Introduction
Concussion/mild traumatic brain injury is a worldwide public health problem and accounts for the largest group of brain injuries.Reference Cassidy, Carroll and Peloso 1 - Reference Silverburg, Gardner, Brubacher, Panenka, Li and Iverson 5 Using common data elements (CDEs) to characterize concussion is the most important strategy to begin to address this global burden.Reference Hicks, Giacino, Harrison-Felix, Manley, Valadka and Wilde 2 The implementation of CDEs for concussion can increase the efficiency and effectiveness of clinical treatment, clinical research studies, and data quality, as well as facilitate data sharing and educate new clinical investigators.Reference Mass, Harrison-Felix and Menon 4 Improving concussion surveillance through collection of CDEs is essential to determining whether progress is being made to reduce the burden of concussion on public health.Reference Bell, Taylor and Breiding 6 In spite of this convincing evidence, healthcare providers (HCPs) across Ontario do not collect uniform CDEs on concussion.
One-fifth of adults with concussion experience persisting symptoms (PSs), defined as lasting beyond 3 months of the traumatic event.Reference Cassidy, Carroll and Peloso 1 These may include such symptoms as cognitive impairments, headache, sleep disturbance, disorders of balance, fatigue, dizziness, mood disorders, and depression. 7 Patients in Ontario with PSs may be referred to tertiary care (TC) and wait an average of 7 months to be seen in Ontario.Reference Langer, Bayley and Levy 8 During this wait time, it has been estimated that Ontario could be spending up to $110 million annually, as patients are seeking symptom relief from a diverse range of services, while they wait for TC.Reference Hunt, Zanetti and Kirkham 9 There are currently numerous and diverse concussion care providers across the province.Reference Ellis, Ritchie, Selci, Chu, McDonald and Russell 10 Consistent patient assessment measures for PSs are not widely used in spite of the recommendations of clinical guidelines. As a result, there is a pattern of haphazard collection of information. Patients with PSs are followed over time, but without consistent outcomes measures it is difficult to share information from one clinician to another to ensure continuity of care. For example, using different tools to monitor symptoms precludes the ability to observe patterns and responses to symptom management. Early implementation of CDEs in Ontario could facilitate a streamlined systematic approach to care, improve access to care, help decrease specialty care wait times, reduce patient suffering, and reduce the economic impact of concussion. The Ontario Concussion Care Strategy (OCCS) has successfully established a collaborative network to promote and implement CDEs. The OCCS has recommended and implemented CDEs for TC. The CDEs selected are readily available at no cost, clinically relevant, patient-friendly, easy to interpret, and recognized by the international scientific community. The purposes of the present paper are to: (1) describe the OCCS’s vision for CDEs; (2) interpret the theoretical framework used to recommend CDEs for TC; (3) define the key steps by OCCS to implement CDEs; and (4) consider the strengths and limitations of CDEs in concussion care.
Ontario Concussion Care Strategy (OCCS)
The OCCS consists of a group of multidisciplinary HCPs (physiotherapy, occupational therapy, nursing, physiatry, psychiatry, family, and emergency clinicians) with experience in caring for patients with concussion and collaborating with brain injury advocate groups, patient representatives, and researchers. Participants in the OCCS are from across the province of Ontario: Ottawa, Kingston, Sudbury, Thunder Bay, Toronto, Hamilton, and London. Over 40 participants attended the inaugural meeting in April of 2014, initiated by the St. Michael’s Hospital Head Injury Clinic. The OCCS operates under a model of shared leadership. Members of the OCCS share a common vision, which is to improve concussion care across Ontario and reduce the impact of chronic impairment from concussion. The OCCS identified the first phase of the strategy to achieve this vision as being the implementation of CDEs in TC.
Methods
The International Classification of Functioning Disability and Health Framework
The practice of patient-centred interprofessional care was considered when choosing a theoretical framework for standardized data collection in concussion care. The World Health Organization’s International Classification of Functioning, Disability, and Health (ICF) 16 provided a comprehensive, multidisciplinary, bio-psychosocial model of functioning and disability, and has been previously used to describe neurological trauma in both acute and chronic phases.Reference Laxe, Cieza and Castano-Monsalve 17 , Reference Raggi, Leonardi and Covelli 18 The value of the ICF in interprofessional practice and research has gained international recognition. It has demonstrated strengths in the promotion of a comprehensive perspective on health, ease in the application of this theory to practice, and the ability to enhance communication and collaboration across HCPs.Reference Nguyen, Fayed, Gorter and MacDermid 19 The ICF has been a catalyst for interprofessional education and collaborative practice in other neurological health conditions.Reference Snyman, Von Pressentin and Clarke 20 Table 1 describes the four domains of the ICF framework and the corresponding recommended CDEs for Ontario TC within each domain. Table 1 also outlines the definition and rationale, and references the source of the CDE.
