance (Tables 2 and 3).
There were statistically significant differences for angular kinematic gait parameters. Planned pairwise comparisons showed that only patients in Group A demonstrated an increased range of motion at the 12-week evaluation when compared with baseline values. The analysis of differences among groups following the intervention at the 12-week evaluation showed that the group undergoing body weight support training had a statistically greater range of motion during the preswing phase to the hip extension and ankle plantar flexion in comparison with those undergoing training on the basis of physiotherapy only. Table 4 summarizes within- and between-group differences with the associated 95% confidence intervals.
Discussion
Physiotherapy management for SCI patients that aims to recover walking function includes intense repetitive practice of walking movements with or without the use of a treadmill. To improve the use of muscles that work against gravity, the off-loading of some of the patient's body weight together with treadmill use may be an option. In this situation, leg movements are aided by the therapists during the sessions.
There is no evidence that specific locomotor training is more effective than any other type of therapy for improving the walking capacity of individuals with SCIs. In the present study, two treatment strategies for improving the locomotion of a group of 24 patients (48 limbs) with incomplete SCIs were compared. The patients enrolled in this study were selected using restricted criteria to control the heterogeneity of the injuries and their sequelae. The patients were selected in accordance with predetermined demographic, anthropometric and clinical characteristics so that the training protocol could be applied without risks and biased results could be avoided.
Group A received physiotherapy combined with gait training on a treadmill with weight support, whereas Group B received conventional physiotherapy, namely, the type of gait training that is usually conducted in most rehabilitation centers. The restricted objective in both groups was to improve the patients’ walking capacity. The regimen of gait training with weight support is based on the neuromuscular principles of human and animal locomotion from previously published studies.11, 15, 16, 17
This study did not find any statistically significant differences in intragroup (before and after) comparisons for the spatial–temporal parameters in Group B (conventional gait training). However, there were significant differences, namely, increases observed after the training, for Group A (treated with body weight support) in the spatial–temporal parameters of velocity, distance covered, cadence, step length, time of gait cycle and time of swing phase. There was also a reduction in the stance time. Gait training with weight support increased gait stability by producing an increase in step length, decreasing the time stance phase and increasing the swing. This training also improved patient performance via increased velocity, cadence, distance covered and time of the gait cycle. These results are similar to those reported by other authors who showed that there were improvements in independence and walking capacity, in addition to increases in gait velocity.9, 10, 11, 12
The angular variations in the hip, knee and ankle joints in the sagittal plane were also evaluated. There were no significant differences in intragroup comparisons (before and after) among the Group B patients independent of the assessed side. Conversely, the Group A patients showed increases in maximum hip extension during stance and maximum plantar flexion during preswing. The other evaluated variables, including maximum dorsiflexion during stance, minimum knee extension during stance, maximum knee flexion during balance and maximum hip flexion during gait cycle, did not change after the training. The increases in hip extension and plantar flexion directly influenced the step length, thereby explaining the greater step length and improved cadence that were observed.18, 19
Increased hip extension increases the step length, but other factors may also interfere: greater extension and consequent reduction of knee flexion at initial contact, improvement of hip flexion, increased pelvic rotation, improvement of muscle strength and reduction of spasticity.18, 19, 20, 21 Even though all the angular variables may interfere with step length, there is no doubt that the training with weight support increased the amplitude of hip extension and increased the step length.
Plantar flexion at the end of the stance, that is, preparing the foot for the swing phase, and hip flexion are important for determining the degree of knee flexion during the swing.18, 19, 21, 22
The increase in plantar flexion among the patients in Group B, caused by increased muscle strength (improvement in concentric contraction) and better alignment of the feet in the transverse plane, did not give rise to greater knee and hip flexion during the swing phase and had no repercussions for the angular movements during this phase of the gait cycle. Training with weight support provided gains in hip extension and ankle plantar flexion, as well as improvement in spatial–temporal gait parameters. The association between this improvement and stimulation of neural plasticity and pattern-generating centers is questionable because the gain in hip extension and plantar flexion during the end stance and prebalance did not facilitate hip flexion, ankle dorsiflexion or consequent knee flexion during the swing through reflex action. We speculate that this deficiency may be due to the short duration of stimulation (daily, weekly and total) or the use of insufficient velocity or an inefficient weight-support system, especially if the stimulation produced was sufficient to promote changes in neural plasticity. However, although the observed improvement was not as expected, it may be inferred that the training stimulated an increase in spinal cord activity. Performing evaluations between certain sessions, particularly the points at which the weight support was decreased (such as at the 10th and 20th sessions in the present study), and reassessing patients at a time point after the end of the protocol (3, 6 and 12 months later) could be useful for verifying whether the acquired improvement is maintained or lost after the training ends. This type of follow-up evaluation may be the key for showing whether good results persisted following treatment. It is well known that many training effects disappear following cessation of treatment and do not affect the final outcome. Without follow-up testing, the long-term benefits of treatment in Group A are unknown.
Gait analysis is considered to be a high-cost tool for hospitals and rehabilitation centers. The equipment is relatively expensive, and there are few professionals trained to use them and interpret the data. Motion analysis laboratories are primarily used to evaluate the potential need for surgery indication and for research. Rarely are these laboratories used to guide decisions or improve support for clinical non-surgical treatments, such as physiotherapy and motor rehabilitation. The use of low-cost systems, as was used in this study, is an option; however, the data processing is slow, and detailed calibration and data capture requires significant attention and careful observation so their limitations are not exceeded. Gait analysis provides a quantitative assessment of neuronal and biomechanical mechanisms. It may be helpful in determining the physiotherapeutic and pharmacological management that is most effective for patients with SCIs, thereby reducing the costs and increasing the efficiency of the provided treatments.
