Abstract
Objectives: The purpose of our study was to determine the frequency of aspirin administration among patients with acute myocardial infarction (MI) as dictated by physicians practicing in the United States.
Background: Aspirin (ASA), a widely available, inexpensive and generally well-tolerated platelet inhibitor, is recommended for patients with acute coronary syndromes, including acute MI. However, there is concern that aspirin is underutilized in daily clinical practice.
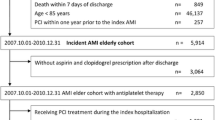
Methods: Early (<24 hours) and predischarge ASA administration were determined among 220,171 patients with suspected acute MI enrolled in the Second National Registry of Myocardial Infarction (NRMI 2) between June, 1994 and April 30, 1996.
Results: Overall, 165,122 (74.9%) of patients received ASA within 24 hours of hospital admission, whereas 55,049 patients did not. Early ASA recipients were younger, more often male, arrived at the hospital earlier, and were more likely to be classified as Killip Class II or less compared to those who did not receive ASA. Patients who received aspirin were also more likely to have chest pain, electrocardiographic ST segment elevation, and tended to arrive at the hospital earlier than those who did not receive ASA. However, over 20% of patients with ST segment elevation did not receive early ASA therapy.
From the total cohort of early ASA recipients, only 69% received ASA at the time of hospital discharge. Trends in early and pre-discharge aspirin administration over a 2 year time period in all patients (72.6 to 75.1% and 71.5 to 74.6%, respectively; p < 0.001) and in specific patient subsets were encouraging with a gradual but steady increase; however, utilization remained comparatively low in women and the elderly. By multivariable analysis, in-hospital recurrent MI (OR 0.90, 95% CI; .78–1.0, p = 0.04), stroke (OR 0.65, 95% CI, .52–.80, p < 0.001) and death (OR 0.24, 95% CI, .22–.26, p < 0.001) occurred less frequently when ASA was administered within 24 hours of hospitalization.
Conclusion: Aspirin is currently underutilized in routine clinical practice as both primary and adjunctive forms of therapy in MI, especially among patients known to be at risk for recurrent cardiothrombotic events. The targeted and timely use of aspirin reduces early cardiovascular events and should remain a priority in national health care efforts.
Similar content being viewed by others
References
Ridker PM, Manson JE, Gaziano JM, Buring JE, Hennelcens CH. Low-dose aspirin therapy for chronic stable angina: A randomized, placebo-controlled clinical trial. Ann Intern Med 1991;114:835–839.
Lewis HD, Davis JW, Archibald DG, Steinke WE, Smitherman TC, Doherty JE, Schnaper HW, LeWinter MM, Linares E, Douget JM, Sabharwal SC, Chesler E, DeMots H. Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina: Results of a Veterans Administration cooperative study. N Engl J Med 1983; 309:396–403.
Théroux P, Ouimet H, McCans J, Latour J-G, Joly P, Levy G, Pelletier E, Juneau M, Stasiak J, DeGuise P, Pelletier G, Rinzler D, Waters DD. Aspirin, heparin or both to treat acute unstable angina. N Engl J Med 1988;319:1107–1111.
The RISC Group. Risk of myocardial infarction and death during treatment with low dose aspirin and intravenous heparin in men with unstable coronary artery disease. Lancet 1990;336:827–830.
Nyman I, Larsson H, Wallentin L, Research Group on Instability in Coronary Artery Disease in Southeast Sweden. Prevention of serious cardiac events by low-dose aspirin in patients with silent myocardial ischemia. Lancet 1992;340: 497–501.
ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Randomized trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet 1988; 2:349–360.
Antiplatelet Trialists' Collaboration. Collaborative overview of randomized trials of antiplatelet therapy--I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ 1994;308:81–106.
Goldstein R, Andrews M, Hall W, Moss A, for the Multicenter Myocardial Ischemia Research Group. Marked reduction in long-term cardiac deaths with aspirin after a coronary event. J Am Coll Cardiol 1996;28:326–330.
Schwartz L, Bourassa M, Lespérance J, Aldridge H, Kazim F, Salvatori V, Henderson M, Bonan R, David P. Aspirin and dipyridamole in the prevention of restenosis after percutaneous transluminal coronary angioplasty. N Engl J Med 1988;318:1714–1719.
Fuster V, Chesebro JH. Role of platelets and platelet inhibitors in aortocoronary artery vein-graft disease. Circulation 1986;73:227–232.
Rajah SM, Salter MC, Donaldson DR, Subba Rao R, Boyle RM, Partridge JB, Watson DA. Acetylsalicylic acid and dipyridimole improve the early patency of corto-coronary bypass grafts. A double-blind, placebo-controlled, randomized trial. J Thoracic Cardiovasc Surg 1985;90:373–376.
Chesebro JH, Fuster V, Elveback LR, Clements IP, Smith HC, Holmes DR Jr, Bardsley WT, Pluth JR, Wallace RB, Puga FJ, et al. Effect of dipyridamole and aspirin on late vein graft patency after coronary bypass operations. N Engl J Med 1984;310:209–214.
