Abstract
Objective:
To describe neonatal intensive care unit (NICU) medical interventions and NICU mortality by birth weight and major anomaly types for infants with trisomy 13 (T13) or 18 (T18).
Study Design:
Retrospective cohort analysis of infants with T13 or T18 from 2005 to 2012 in the Pediatrix Medical Group. We classified infants into three groups by associated anomaly type: neonatal surgical, non-neonatal surgical and minor. Outcomes were NICU medical interventions and mortality.
Results:
841 infants were included from 186 NICUs. NICU mortality varied widely by anomaly type and birth weight, from 70% of infants <1500 g with neonatal surgical anomalies to 31% of infants ⩾2500 g with minor anomalies. Infants ⩾1500 g without a neonatal surgical anomaly comprised 66% of infants admitted to the NICU; they had the lowest rates of NICU medical interventions and NICU mortality.
Conclusions:
Risk stratification by anomaly type and birth weight may help provide more accurate family counseling for infants with T13 and T18.
Similar content being viewed by others
Introduction
There is ongoing debate about the extent of neonatal intensive care unit (NICU) interventions that should be provided for infants with trisomy 13 (T13) or trisomy 18 (T18), and whether providing more interventions impacts survival.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21 Multi-center studies are limited to very-low-birth-weight (VLBW) infants1 or to older survivors for whom information on neonatal management is lacking.22 Parent surveys report many infants who survive past 1 year, but there is no denominator of how many infants received neonatal intervention or what kinds of intervention they received.4, 14, 23 Single-center case series report 1-year survival among infants receiving intensive treatment and cardiac surgeries, but these are limited by small numbers.3, 6, 24 Due to lack of multi-center data on neonatal management of infants with T13 or T18, it is challenging for families and physicians to have informed discussions on medical interventions for infants with these diagnoses.3, 5, 6, 23, 24, 25, 26, 27
The impact of NICU medical interventions on survival may be influenced by coexisting major anomalies or birth weight.3, 28, 29, 30 Although rates of anomalies for infants with T13 or T18 are well-documented, not all anomalies impact survival equally.11, 12, 29, 31 For example, infants with limb anomalies may not require immediate inpatient care, whereas infants with ductal-dependent cardiac lesions require immediate decisions about surgical intervention. In addition, many infants with T13 or T18 are born with significant growth restriction; birth-weight influences feasibility of some surgical interventions.32 For families pursuing a goal of discharge home from the NICU, it would be helpful to understand how many infants survived to discharge home after birth, and how coexisting anomalies, birth weight and receipt of medical interventions affect their infant’s chance of discharge home.
Our specific objectives were to use a multi-center NICU data set to (1) evaluate the rates of coexisting major anomalies in infants with T13 or T18, categorized by whether or not those anomalies are life-threatening without surgical intervention during the neonatal period; (2) describe the use of NICU medical interventions by anomaly type and birth weight; (3) compare NICU mortality by anomaly type, birth weight and receipt of medical interventions.
Materials and methods
We conducted a retrospective cohort analysis of infants with T13 or T18 admitted to the NICU from 2005 to 2012 using the Pediatrix Clinical Data Warehouse (CDW). The CDW contains de-identified electronic medical record data on all infants from 270 NICUs in 34 states, including academic and private NICUs of all levels of care, and representing 15–20% of NICU admissions in the U.S. Data are automatically extracted from the medical record generated prospectively by clinicians, de-identified and stored in the CDW. Information includes maternal history, birth information, demographics, medications, laboratory values, diagnoses and respiratory support. The CDW includes all diagnoses that are made throughout a patient’s hospitalization, not just admission diagnoses. All diagnoses are recorded as entered by the provider; major and minor anomaly diagnoses are flagged within the CDW. T13 and T18 are coded discretely.