Table 1 Ontario concussion care strategy recommended common data elements for tertiary care

Shading indicates new experimental CDE initiated by OCCS.
The four domains of the ICF framework were used as “building blocks” in the selection of CDEs recommended by the OCCS. The first domain encompasses “body functions and structure,” which specifies the physiological functions of body systems and impairments in body function. In the recommendation of CDEs, the OCCS divided this domain into pre-injury, peri-injury and post-injury body function and structure, to align with parts of the classic injury grid designed by Haddon.Reference Haddon 21 The second domain, “activities,” comprises various activities involved in daily life. The OCCS modified this domain to include characteristics about the person’s activities at the time of the injury, such as date/time of injury and mechanism of injury. The third domain is “participation,” which refers to the nature and extent of the person’s societal functioning. Several examples of CDEs in this domain include marital status, persons living with, employment, and education. Contextual factors comprise the fourth domain. This domain is further divided into “personal factors” (internal influences of functioning), with examples of CDEs including immigration status, ethnicity, alcohol, and drug use, and “environmental factors” (or external influences on functioning), with examples of CDEs in this domain being protective equipment and type of housing.
Key Steps by OCCS to Implement CDEs
The steps in the identification and implementation of CDEs are outlined in Figure 1. First, an environmental scan was conducted with five TC centres in the OCCS. Mapping of patient measures collected at each site revealed limited commonalities across sites. This was a further call to action for the collection of standardized data. Secondly, a CDE subcommittee was established by the OCCS. The subcommittee began reviewing landmark documents on concussion care from provincial and international healthcare jurisdictions (Unites States and Europe). A brief description of the landmark documents is offered below.
-
1. The Ontario Neurotrauma Foundation (ONF) Guidelines for Concussion/mTBI and Persistent Symptoms. 7 Released in 2008 and revised in 2013, these guidelines are written for HCPs implementing evidence-based care for adults with persistent post-concussive symptoms. A comprehensive literature review was undertaken in the development of these guidelines.
-
2. The National Institute of Neurological Disorder and Stroke–Common Data Elements. 14 This initiative was begun in 2007 by international clinical experts building consensus for standardized data acquisition in traumatic brain injury. CDEs became actionable information by enabling comparison across studies.
-
3. The Zurich Consensus Statement on Concussion in Sport.Reference McCrory, Meeuwisse and Aubry 15 Developed by an international panel of sports concussion experts for use by HCPs involved in the care of injured athletes to further inform the treatment and management of sports-related concussion.
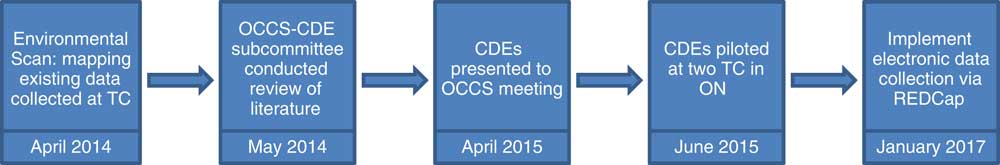
Figure 1 Steps to identification and implementation of CDEs for concussions in Ontario.
Four guiding principles were agreed upon in selecting CDEs. These principles included: (1) CDEs will enhance the standard of practice by selecting clinically relevant measures; (2) CDEs will be dynamic and evolve over time; (3) resources will be needed to review and revise CDEs on a semiannual basis; and (4) CDEs need to be readily available at no cost, easy to implement, easy to collect, and easy to interpret. The subcommittee presented their recommended CDEs to the larger OCCS group. The CDEs were discussed and accepted at a face-to-face meeting in April of 2015. The OCCS CDE subcommittee developed a patient self-reported “baseline patient questionnaire.” This questionnaire embeds the CDEs in a series of questions and standardized screening tools for the patient to complete. Two weeks in advance of the TC clinic appointment, the patient receives the questionnaire by mail, giving them ample time to complete and bring it to their TC appointment. Patients require 20 to 45 minutes to complete the questionnaire. A “significant other” can assist if necessary. Upon subsequent visits to the TC clinic (if required), the OCCS recommends selected CDEs to be repeated in a “self-reported follow-up questionnaire.” CDEs in the follow-up TC questionnaire include repeated measures of symptoms and functional independence (return to work/school and/or return to regular community activities), as well as health, social behaviour, and quality of life.