Patrono C. Aspirin as an antiplatelet drug. N Engl J Med 1994;330:1287–1294.
Gunnar RM, Bourdillon PDV, Dixon DW, et al. Guidelines for the early management of patients with acute myocardial infarction: A report of the American College of Cardiology / American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee to Develop Guidelines for the Early Management of Patients with Acute Myocardial Infarction). J Am Coll Cardiol 1990;16:249–252.
Dalen JE, Hirsh J, eds. Fourth ACCP Consensus Conference on Antithrombotic Therapy. Chest 1998;114:439–769.
Rogers W, Bowlby L, Chandra N, French W, Gore J, Lambrew C, Rubison M, Tiefenbrunn A, Weaver W, for the participants in the National Registry of Myocardial Infarction. Treatment of myocardial infarction in the United States (1990 to 1993): Observations from the National Registry of Myocardial Infarction. Circulation 1994;90:2103–2114.
Col N, Yarzebski J, Gore J, Alpert J, Goldberg R. Does aspirin consumption affect the presentation or severity of acute myocardial infarction? Arch Intern Med 1995;155: 1386–1389.
Krumholtz H, Radford M, Ellerbeck E, Hennen J, Meehan T, Petrillo M, Wang Y, Kresowik T, Jencks S. Aspirin in the treatment of acute myocardial infarction in elderly Medicare beneficiaries: patterns of use and outcomes. Circulation 1995;92:2841–2847.
Ellerbeck E, Jencks S, Radford M, Kresowik T, Craig A, Gold J, Krumholtz H, Vogel R. Quality of care for Medicare patients with acute myocardial infarction: A four-state pilot study from the Cooperative Cardiovascular Project. JAMA 1995;273:1509–1514.
Meehan T, Hennen J, Radford M, Petrillo M, Elstein P, Ballard D. Process and outcome of care for acute myocardial infarction among medicare beneficiaries in Connecticut: A quality improvement demonstration project. Ann Intern Med 1995;122:928–936.
Lee K, Woodlief L, Topol E, Weaver W, Betrice A, Col J, Simoons M, Aylward P, Van deWerf F, Califf R, for the GUSTO-I Investigators. Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction: Results from an international trial of 41,021 patients. Circulation 1995;91:1659–1668.
Krumholtz H, Radford M, Ellerbeck E, Hennen J, Meehan T, Petrillo M, Wang Y, Jencks S. Aspirin for secondary prevention after acute myocardial infarction in the elderly: Prescribed use and outcomes. Ann Intern Med 1996;124:292–298.
Giugliano RP, Camargo Jr CA, Lloyd-Jones, et al. Elderly patients receive less agressive medical and invasive management of unstable angina. Arch Intern Med 1998;158: 1113–1120.
Gurwitz J, Gore JM, Goldberg R, Rubison M, Chandra N, Rogers WJ, for the participants in the National Registry of Myocardial Infarction. Recent age-related trends in the use of thrombolytic therapy in patients who have had acute myocardial infarction. Ann Intern Med 1996;124:283–291.
Gil M, Marrugat J, Sala J. et al., for the REGICOR Investigators. Relationship of therapeutic improvements and 28-day case fatality in patients hospitalized with acute myocardial infarction between 1978 and 1993 in the REGICOR study, Gerona Spain. Circulation 1999;99:1767–1773.
Lamas G, Pfeffer M, Hamm P, Wertheimer J, Rouleau J-L, Braunwald E, for the SAVE Investigators. Do the results of randomized clinical trials of cardiovascular drugs influence medical practice? N Engl J Med 1992;327:241–247.
Manning M, Stevenson D, Mathison D. Reactions to aspirin and other nonsteroidal anti-inflammatory drugs. Immunol & Allergy Clin N Amer 1992;12:611–631.
Feigenbaum B, Simon R, Stevenson D. Aspirin intolerance. Ann Allergy, Asthma & Immunol 1995;74:193–194.
American Hospital Formulary Service Drug Information 97. McEvoy GK, editor. 1997;1459–1480.
Ryan TJ, Anderson JL, Antman EM, Branoff BA, Brooks NH, Califf RM, Hillis LD, Hiratzlod LF, Rapaport E, Riegel BJ, Russell RO, Smith EE III, Weaver WD. ACC/AHA guidelines for the management of patients with acute myocardialinfarction: A report of the American College of Cardiology (American Heart Association Task Force on Practice Guidelines, Committee on Management of Acute Myocardial Infarction). JAmColl Cardiol 1996;28:1328–1428.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Becker, R.C., Burns, M., Gore, J.M. et al. Early and Pre-Discharge Aspirin Administration Among Patients with Acute Myocardial Infarction: Current Clinical Practice and Trends in the United States. J Thromb Thrombolysis 9, 207–215 (2000). https://doi.org/10.1023/A:1018706425864
Issue Date:
DOI: https://doi.org/10.1023/A:1018706425864