We manually reviewed all diagnoses flagged as major or minor anomalies in the CDW, and consolidated them similarly to reports from the Vermont Oxford Network32 and National Institutes of Child Health and Development Neonatal Research Network.33 We further classified major anomalies into those that are neonatal surgical or non-neonatal surgical. A neonatal surgical anomaly was defined as follows: (a) incompatible with life without surgical intervention during the neonatal period, and/ or (b) an anomaly that prohibits enteral feeding unless surgically repaired during the neonatal period. Accordingly, the following anomalies were counted as ‘neonatal surgical’: gastrointestinal anomalies such as bowel atresias and gastroschisis; diaphragmatic hernia; meningomyelocele, and ductal-dependent cardiac lesions (hypoplastic left heart syndrome, interrupted aortic arch, total anomalous pulmonary venous return, transposition of the great vessels, pulmonary atresia, tricuspid atresia and truncus arteriosus)(Supplementary Information (1)). As the CDW does not systematically require details about surgical intervention, we were not able to determine with certainty whether patients with neonatal surgical anomalies received neonatal surgical intervention, only that such an anomaly was present.
We defined a ‘non-neonatal surgical’ anomaly as a major life-limiting anomaly that does not necessarily require surgery during the neonatal period. For example, an AV canal typically does not cause symptoms until several weeks of life. Thus, it does not prohibit discharge home if feedings and respiratory status are stable. Similarly, neurologic anomalies such as holoprosencephaly impact survival, but cannot be surgically repaired, and therefore were also classified as ‘non-neonatal surgical.’ Infants with multiple anomalies (such as hypoplastic left heart syndrome and coarctation of the aorta) were classified under the more severe category (in this case hypoplastic left heart syndrome).
Infants without major anomalies were classified as having ‘minor’ anomalies, since they were likely to have characteristic facial, musculoskeletal or skin anomalies but would not necessarily require neonatal intensive care for those specific conditions.
We defined ‘NICU medical interventions’ as interventions generally only offered in an intensive care setting. We recorded respiratory supports including mechanical ventilation, surfactant and inhaled nitric oxide; cardiovascular medications including prostaglandins, vasopressors and systemic corticosteroids; and neuromuscular blocking agents.
Information on anomalies and medical interventions was merged with patient data including gender, gestational age by obstetric estimate, birth weight, multiple gestations, maternal age, maternal race/ethnicity, delivery method, Apgar scores and inborn status.
Data analysis
All infants with a diagnosis of T13 or T18 admitted to a Pediatrix NICU between 2005 and 2012 were included. Rates of missing demographic data were assessed (infants with missing data were retained in the data set). For calculation of mortality rates, infants who were transferred were retained in the denominator. Our primary outcome of interest was mortality before NICU discharge.
First, we evaluated demographic characteristics of infants with T13 or T18 to compare our data to prior reports in the literature. Second, we identified major anomalies in infants with T13 or T18, and calculated the proportion of infants with T13 or T18 who had neonatal surgical anomalies, non-neonatal surgical anomalies or minor anomalies. Third, we compared differences in the use of NICU medical interventions among infants with T13 or T18 by coexisting anomalies and birth weight. We analyzed use of prostaglandin only for infants with neonatal surgical cardiac anomalies. Univariate comparisons were made using χ2 and Wilcoxon rank-sum tests, as appropriate. Finally, we calculated differences in NICU mortality by birth weight, major anomalies and receipt of medical intervention.
The Mantel–Haenszel test was used to evaluate temporal trends in admissions, inborn status, receipt of mechanical ventilation, and mortality over the study period. A P-value of 0.05 was accepted for statistical significance. Stata version 13 was used for all analyses. The study was approved by the Medical College of Wisconsin institutional review board; the Clinical Data Warehouse was approved for research use by the Western institutional review board.
Results
Demographic characteristics
Out of 615 200 neonates admitted to the Pediatrix NICUs from 2005–2012, 273 had T13 and 568 had T18, representing 0.13% of all admissions and 11% of all infants with a recognized chromosomal anomaly. These infants were admitted to one of 186 NICUs. There was no significant clustering of infants with T13 or T18 within NICUs; 132 (71%) of the NICUs had ⩽5 patients with T13 or T18, 33 (18%) of NICUs had 6–10 patients, and 21 (11%) had >10 patients. All but two infants with T13 or T18 were cared for in a center that provided mechanical ventilation, and 94% were cared for in a center that discharged at least one patient with a neonatal surgical condition.
