Abstract
Objective:
(1) Evaluate the effect of different medications on pain and stress in neonates during nonemergent endotracheal intubation; (2) determine whether gestational age affects medication use; (3) determine whether better sedation results in a decrease in the number of attempts and/or total time for the procedure.
Study design:
Prospective observational study. Infant responses were measured using a clinical pain scale and blood glucose, a biochemical marker of acute stress.
Result:
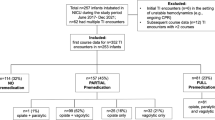
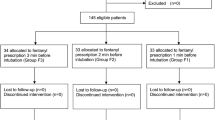
A total of 166 infants were included, with adjusted gestational ages 24 to 44 weeks at the time of procedure. Premedication regimens included no medication (‘none,’ 27%), morphine (19%), morphine+midazolam (11%), fentanyl (14%), fentanyl+midazolam (19%) and midazolam alone (10%). Fentanyl+midazolam resulted in lower pain scores and less increase in blood glucose (both P<0.0001). No other regimen was different from ‘none’. The most immature infants were less likely to receive premedication (P=0.023), although their pain scores and blood glucose responses were similar to more mature infants. None of the medication regimens reduced the total procedure time (P=0.55) or the number of attempts (P=0.145).
Conclusion:
Only fentanyl+midazolam significantly attenuated both the clinical pain score and the increase in blood glucose. Less mature infants had responses similar to those of more mature infants, but were less likely to receive premedication. None of the regimens decreased the time or number of attempts required for successful intubation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Sarkar S, Schumacher RE, Baumgart S, Donn SM . Are newborns receiving premedication before elective intubation? J Perinatol 2006; 26: 286–289.
Stevens B, Johnson C, Gibbins S . Pain assessment in neonates. Anand KJS, Stevens BJ, McGrath PJ (eds). Pain In Neonates, 2nd edn. Elsevier: Edinburgh, UK, 2000; 101–130.
Kumar P, Denson SE, Mancuso TJ, Committee on Fetus and Newborn, Section on Anesthesiology and Pain Medicine. Premedication for nonemergency endotracheal intubation in the neonate. Pediatrics 2010; 125: 608–615.
Brummelte S, Grunau RE, Chau V, Poskitt KJ, Brant R, Vinall J et al. Procedural pain and brain development in premature newborns. Ann Neurol 2012; 71: 385–396.
McPherson C, Grunau RE . Neonatal pain control and neurologic effects of anesthetics and sedatives in preterm infants. Clin Perinatol 2014; 41: 209–227.
Vinall J, Grunau RE, Brant R, Chau V, Poskitt KJ, Synnes AR et al. Slower postnatal growth is associated with delayed cerebral cortical maturation in preterm newborns. Sci Transl Med 2013; 5: 168ra8.
Zwicker JG . Motor impairment in very preterm infants: implications for clinical practice and research. Dev Med Child Neurol 2014; 56 (6): 514–515.
Carbajal R, Lenclen R, Jugie M, Paupe A, Barton BA, Anand KJS . Morphine does not provide adequate analgesia for acute procedural pain among preterm neonates. Pediatrics 2005; 115: 1494–1500.
Oei J, Hari R, Butha T, Lui K . Facilitation of neonatal nasotracheal intubation with premedication: a randomized controlled trial. J Paediatr Child Health 2002; 38: 146–150.
Lemyre B, Doucette J, Kalyn A, Gray S, Marrin ML . Morphine for elective endotracheal intubation in neonates: a randomized trial. BMC Pediatr 2004; 4: 20.
Pereira e Silva Y, Gomez RS, Marcatto JDO, Maximo TA, Barboas RF, Silva ACS . Morphine versus remifentanil for intubating preterm neonates. Arch Dis Child Fetal Neonatal Ed 2007; 92: F293–F299.
Lilien LD, Rosenfield RL, Baccaro MM, Pildes RS . Hyperglycemia in stressed small premature neonates. J Pediatr 1979; 94: 454–459.