Clinician-reported CDEs are gathered with a focus on the time immediately after an injury. The CDEs reported include amnesia (before/after injury), loss of consciousness, alteration of consciousness, seizure within 48 hours, vomiting, Glasgow Coma Scale score, and CT scan, as well as mechanism of injury, use of protective equipment, and healthcare services accessed immediately after the injury.
Results
The purpose of this paper was to present the recommended CDEs for TC. Future studies will present aggregate CDE data and results.
Discussion
Strengths of CDEs for Concussion Care
The standardization of concussion care data across the province of Ontario will provide powerful information. CDEs can improve the efficiency of data collection for concussion care while decreasing strain on patients, who are frequently asked to recall information by different HCPs at different time points. CDEs can accompany the patient and be consistently monitored throughout their trajectory of care. The implementation of CDEs can improve the orientation of trainee clinicians by assisting them to more easily identify health conditions among patients for further investigation and advanced management.Reference Wilde, Whiteneck and Bogner 11 Furthermore, without a standardized and consistent approach to data collection for each patient, it is difficult to evaluate whether clinical interventions have been effective. Research-based initiatives using CDEs have been shown to help to advance medical treatments. 3 , Reference Wilkins, Shannon and Brown 12 CDEs allow for ease of evaluation of the impact of medical interventions, including individual patient progress, as well as allowing analyses of multi-site research studies at the local, provincial, national, and international levels.
For many clinical centres across the province, small-scale studies present challenges in terms of the length of time required to obtain a sufficient number of enrolled patients to allow for adequate power in statistical analyses. CDEs allow for sound statistical analyses of aggregate data for use in addressing individual clinic as well as larger population-level questions.Reference Wilde, Whiteneck and Bogner 11 A shared database will help to identify adverse outcomes common to concussion and the associated risk factors, thereby allowing for the development of improved clinical interventions to mitigate these risk factors. Standardization will facilitate high-quality data harmonization by supporting meta-analysis of patient dataReference Mass, Harrison-Felix and Menon 4 and could lay the foundation for the creation of a concussion registry for patients with PSs. The collection of CDEs will enable better characterization of patient trajectory in the years following concussion. Data sharing of standardized de-identified CDEs will provide a large provincial resource for advancing knowledge of short- and long-term outcomes of concussion. Collecting CDEs will shift research questions and move treatment evaluation toward a comparative effectiveness approach. 3 , Reference Mass, Harrison-Felix and Menon 4 , Reference Wilkins, Shannon and Brown 12 This can help to improve Ontario’s ability to address questions about the magnitude, as well as risk factors, protective factors, natural history, and patterns of recovery in concussion and to resolve service gaps to improve resource utilization.
A congruent shared database can establish a basis for comparison with other data sources. The sharing of data methodologies and associated tools, rather than summaries of interpretations of data collected by each individual HCP, can accelerate research progress by allowing independent, unbiased re-analysis of data, as well as re-aggregation, integration, and rigorous comparison with other datasets, tools, and methods.Reference Thompson, Vavilala and Rivara 13 Implementing CDEs province-wide will help to better inform health policy and resource planning. The resulting clinical knowledge accrued from data analyses can be used to establish benchmarks for provincial standards of care.
Limitations of CDEs for Concussion Care
In Ontario, the development of data sharing agreements will require ongoing collaborative work. Steps to sustain data quality will be ongoing. To this end, transcription of paper-based questionnaires to electronic spreadsheets is performed by double entry of questionnaires to minimize data entry errors. At this time, staff and resources to support data collection and management are limited, and student volunteers have been one solution. The quality of patient responses in the self-reported questionnaire requires consideration. The “good old days bias” with self-reported patient data has been identified.Reference Iverson, Lange, Brooks and Rennison 34
Patient feedback on the implementation of CDEs was gathered. Patients expressed symptoms of fatigue when completing the paper-and-pencil questionnaires, likely related to the length of the instruments. Limiting the number of CDEs is a challenging but important consideration in an effort to minimize patient fatigue and maximize patient participation. Moving from paper-based to electronic data capture is a critical next step. The OCCS has planned a system of direct patient data entry into a secure patient-friendly and de-identified web-based system using REDCap.Reference Harris, Taylor, Thielke, Payne, Gonzalez and Conde 35 Utilizing a secure and private web-based data collection system, patients can take the time they need to enter their data at home. The electronic data capture system will have the capacity to construct a large dataset from smaller datasets across the province.