Demographic characteristics are shown in Supplementary Information (2) (online). Three-fourths of infants were born after 34 weeks’ gestation. VLBW was uncommon, but low birth-weight occurred in over half of the infants. Three-fourths of infants were inborn and born to mothers under 35 years of age. Half of infants were delivered via cesarean section. Less than 10% of infants had a 5-minute Apgar score<3. There were no significant temporal trends from 2005–2012 in number of NICU admissions, although more infants were inborn over time (67% inborn in 2005–2006 increasing to 80% inborn in 2011–2012; Mantel–Haenzel test for trend P=0.003).
Major anomalies
Figure 1 shows the common anomalies in infants with T13 or T18. The majority of infants had a coexisting major anomaly; however, most were non-neonatal surgical anomalies. Although there were differences between T13 and T18 in prevalence of specific anomalies, overall the most common neonatal surgical anomaly was tracheoesophageal fistula. Cardiac neonatal surgical anomalies were recognized in only 5% of patients.
Common major anomalies in Trisomy 13 and 18. The flow chart depicts anomaly categories for infants with Trisomy 13 and 18. The top row indicates the number of NICU admissions with Trisomy 13 or 18 separately. The second row shows the number of infants in each designated anomaly category. Anomalies are categorized as neonatal surgical, non-neonatal surgical and minor. Neonatal surgical=an infant with a major anomaly that requires surgery during the neonatal hospitalization for survival; non-neonatal surgical=an infant with a major anomaly that does not necessarily require surgery during the neonatal hospitalization for survival; minor=infants without major anomalies. Since some patients had multiple anomalies, the numbers in the white boxes indicate the number of infants whose most severe anomaly falls into that category; for example, an infant with a ductal-dependent cardiac lesion plus a VSD would be counted as neonatal surgical. The third row lists specific anomalies which fall into that category, and the number of infants with each specific anomaly, listed in order of frequency for that trisomy. Because some infants had multiple anomalies, the numbers in the third row do not add up to the number of infants in each anomaly category. Cardiac neonatal surgical conditions include hypoplastic left heart syndrome, interrupted aortic arch, pulmonary atresia, total anomalous pulmonary venous return, transposition of great vessels, tricuspid atresia, truncus arteriosus. ASD, atrial septal defect; CDH, congenital diaphragmatic hernia; NICU, neonatal intensive care unit; PDA, patent ductus arteriosus; TEF, tracheoesophageal fistula; VSD, ventricular septal defect.
NICU medical interventions
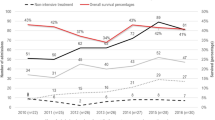
Figure 2 shows NICU medical interventions in infants with T13 or T18, stratified by major anomaly and birth-weight. Infants with T13 or T18 were likely to receive mechanical ventilation, with those receiving ventilation having a median 5 days on the ventilator (IQR 2–10 days). Vasopressors and inhaled nitric oxide were infrequently used. Of the 42 infants with cardiac neonatal surgical anomalies, 19 (45%) received prostaglandin.
NICU medical interventions in infants with Trisomy 13 or 18 by birth-weight and anomaly type. Three graphs, A–C, illustrate the proportion of infants receiving NICU medical interventions. Graph A depicts infants with birth-weight <1500 g; B depicts infants with birth-weight 1500–2499 g; C depicts infants with birth-weight ⩾2500 g. The x-axis is the same in each graph, and represents NICU medical interventions. Ventilation=mechanical ventilation. Steroids=systemic corticosteroids. Pressors=dopamine, dobutamine, epinephrine, norepinephrine or milrinone. Paralytic=vecuronium, cisatracurium or rocuronium. NICU, neonatal intensive care unit; iNO, inhaled nitric oxide; PGE, prostaglandin E (reported only for infants with ductal-dependent cardiac lesions). The y-axis is the same in each graph, and represents percentage of infants in that group who received the intervention. Shaded columns each represent percentage of infants who received an intervention in each of the anomaly groups. Neonatal surgical=an infant with a major anomaly that requires surgery during the neonatal hospitalization for survival; non-neonatal surgical=an infant with a major anomaly that does not necessarily require surgery during the neonatal hospitalization for survival; minor=infants without major anomalies. P-values indicate differences in use of NICU intervention among anomaly groups, by χ2 or Fisher’s exact test, as appropriate.
