Abstract
Introduction: The transgenic mouse is a popular model for human inherited cardiac disease. Electrophysiology (EP) studies have recently been performed in transgenic mice to characterize the electrical phenotype of the heart. However, little is known regarding the impact of experimental conditions or model selection on the outcome of EP studies in mice.
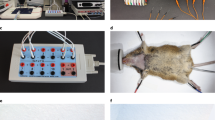
Methods and Results: We investigated the effects of experimental conditions on mouse cardiac EP by (1) comparing the findings of transesophageal pacing with those of invasive intracardiac pacing, (2) elucidating the effects of commonly used anesthetic agents, and (3) determining the impact of changes in body temperature. We also investigated the effects of model selection by (1) studying the dependence on mouse strain, and (2) exploring the effects of age. We found that EP parameters derived by both transesophageal and intracardiac pacing/recordings methods were similar. On the other hand, the anesthetic mixture of ketamine, xylazine, and acepromazine had profound effects on cardiac EP compared to sodium pentobarbital or isoflurane. Meanwhile, compared to normal body temperature (97–99 F), low body temperature (92–94 F) prolonged most cardiac EP parameters, while high body temperature (102–104 F) had little effect. Heart rate was a sensitive indicator of changes in body temperature. Significant differences were observed in specialized conduction system properties among the mouse strains studied (FVB, C57, and DBA). Furthermore, atrial electrical remodeling was evidently associated with age, while ventricular electrical properties were virtually unaltered. In comparison with corresponding invasive EP parameters, we found that the QT interval was not a reliable EP index in the mouse.
Conclusions: Cardiac EP variability may result from differences in experimental techniques including anesthesia and body temperature and from differences in mouse selection including strain and age. The influence of these factors should be considered when characterizing the electrical phenotype of transgenic mice in cardiovascular research.
Similar content being viewed by others
References
James JF, Hewett TE, Robbins J. Cardiac physiology in transgenic mice. Circ Res 1998;82:407–415.
Germann J, Berul CI. Cardiac electrophysiology in genetically engineered mice. J Cardiovasc Electrophysiol 2000;11:354–368.
Richards AG, Simonson E, Visscher MB. Electrocardiogram and pohonogram of adult and newborn mice in normal conditions and under the effect of cooling, hypoxia and potassium. Am J Physiol 1953;174:293–298.
GoldbargAN, Hellerstein HK, Bruell JH, DaroczyAF. Electrocardiogram of th enormal mouse, Mus musculus: General considerations and genetic aspects. Cardiovasc Res 1968;2:93–99.
Doevendans PA, Daemen MJ, de Muinck ED, Smits JF. Cardiovascular phenotyping in mice. Cardiovasc Res 1998;39:34–49.
Berul CI, Aronovitz MJ, Wang PJ, Mendelsohn ME. In vivo cardiac electrophysiology studies in the mouse. Circulation 1996;94:2641–2648.
Vitelli LL, Crow RS, Shahar E, Hutchinson RG, Rautaharju PM, Folsom AR. Electrocardiographic findings in a healthy biracial population. Atherosclerosis Risk in Communities (ARIC) Study Investigators. Am J Cardiol 1998;81:453–459.
Chapman N, Mayet J, Ozkor M, Foale R, Thom S, Poulter N. Ethnic and gender differences in electrocardiographic QT length and QT dispersion in hypertensive subjects. J Hum Hypertens 2000;14:403–405.
Hoit BD, Kiatchoosakun S, Restivo J, Kirkpatrick D, Olszens K, Shao H, Pao YH, Nadeau JH. Naturally occurring variation in cardiovascular traits among inbred mouse strains. Genomics 2002;79:679–685.
Roth DM, Swaney JS, Dalton ND, Gilpin EA, Ross J Jr. Impact of anesthesia on cardiac function during echocardiography in mice. Am J Physiol Heart Circ Physiol 2002;282:H2134–H2140.
Mitchell GF, Jeron A, Koren G. Measurement of heart rate and Q-T interval in the conscious mouse. Am J Physiol Heart Circ Physiol 1998;274:H747–H751.
Arras M, Autenried P, Rettich A, Spaeni D, Rulicke T. Optimization of intraperitoneal injection anesthesia in mice: Drugs, dosages, adverse effects, and anesthesia depth. Comp Med 2001;51:443–456.
Sessler DI. Perioperative heat balance. Anesthesiology 2000;92:578–596.
Dardai E, Heavner JE. Respiratory and cardiovascular effects of halothane, isoflurane and enflurane delivered via a Jackson-Rees breathing system in temperature controlled and uncontrolled rats. Methods Find Exp Clin Pharmacol 1987;9:717–720.
Denes P, Wu D, Dhingra R, Pietras RJ, Rosen KM. The effects of cycle length on cardiac refractory periods in man. Circulation 1974;49:32–41.
Attwell D, Cohen I, Eisner DA. The effects of heart rate on the action potential of guinea-pig and human ventricular muscle. J Physiol 1981;313:439–461.
Franz MR, Swerdlow CD, Liem LB, Schaefer J. Cycle length dependence of human action potential duration in vivo. Effects of single extrastimuli, sudden sustained rate acceleration and deceleration, and different steady state frequencies. J Clin Invest 1988;82:972–979.
Arnold L, Page J, Attwell D, Cannell M, Eisner DA. The dependence on heart rate of the human ventricular action potential duration. Cardiovasc Res 1982;16:547–551.
Josephson ME. Clinical Cardiac Electrophysiology. Techniques and Interpretations. Malvern, Pennsylvania: Lea & Febiger, 2nd edition, 1982:41–48.