Conclusion
Among patients with incomplete SCIs, gait training was more effective with body weight support than with conventional physiotherapy alone for improving spatio–temporal and kinematic gait parameters. In particular, this study opens new perspectives for future randomized clinical trials in the field of intensive rehabilitation and for the use of motion analysis tools to measure human movement.
References
Hesse S, Werner C . Connecting research to the needs of patients and clinicians. Brain Res Bull 2009; 78: 26–34.
Wyndaele M, Wyndaele JJ . Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord 2006; 44: 523–529.
Ackery A, Tator C, Krassioukov A . A global perspective on spinal cord injury epidemiology. J Neurotrauma 2004; 21: 1355–1370.
Maynard Jr FM, Bracken MB, Creasey G, Ditunno Jr JF, Donovan WH, Ducker TB et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
Marsolais EB, Kobetic R . Implantation techniques and experience with percutaneous intramuscular electrodes in the lower extremities. J Rehabil Res Dev 1986; 23: 1–8.
Barbeau H, Rossignol S . Recovery of locomotion after chronic spinalization in the adult cat. Brain Res 1987; 412: 84–95.
Wernig A, Müller S . Laufband locomotion with body weight support improved walking in persons with severe spinal cord injuries. Paraplegia 1992; 30: 229–238.
Dietz V, Colombo G, Jensen L . Locomotor activity in spinal man. Lancet 1994; 344: 1260–1263.
Ditunno J, Scivoletto G . Clinical relevance of gait research applied to clinical trials in spinal cord injury. Brain Res Bull 2009; 78: 35–42.
Postans NJ, Hasler JP, Granat MH, Maxwell DJ . Functional electric stimulation to augment partial weight-bearing supported treadmill training for patients with acute incomplete spinal cord injury: a pilot study. Arch Phys Med Rehabil 2004; 85: 604–610.
Field-Fote EC, Tepavac D . Improved intralimb coordination in people with incomplete spinal cord injury following training with body weight support and electrical stimulation. Phys Ther 2002; 82: 707–715.
Dobkin B, Apple D, Barbeau H, Basso M, Behrman A, Deforge D et al. Spinal Cord Injury Locomotor Trial Group. Weight-supported treadmill vs over-ground training for walking after acute incomplete SCI. Neurology 2006; 66: 484–493.
Hornby TG, Zemon DH, Campbell D . Robotic-assisted, body-weight-supported treadmill training in individuals following motor incomplete spinal cord injury. Phys Ther 2005; 85: 52–66.
Lucareli PR, Lima MO, Lima FP, Garbelotti Jr SA, Gimenes RO, Almeida JG et al. Gait analysis and quality of life evaluation after gait training in patients with spinal cord injury. Rev Neurol 2008; 46: 406–410.
Mehrholz J, Kugler J, Pohl M . Locomotor training for walking after spinal cord injury. Spine (Phila Pa 1976) 2008; 33: E768–E777.
Grillner S . Neurobiological bases of rhythmic motor acts in vertebrates. Science 1985; 228: 143–149.
Pearson KG, Rossignol S . Fictive motor patterns in chronic spinal cats. J Neurophysiol 1991; 66: 1874–1887.
Harkema SJ, Hurley SL, Patel UK, Requejo PS, Dobkin BH, Edgerton VR . Human lumbosacral spinal cord interprets loading during stepping. J Neurophysiol 1997; 77: 797–811.
Gage JR, Koop SE, Schwartz MH, Novacheck TF . The Identification and Treatment of Gait Problems in Cerebral Palsy, Series: Clinics in Developmental Medicine, no. 180–181. Mac Keith Press: London, 2009, p 644.
Perry J, Burnfield JM . Gait Analysis: Normal and Pathological Function. SLACK Incorporated: Thorofare, NJ, 2010, p 551.
Lucareli PR, D’Andrea Greve JM . Knee joint dysfunctions that influence gait in cerebrovascular injury. Clinics 2008; 63: 443–450.
Kirtley C . Clinical Gait Analysis—Theory and Practice (Hardcover). Churchill Livingstone: Oxford, 2006, p 328.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lucareli, P., Lima, M., Lima, F. et al. Gait analysis following treadmill training with body weight support versus conventional physical therapy: a prospective randomized controlled single blind study. Spinal Cord 49, 1001–1007 (2011). https://doi.org/10.1038/sc.2011.37
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.37
Keywords
This article is cited by
-
The efficacy of gait rehabilitations for the treatment of incomplete spinal cord injury: a systematic review and network meta-analysis
Journal of Orthopaedic Surgery and Research (2023)
-
Walking after Spinal Cord Injury: Current Clinical Approaches and Future Directions
Current Physical Medicine and Rehabilitation Reports (2020)
-
Functional magnetic resonance imaging (fMRI) of the sensorimotor cortex in spinal cord injury patient after intensive rehabilitation
Research on Biomedical Engineering (2020)
-
Acute Intermittent Hypoxia as a Potential Adjuvant to Improve Walking Following Spinal Cord Injury: Evidence, Challenges, and Future Directions
Current Physical Medicine and Rehabilitation Reports (2020)
-
Influence of percentage of body-weight support on gait in patients with traumatic incomplete spinal cord injury
The Egyptian Journal of Neurology, Psychiatry and Neurosurgery (2019)