Overall, receipt of NICU medical intervention was most common in infants with neonatal surgical anomalies, occurring in 96/142 (67%) infants with neonatal surgical anomalies, 274/545 (50%) infants with non-neonatal surgical anomalies, and 33/154 (21%) infants with only minor anomalies. VLBW infants were more likely to receive mechanical ventilation, vasopressors and surfactant. Infants with minor anomalies were least likely to receive medical interventions across all birth-weight categories.
There were no temporal trends in receipt of mechanical ventilation from 2005–2012 (Mantel–Haenzel test for trend P=0.759). There were no differences in receipt of medical intervention between infants with T13 and infants with T18, except that infants with T13 were more likely to receive postnatal steroids (8 vs 3%, P<0.001).
NICU Mortality
In total, 47% of infants with T13 or T18 died in the NICU; 40% survived to home discharge; 13% were transferred to another facility before discharge. The proportion of infants transferred was similar to infants without T13 or T18 (13%; P=0.593), and was not different among the anomaly groups (11–13%, P=0.707). For surviving infants discharged home, the median length of stay (LOS) was 10 days (IQR 6–23 days). For infants who died, median LOS was 4 days (IQR 1–12). There were no temporal trends in survival to NICU discharge, transfer before discharge or LOS for infants who died in the NICU or survived to discharge from 2005–2012.
Figure 3 shows that infants’ birth-weight and anomaly category were associated with significant differences in mortality before NICU discharge among infants with T13 or T18. NICU mortality varied widely by birth-weight and anomaly category, ranging from 70% of infants <1500 g with neonatal surgical anomalies to 31% of infants ⩾2500 g with only minor anomalies. VLBW infants had the highest mortality in every anomaly category. Among larger birth-weight infants, neonatal surgical anomalies were associated with higher mortality. When analyzed separately, infants with T13 had higher NICU mortality than infants with T18 in the lower-risk groups of infants ⩾1500 gm (54 vs 36%, P<0.001) and infants without neonatal surgical anomalies (51 vs 36%, P=0.001). There were no differences in mortality between infants with T13 and T18 among those with neonatal surgical anomalies (69 vs 59%, P=0.317) or those <1500 gm (71 vs 68%, P=0.719).
Mortality before NICU discharge for infants with Trisomy 13 or Trisomy 18 by birth-weight and anomaly type. Figure 3 shows NICU mortality by birth-weight and anomaly type. The x-axis shows birth-weight categories; the y-axis shows the proportion of infants who died before NICU discharge. Infants who were transferred were retained in the denominator for calculations. Shaded bars represent anomaly categories. Neonatal surgical=an infant with a major anomaly that requires surgery during the neonatal hospitalization for survival; non-neonatal surgical=an infant with a major anomaly that does not necessarily require surgery during the neonatal hospitalization for survival; minor=infants without major anomalies. P-values indicate differences in mortality between groups, by χ2 or Fisher’s exact test, as appropriate.
Table 1 shows the association between receipt of NICU medical intervention and NICU mortality in subgroups of anomaly category and birth-weight. Overall, infants receiving NICU medical intervention had similar or higher NICU mortality compared with infants who did not receive NICU medical intervention. Of the 14 infants with neonatal surgical anomalies that were discharged home without NICU medical interventions, 9 infants had a cardiac anomaly, 2 infants had tracheoesophageal fistula/esophageal atresia and 1 infant each had imperforate anus, CDH and meningomyelocele.
Infants >1500 g without a neonatal surgical anomaly comprised 554/841 (66%) of the infants in the study. These infants were at lower risk for receipt of intervention and subsequent NICU mortality. Infants in these lower-risk groups who did not receive NICU medical intervention had approximately half the NICU mortality of their anomaly- and birth-weight-matched peers (21–43% vs 50–82%).
Discussion
This is the first multi-center study to describe the medical management of infants with T13 or T18 admitted to U.S. NICUs. Our findings add to the literature on outcomes of infants with T13 and T18 by describing not just overall survival, but by the major risk factors of anomaly type and birth-weight. A publication from the NICHD Neonatal Research Network highlighted the high mortality of VLBW infants with T13 or T18.1 Our study extends those findings by highlighting the survival of infants larger than 1500g, who represent >75% of NICU admissions with T13 or T18. Our major conclusions are:
-
1)
Although most infants with T13 or T18 had a major anomaly, few had a neonatal surgical anomaly that would require immediate decisions about surgical intervention.