Morady F, Kadish AH, Toivonen LK, Kushner JA, Schmaltz S. The maximum effect of an increase in rate on human ventricular refractoriness. PACE 1988;11:2223–2234.
Danik S, Cabo C, Chiello C, Kang S, Wit AL, Coromilas J. Correlation of repolarization of ventricular monophasic action potential with ECG in the murine heart. Am J Physiol Heart Circ Physiol 2002;283:H372–H381.
Kuo HC, Cheng CF, Clark RB, Lin JJC, Lin JLC, Hoshijima M, Nguyen-Tran VTB, Gu Y, Ikeda Y, Chu PH, Ross J Jr, Giles WR, Chien KR. A defect in the Kv channelinteracting protein 2 (KChlP2) gene leads to a complete loss of Ito and confers susceptibility to ventricular tachycardia. Cell 2001;107:801–813.
Butz GM, Davisson RL. Long-term telemetric measurement of cardiovascular parameters in awake mice: A physiological genomics tool. Physiol Genomics 2001;5:89–97.
Hara Y, Chugun A, Nakaya H, Kondo H. Tonic block of the sodium and calcium currents by ketamine in isolated guinea pig ventricular myocytes. J Vet Med Sci 1998;60:479–483.
Rao S, Verkman AS. Analysis of organ physiology in transgenic mice. Am J Physiol Cell Physiol 2000;279:C1–C18.
Wartenberg HC, Wartenberg JP, Urban BW. Human cardiac sodium channels are affected by pentobarbital. Eur J Anaesthesiol 2001;18:306–313.
Nattel S, Wang ZG, Matthews C. Direct electrophysiological actions of pentobarbital at concentrations achieved during general anesthesia. Am J Physiol Heart Circ Physiol 1990;259:H1743–H1751.
Weigt HU, Kwok WM, Rehmert GC, Bosnjak ZJ. Sensitization of the cardiac Na channel to alpha1-adrenergic stimulation by inhalation anesthetics: Evidence for distinct modulatory pathways. Anesthesiology 1998;88:125–133.
Riley DC, Schmeling WT, al-Wathiqui MH, Kampine JP, Warltier DC. Prolongation of the QT interval by volatile anesthetics in chronically instrumented dogs. Anesth Analg 1988;67:741–749.
Hannon JD, Cody MJ. Effects of volatile anesthetics on sarcolemmal calcium transport and sarcoplasmic reticulum calcium content in isolated myocytes. Anesthesiology 2002;96:1457–1464.
Fujimoto K, Bosnjak ZJ, Kwok WM. Isoflurane-induced facilitation of the cardiac sarcolemmal K(ATP) channel. Anesthesiology 2002;97:57–65.
Hahn N, Hornchen U, Eichelkraut W. [Effects of intravenous anaesthetics on excitation, conduction, and refractory parameters of the heart. Experimental study in the dog] Arzneimittelforschung 1995;45:462–471.
HahnN, HornchenU, EichelkrautW. [Effects of anesthesia with inhalation anesthetics on excitation, conduction and refractory parameters of the heart. Experiments in dogs] Arzneimittelforschung 1996;46:251–256.
ThibaultB, de Bakker JM, Hocini M, Loh P, Wittkampf FH, Janse MJ. Origin of heat-induced accelerated junctional rhythm. J Cardiovasc Electrophysiol 1998;9:631–641.
Spear JF, Moore EN. Modulation of quinidine-induced arrhythmias by temperature in perfused rabbit heart. Am J Physiol Heart Circ Physiol 1998;274:H817–H828.
Kiyosue T, Arita M, Muramatsu H, Spindler AJ, Noble D. Ionic mechanisms of action potential prolongation at low 14 Appleton et al.temperature in guinea-pig ventricular myocytes. J Physiol 1993;468:85–106.
Doubt TJ, Hogan PM. Combined influence of temperature and hydrostatic pressure on cardiac conduction. Undersea Biomed Res 1980;7:211–223.
Franco D, Demolombe S, Kupershmidt S, Dumaine R, Dominguez JN, Roden D, Antzelevitch C, Escande D, Moorman AF. Divergent expression of delayed rectifier K(+) channel subunits during mouse heart development. Cardiovasc Res 2001;52:65–75.
Larsen JA, Kadish AH. Effects of gender on cardiac arrhythmias. J Cardiovasc Electrophysiol 1998;9:655–664.
Berul CI, Christe ME, AronovitzMJ, Maguire CT, Seidman CE, Seidman JG, Mendelsohn ME. Familial hypertrophic cardiomyopathy mice display gender differences in electrophysiological abnormalities. J Interv Card Electrophysiol 1998;2:7–14.
Bevilacqua LM, Maguire CT, Seidman JG, Seidman CE, Berul CI. QT dispersion in alpha-myosin heavy-chain familial hypertrophic cardiomyopathy mice. Pediatr Res 1999;45:643–647.
Gussak I, Chaitman BR, Kopecky SL, Nerbonne JM. Rapid ventricular repolarization in rodents: Electrocardiographic manifestations, molecular mechanisms, and clinical insights. J Electrocardiol 2000;33:159–170.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Appleton, G.O., Li, Y., Taffet, G.E. et al. Determinants of Cardiac Electrophysiological Properties in Mice. J Interv Card Electrophysiol 11, 5–14 (2004). https://doi.org/10.1023/B:JICE.0000035922.14870.56
Issue Date:
DOI: https://doi.org/10.1023/B:JICE.0000035922.14870.56