Anand KJS, Sippell WG, Schofield NM, Aynsley-Green A . Does halothane anaesthesia decrease the metabolic and endocrine stress responses of newborn infants undergoing operation? Br Med J 1988; 29: 688–672.
Srinivasan G, Jain R, Pildes RS, Kannan CR . Glucose homeostasis during anesthesia and surgery in infants. J Pediatr Surg. 1989; 21 (8): 718–721.
Decaro MH, Vain NE . Hyperglycaemia in preterm neonates: What to know, what to do. Early Hum Dev 2011; 87 (Suppl 1): S19–S22.
Bozza P, Morini F, Conforti A, Sgro S, Laviani Mancinelli R, Ottino S et al. Stress and ano-colorectal surgery in newborn/infant: role of anesthesia. Pediatr Surg Int 2012; 28 (8): 821–882.
Carbajal R, Paupe A, Hoenn E, Lenclen R, Olivier-Martin M . APN: Evaluation of a behavioral scale of acute pain in newborn infants. Arch Pediatr 1997; 4: 623–628.
Sisto R, Bellieni CV, Perrone S, Buonocore G . Neonatal pain analyzer: development and validation. Med Biol Eng Comput 2006; 44: 841–845.
VanLooy JW, Schumacher RE, Bhatt-Mehta V . Efficacy of a premedication algorithm for nonemergent intubation in a neonatal intensive care unit. Ann Pharmacother 2008; 42: 947–955.
Ghanta S, Abdel-Latif ME, Lui K, Ravindranathan H, Awad J, Oei J . Propofol compared with the morphine, atropine, and suxamethonium regimen as induction agents for neonatal endotracheal intubation: a randomized, controlled trial. Pediatrics 2007; 119: e1248.
Lemyre B, Cheng R, Gaboury I . Atropine, fentanyl and succinylcholine for non-urgent intubations in newborns. Arch Dis Child Fetal Neonatal Ed 2009; 94: F439–F442.
Papoff P, Mancuso M, Caresta E, Moretti C . Effectiveness and safety of propofol in newborn infants. Pediatrics 2008; 121: 448–44.
Attardi DM, Paul DA, Tuttle DJ, Greenspan JS . Premedication for intubation in neonates. Arch Dis Child Fetal Neonatal Ed 2000; 83: F161.
Anand KJS, International Evidence-Based Group for Neonatal Pain. Consensus statement for the prevention and management of pain in the newborn. Arch Pediatr Adolesc Med 2001; 155: 173–180.
Feltman DM, Weiss MG, Nicoski P, Sinacore J . Rocuronium for nonemergent intubation of term and preterm infants. J Perinatol 2010; 31 (1): 38–43.
Choong K, AlFaleh K, Doucette J, Gray S, Rich B, Verhey L et al. Remifentanil for endotracheal intubation in neonates:a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed 2010; 95 (2): F80–F84.
Roberts KD, Leone TA, Edwards WH, Rich WD, Finer NN . Premedication for nonemergent neonatal intubations: a randomized, controlled trial comparing atropine and fentanyl to atropine, fentanyl, and mivacurium. Pediatrics 2006; 118 (4): 1583–1591.
Acknowledgements
No financial support was received for this study, and the authors have no financial conflict of interest to disclose. There were no study sponsors involved in the study design, collection, analysis, and interpretation of data; the writing of the report; and the decision to submit the paper for publication. Curtis Caldwell wrote the first draft of the manuscript. There were no grants or other form of payment given to anyone to produce this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Caldwell, C., Watterberg, K. Effect of premedication regimen on infant pain and stress response to endotracheal intubation. J Perinatol 35, 415–418 (2015). https://doi.org/10.1038/jp.2014.227
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.227
This article is cited by
-
Should less invasive surfactant administration (LISA) become routine practice in US neonatal units?
Pediatric Research (2023)
-
Practical approaches to sedation and analgesia in the newborn
Journal of Perinatology (2021)
-
Moving from controversy to consensus: premedication for neonatal intubation
Journal of Perinatology (2018)