-
2)
Infants with T13 or T18 received a wide range of NICU medical interventions.
-
3)
Infants who were born VLBW or with a neonatal surgical anomaly had twice the NICU mortality rate of infants without those risk factors.
-
4)
Infants who received NICU medical interventions did not have significantly improved survival to NICU discharge; in fact, the majority of infants discharged home received minimal NICU medical intervention.
There is often clinical and ethical conflict between health care providers or between families and providers, over how much intervention should be offered to infants with T13 or T18.4, 34 We found that the majority of infants with T13 or T18 admitted to a NICU in fact do not require decisions pertaining to surgical management during the neonatal period. We do not know how many of these infants were considered for medical and surgical interventions after the neonatal period. We also do not know how the distribution of coexisting anomalies differs from infants diagnosed prenatally, who may have experienced in utero demise or whose parents may have chosen pregnancy termination. The prevalence of coexisting anomalies in this study was consistent with other published reports.29, 30, 31, 35 Although most studies on surgical intervention for infants with T13 or T18 have focused on congenital heart disease,5, 24 we found that the most common condition associated with early neonatal surgery was tracheoesophageal fistula. Surgical decision-making for non-cardiac conditions is an important area for further research. Regardless, in counseling families on how to best advocate for their infant, encouraging a longitudinal relationship with a supportive primary care provider and relevant subspecialists is critical to addressing intervention decisions over time, not just at birth.
Despite concern that medical providers are unwilling to provide neonatal intensive care to infants with T13 or T18,4, 34 we found that infants with T13 or T18 were offered a wide variety of medical interventions. Infants frequently received ventilation and surfactant, and those with neonatal surgical anomalies were more likely to receive medical interventions. These findings could represent two possible clinical scenarios: Some families likely received a prenatal diagnosis and were interested in pursuing NICU interventions. Other families may have received a postnatal diagnosis and made decisions about the extent of NICU interventions after a diagnosis was confirmed. We do not have data on the number of infants diagnosed prenatally with T13 or T18, but in an era of increasingly common prenatal diagnostic testing, it is likely that a significant percentage of families knew or suspected the diagnosis and opted for intervention. A survey of US neonatologists showed that about half would resuscitate an infant with T18 if parents desired.36 Our results suggest that, consistent with the report about older infants with T13 or T18 receiving inpatient care and procedures, neonates with these conditions also receive significant NICU interventions.22 Our finding that NICU survival, LOS and use of mechanical ventilation have not significantly changed over our study period may reflect that a high proportion (40%) of infants in this cohort were receiving mechanical ventilation at the onset of the study period, and suggests that the changes in the medical treatment of these infants may have occurred prior to the study period we investigated. The increasing number of inborn admissions and large proportion of infants delivered via Cesarean section in our study also suggests that many obstetricians may be willing to arrange transfer of care and offer surgical intervention to facilitate a live birth.
We found wide variation in NICU mortality by infants’ anomaly type and birth-weight, with VLBW infants and those with neonatal surgical anomalies having twice the NICU mortality of other infants with T13 and T18. We suggest that physicians offering prognostic counseling could apply this type of risk stratification when offering prognostic counseling for infants with T13 and T18. A key feature of our study is that we reported mortality before NICU discharge, as opposed to the commonly-reported outcome of mortality before one year of age. Recent literature and our clinical experience both suggest that this distinction is not always clear when counseling families of infants with T13 or T18. Although medical textbooks and population studies report 75–90% 1-year mortality, it is important to understand that this does not necessarily mean that their infant with T13 or T18 will die during the birthing process or shortly after birth. Indeed, our results show that a majority of these infants do not have poor Apgar scores, and do not require significant resuscitation at birth. In our study we do not have the numbers of spontaneous or elective terminations of pregnancy or the numbers of infants who died in the delivery room, but we do know that at least 841 infants with T13 or T18 were admitted to a NICU, and 40% of those admitted to a NICU survived to discharge home. This is similar to a Japanese national study reporting 50% mortality within the first week of life.37 Death after NICU discharge is certainly a strong possibility in this high-risk patient group. But if a family’s goal is to meet their baby and decide over time how much intervention makes sense, we suggest that physicians should provide counseling about survival to discharge for babies admitted to a NICU, along with longer-term survival. Inappropriate counseling regarding the timing of mortality may lead to parents’ distrust of the medical system and complicate later decision-making.
