Abstract
Objectives: This study measured the impact of an educational intervention aimed at heightening rural physicians' awareness of state-of-the-art breast and colorectal cancer therapies.
Methods: Pre- and post-intervention mailed surveys were administered to all primary-care physicians and referring physicians in the seven-county intervention region in North Carolina (NC) and a comparison region in South Carolina (SC).
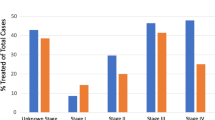
Results: The survey revealed few significant changes in physicians' perspectives that could be attributed to the intervention. Physicians erroneously stated that lumpectomy without follow-up radiation was acceptable for treating breast cancer (55%), failed to indicate that adjuvant therapy was an accepted practice for treating Stage I breast cancer (67%), failed to acknowledge chemotherapy as experimental for Dukes' B colon cancer patients (70%), and failed to recognize a combination of surgery, chemotherapy, and radiation as a standard treatment for rectal cancer (25%).
Conclusions: The low levels of awareness of National Cancer Institute guidelines were reflected in low breast-sparing surgery rates for women living in the intervention region. Stronger consensus on appropriate cancer treatments is needed throughout the medical community in order to reduce undesired variation in rural, community-based cancer care.
Similar content being viewed by others
References
Greenwald P, Sondik EJ, eds (1986) Cancer Control Objectives for the Nation, 1985–2000. NCI Monogr 2: 1-105.
Osteen RT, Cady B, Chmiel JS et al. (1994) 1991 National survey of carcinoma of the breast by the Commission on Cancer. J Am Coll Surg 178: 213-219.
Studnicki J, Schapira DV, Bradham DD, Clark RA, Jarrett A (1993) Response to the National Cancer Institute Alert. Cancer 72: 2986-2992.
Hynes DM (1994) The quality of breast cancer care in local communities: implications for health care reform. Med Care 32: 328-340.
Hand RH, Sener S, Imperato J, Chmiel JS, Sylvester JA, Fremgen A (1992) Hospital variables associated with quality of care for breast cancer patients. JAMA 266: 3429-3432.
Ermann D (1990) Rural health care: the future of the hospital. Med Care Rev 47: 33-73.
Keeler EB, Rubenstein LV, Kahn KL, et al. (1992) Hospital characteristics and quality of care JAMA 268: 1709-1714.
Howe HL, Katterhagen JG, Yates, J, Lehnherr M (1992) Urban-rural differences in the management of breast cancer. Cancer Causes Control 3: 533-539.
Curtiss CP (1993) Trends and issues for cancer care in rural communities. Rural Nursing 28: 241-251.
McFall SL, Warnecke RB, Kaluzny AD, Ford L (1994) Physician and practice characteristics associated with judgments about breast cancer treatment. Med Care 32: 106-117.
McFall SL, Warnecke RB, Kaluzny AD, Ford L (1996) Practice setting and physician influences on judgments of colon cancer treatments by community physicians. Health Serv Res 31: 5-18.
Cooper MR, Ricketts TC (1998) Reaching Cancer for Cancer Care (REACH) Project Evaluation Report, 1998. Winston-Salem NC: Wake Forest University Comprehensive Cancer Center. April.
Kaluzny AD, Warnecke R, Gillings D (1992) Assessment of the implementation and impact of the community clinical oncology program, Phase II. Vol. 1. Overview, Findings, and Recommendations. Chapel Hill, NC: Cecil G. Sheps Center for Health Services Research, the University of North Carolina at Chapel Hill.
Belanger D, Moore M, Tannock I (1991) How American oncologists treat breast cancer: an assessment of the influence of clinical trials. J Clin Oncol 9: 7-16.
Greer Al (1977) Advances in the study of diffusion of innovation in health care organizations, Milbank Memorial Fund Quarterly 55: 505-532.
Kosecoff J, Kanouse DE, Rogers WH, McCloskey L, Winslow CM, Brook RH (1987) Effects of the National Institutes of Health Consensus Development Program on physician practices. JAMA 258: 2708-2713.
Olivotto IA, Coldman AJ, Hislop TG, et al. (1997) Compliance with practice guidelines for node-negative breast cancer. J Clin Oncol 15: 216-222.
Mittman BS, Tonesk X, Jacobson PD (1992) Implementing clinical practice guidelines: social influence strategies and practitioner behavior change. Qual Rev Bull 18: 413-422.
Kanouse DE, Jacoby I (1988) When does information change practitioners' behavior? Int J Technol Assess Health Care 4: 27-33.
Ford LG (1989) Therapy: state-of-the-art assessment of quality. Cancer 64: 219-222.
Greer AL (1988) The state of the art versus the state of the science. The diffusion of new medical technologies into practice. Int J Technol Assess Health Care 4: 5-26.
Grady KE, Wallston BS (1988) Research in Health Care Settings. Newbury Park: Sage.
Author information
Authors and Affiliations
Additional information
(S.E.T. is currently with the MD Anderson Comprehensive Cancer Center, University of Texas Medical College, USA)
Rights and permissions
About this article
Cite this article
Hatzell, T.A., Ricketts, T.C., Tropman, S.E. et al. Rural physicians' understanding of the state-of-the-art in breast, colon and rectum cancer treatment. Cancer Causes Control 10, 261–267 (1999). https://doi.org/10.1023/A:1008996227202
Issue Date:
DOI: https://doi.org/10.1023/A:1008996227202