We found that receipt of NICU medical interventions was not necessarily associated with improved survival to discharge. This again suggests two possible clinical scenarios: the first is that for some infants, interventions were started and then withdrawn, perhaps when a diagnosis was confirmed and discussions led to withdrawal. The other possibility is that for some infants, interventions were provided but the infants were too sick and the interventions were not effective. Infants with neonatal surgical anomalies who survived without medical interventions may represent infants who received surgical intervention without NICU medical support, such as coming back from the operating room extubated, or infants discharged with palliative care. In any scenario, these data support that many infants with T13 or T18 are offered NICU interventions, and it is likely that the high risk of NICU mortality is not entirely a self-fulfilling prophecy.
The majority of infants in our study did not have neonatal surgical anomalies, were not VLBW, and did not receive intervention. These infants had nearly half the rate of NICU mortality compared with their peers receiving NICU medical intervention. Again, this has two possible interpretations: The first is that many infants with T13 and T18 may not receive intervention in the neonatal period because they do not require intervention in the neonatal period. Many medical and surgical interventions are reported for infants with T13 or T18 after the neonatal hospitalization. 22 The second is that some families may choose limited interventions during the neonatal hospitalization, opting to go home with palliative care. From a practical standpoint, it is easier to arrange home discharge for babies receiving fewer NICU interventions. In both scenarios, it is important to counsel families that many infants with T13 and T18 will need a range of home care supports, which are likely to include medical and surgical considerations in addition to supportive palliative care services.
The results of this study should be interpreted in light of several limitations. Although the rate of anomalies is consistent with other publications, this is a retrospective study of data abstracted from electronic medical record documentation. We do not have information on whether the diagnosis of T13 or T18 was made prenatally or postnatally, how many families at each center may have elected terminations of pregnancy, or the exact genetic diagnosis (mosaic vs full trisomy). We do not know how many infants received palliative care in the delivery room or were discharged home with hospice care. For infants who died, we do not know if this was due to withholding or failure of interventions. Anomalies are classified based on whether they would typically be associated with neonatal surgical intervention, but we do not know if surgery was performed. Finally, we caution against the use of the study results in counseling about long-term survival or prognosis. The outcomes of this study are limited to NICU discharge, and provide no information about long-term survival or neurodevelopmental outcomes. Despite these limitations, this is the largest study with objective data on infants with T13 or T18 cared for in multiple U.S. NICUs, providing detail on how many infants have neonatal surgical anomalies, which interventions are used, and the associations between major risk factors and survival to discharge home. This fills a major gap in honest physician–parent communication to support families’ goals.
Conclusions
Infants with T13 or T18 receive a wide spectrum of medical interventions in U.S. NICUs. VLBW and neonatal surgical anomalies are risk factors for higher NICU mortality. Medical interventions are not necessarily associated with improved survival to NICU discharge, and the majority of infants discharged home from the NICU receive minimal intervention. For families whose goal is to take their infant home from the NICU with full, limited or end of life interventions, these data can be used to individualize counseling to support those goals.
References
Boghossian NS, Hansen NI, Bell EF, Stoll BJ, Murray JC, Carey JC et al. Mortality and morbidity of VLBW infants with trisomy 13 or trisomy 18. Pediatrics 2014; 133: 226–235.
Brewer CM, Holloway SH, Stone DH, Carothers AD, FitzPatrick DR . Survival in trisomy 13 and trisomy 18 cases ascertained from population based registers. J Med Genet 2002; 39 (9): e54.
Kosho T, Nakamura T, Kawame H, Baba A, Tamura M, Fukushima Y . Neonatal management of trisomy 18: clinical details of 24 patients receiving intensive treatment. Am J Med Genet A 2006; 140 (9): 937–944.
Janvier A, Farlow B, Wilfond BS . The experience of families with children with trisomy 13 and 18 in social networks. Pediatrics 2012; 130 (2): 293–298.
Graham EM, Bradley SM, Shirali GS, Hills CB, Atz AM . Pediatric Cardiac Care Consortium. Effectiveness of cardiac surgery in trisomies 13 and 18 (from the Pediatric Cardiac Care Consortium). Am J Cardiol 2004; 93 (6): 801–803.
Maeda J, Yamagishi H, Furutani Y, Kamisago M, Waragai T, Oana S et al. The impact of cardiac surgery in patients with trisomy 18 and trisomy 13 in Japan. Am J Med Genet A 2011; 155A (11): 2641–2646.
Lin HY, Lin SP, Chen YJ, Hsu CH, Kao HA, Chen MR et al. Clinical characteristics and survival of trisomy 13 in a medical center in Taiwan, 1985-2004. Pediatr Int 2007; 49 (3): 380–386.
Carter PE, Pearn JH, Bell J, Martin N, Anderson NG . Survival in trisomy 18. Life tables for use in genetic counselling and clinical paediatrics. Clin Genet 1985; 27 (1): 59–61.
Goldstein H, Nielsen KG . Rates and survival of individuals with trisomy 13 and 18. Data from a 10-year period in Denmark. Clin Genet 1988; 34 (6): 366–372.
Irving C, Richmond S, Wren C, Longster C, Embleton ND . Changes in fetal prevalence and outcome for trisomies 13 and 18: a population-based study over 23 years. J Matern Fetal Neonatal Med 2011; 24 (1): 137–141.
Niedrist D, Riegel M, Achermann J, Schinzel A . Survival with trisomy 18—data from Switzerland. Am J Med Genet A 2006; 140 (9): 952–959.
Rasmussen SA, Wong LY, Yang Q, May KM, Friedman JM . Population-based analyses of mortality in trisomy 13 and trisomy 18. Pediatrics 2003; 111 (4 Pt 1): 777–784.
Vendola C, Canfield M, Daiger SP, Gambello M, Hashmi SS, King T et al. Survival of Texas infants born with trisomies 21, 18, and 13. Am J Med Genet A 2010; 152 A (2): 360–366.
Bruns D . Birth history, physical characteristics, and medical conditions in long-term survivors with full trisomy 13. Am J Med Genet A 2011; 155 A (11): 2634–2640.
Wu J, Springett A, Morris JK . Survival of trisomy 18 (Edwards syndrome) and trisomy 13 (Patau Syndrome) in England and Wales: 2004-2011. Am J Med Genet A 2013; 161 (10): 2512–2518.
Root S, Carey JC . Survival in trisomy 18. Am J Med Genet 1994; 49 (2): 170–174.
Redheendran R, Neu RL, Bannerman RM . Long survival in trisomy-13-syndrome: 21 cases including prolonged survival in two patients 11 and 19 years old. Am J Med Genet 1981; 8 (2): 167–172.
Petek E, Pertl B, Tschernigg M, Bauer M, Mayr J, Wagner K et al. Characterisation of a 19-year-old "long-term survivor" with Edwards syndrome. Genet Couns 2003; 14 (2): 239–244.
Peroos S, Forsythe E, Pugh JH, Arthur-Farraj P, Hodes D . Longevity and Patau syndrome: what determines survival? BMJ Case Rep 2012; 2012: bcr0620114381.
Hsiao CC, Tsao LY, Chen HN, Chiu HY, Chang WC . Changing clinical presentations and survival pattern in trisomy 18. Pediatr Neonatol 2009; 50 (4): 147–151.
Bruns D, Campbell E . Twenty‐two survivors over the age of 1 year with full trisomy 18: presenting and current medical conditions. Am J Med Genet Part A 2014; 164 (3): 610–619.
Nelson KE, Hexem KR, Feudtner C . Inpatient hospital care of children with trisomy 13 and trisomy 18 in the United States. Pediatrics 2012; 129 (5): 869–876.
Tsukada K, Imataka G, Suzumura H, Arisaka O . Better prognosis in newborns with trisomy 13 who received intensive treatments: a retrospective study of 16 patients. Cell Biochem Biophys 2012; 63 (3): 191–198.
Kaneko Y, Kobayashi J, Yamamoto Y, Yoda H, Kanetaka Y, Nakajima Y et al. Intensive cardiac management in patients with trisomy 13 or trisomy 18. Am J Med Genet A 2008; 146 A (11): 1372–1380.
Janvier A, Watkins A . Medical interventions for children with trisomy 13 and 18: what is the value of a short disabled life? Acta Paediatr 2013; 102: 1112–1117.
Wyllie JP, Wright MJ, Burn J, Hunter S . Natural history of trisomy 13. Arch Dis Child 1994; 71 (4): 343–345.
Yates AR, Hoffman TM, Shepherd E, Boettner B, McBride KL . Pediatric sub-specialist controversies in the treatment of congenital heart disease in trisomy 13 or 18. J Genet Couns 2011; 20 (5): 495–509.
Cereda A, Carey JC . The trisomy 18 syndrome. Orphanet J Rare Dis 2012; 7 (1): 1.
Pont SJ, Robbins JM, Bird TM, Gibson JB, Cleves MA, Tilford JM et al. Congenital malformations among liveborn infants with trisomies 18 and 13. Am J Med Genet A 2006; 140 (16): 1749–1756.
Parikh A, Mitchell A . Congenital anomalies. In: Martin R, Fanaroff A, Walsh M (eds). Fanaroff and Martin's Neonatal-Perinatal Medicine 10th edn. Saunders, 2015; 436.
Madan-Khetarpal S, Arnold G . Genetic disorders and dysmorphic conditions. In: Zitelli B, McIntire S, Nowalk A (eds). Atlas of Pediatric Physical Diagnosis, 6th edn. Saunders: Philadelphia, 2012; 1.
Boghossian NS, Horbar JD, Carpenter JH, Murray JC, Bell EF, Vermont Oxford Network. Major chromosomal anomalies among very low birth weight infants in the Vermont Oxford Network. J Pediatr 2012; 160 (5): 774–780, e11.
Adams-Chapman I, Hansen NI, Shankaran S, Bell EF, Boghossian NS, Murray JC et al. Ten-year review of major birth defects in VLBW infants. Pediatrics 2013; 132 (1): 49–61.
Bruns D . Erring on the side of life: children with rare trisomy conditions, medical interventions and quality of life. J Genet Disord Genet Rep 2013; 2 (1).
Springett A, Wellesley D, Greenlees R, Loane M, Addor M, Arriola L et al. Congenital anomalies associated with trisomy 18 or trisomy 13: a registry‐based study in 16 european countries, 2000–2011. Am J Med Genet Part A 2015; 167 (12): 3062–3069.
McGraw MP, Perlman JM . Attitudes of neonatologists toward delivery room management of confirmed trisomy 18: potential factors influencing a changing dynamic. Pediatrics 2008; 121 (6): 1106–1110.
Ishitsuka K, Matsui H, Michihata N, Fushimi K, Nakamura T, Yasunaga H . Medical procedures and outcomes of Japanese patients with trisomy 18 or trisomy 13: Analysis of a nationwide administrative database of hospitalized patients. Am J Med Genet Part A 2015; 167 (8): 1816–1821.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Acharya, K., Leuthner, S., Clark, R. et al. Major anomalies and birth-weight influence NICU interventions and mortality in infants with trisomy 13 or 18. J Perinatol 37, 420–426 (2017). https://doi.org/10.1038/jp.2016.245
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.245
This article is cited by
-
The short-term mortality and morbidity of very low birth weight infants with trisomy 18 or trisomy 13 in Japan
Journal of Human Genetics (2021)
-
Medical and surgical interventions and outcomes for infants with trisomy 18 (T18) or trisomy 13 (T13) at children’s hospitals neonatal intensive care units (NICUs)
Journal of Perinatology (2021)
-
Cardiac Surgery in Trisomy 13 and 18: A Guide to Clinical Decision-Making
Pediatric Cardiology (2020)
-
NICU management and outcomes of infants with trisomy 21 without major anomalies
Journal of Perinatology (2018)
-
Prenatal counseling and parental decision-making following a fetal diagnosis of trisomy 13 or 18
Journal of Perinatology (2018)