Some OCCS TC sites questioned the utility of certain CDEs and the exclusion of others. Selection and revision of CDEs will be considered a continuing process.Reference Mass, Harrison-Felix and Menon 4 In response and to address the evolving interests and priorities of CDEs, the OCCS established a process of biannual reviews of CDEs. It has also been recognized that selected data elements may be of relevance only to specific subpopulations, and as such require further study for supplemental data elements for Ontario. Examples include CDEs on stress and resilience. Experimental CDEs have been introduced to facilitate novel research inquiry. These include adverse childhood experiences, physical activity levels, pain assessment, and health service utilization. With the implementation of standardized data collection at OCCS sites, each TC site established a data steering committee. These committees regularly monitor and review data quality and provide a forum in which to present clinician and patient feedback for discussion, which is relayed back to the OCCS CDE subcommittee for discussion.
As the number of HCP settings implementing collection of CDEs increases, the possibility of a shared database for patients with concussion across Ontario is becoming a reality. Ongoing challenges to develop a large provincial aggregate electronic database include the integration of proprietary data capture systems and the implementation of resiliency (such as safety nets for a databaseReference Thompson, Vavilala and Rivara 13 and individual health institutional review ethics board approval). The OCCS will require a sophisticated IT platform for electronic data capture, storage, and data use and sharing. A considerable amount of funding and resource personnel will be required to sustain a quality shared database.
Conclusions
The OCCS has taken a methodologically rigorous and collaborative approach to arrive at CDEs to standardize data in concussion care and research in Ontario. This phase-one CDE implementation focused on TC settings. In this phase, data collection has relied on patient self-report. Patients complete a questionnaire to describe demographics, physical environment, risk factors, protective factors, co-morbidities, and other social determinants of their health. Clinician-reported measures in phase one have been limited to focus on immediate post-injury factors. As the CDEs move into phase two, the OCCS may consider adding physical exam findings as well as MRI and/or x-ray findings. As the implementation of CDEs spreads, an abundance of high-quality data will be available to assist HCPs and researchers. These data will have the ability to be used to improve estimates on the magnitude of the problem of concussion, to characterize the experience of concussion by examining symptoms over time, and to assess service delivery. Further, it can be used to identify groups at high risk and to document the characteristics of the patients served and their health outcomes.
Standardized data on concussions will build a surveillance system for better understanding of concussion injuries in Ontario. Ongoing and future observational clinical studies enrolling patients with concussion can be linked across regions and across the province with standardized data. Multi-centre and international clinical research efforts can be facilitated using the internationally recognized CDEs. The results derived from the CDE concussion database will foster prevention strategies and establish priorities for research.
The OCCS invites new partners from across Ontario to join the collaborative network and to promote implementation and spread of CDEs throughout the patient care pathway. Dissemination of the CDEs to other centres of care continues through consultation and collaboration. Scalability and sustainability of CDEs will require human and financial resources. Work is underway to recommend CDEs for emergency departments and family practice clinicians. The CDEs for these care settings will need to match and flow into the pathway of CDEs recommended for TC. Other research has suggested that CDEs can be useful in triage tools to support clinical decisions for timely and appropriate referrals and for early access to specialty care for those patients in need.Reference Silverburg, Gardner, Brubacher, Panenka, Li and Iverson 5
Standardized data collection using CDEs is a promising road map for system-wide improvement in concussion care. While no single measure can capture the progress of a patient after a concussion, the implementation of CDEs can help to shift Ontario toward internationally recognized standard data collection and in so doing yield a more comprehensive, evidence-based approach to care and support rigorous research. Without a common language to report and monitor concussion care, PSs may go unnoticed and undocumented, leading to an increased long-term burden of patient suffering with unnecessary healthcare costs. The ICF theoretical model provides a framework to describe CDEs with regard to functioning and disability in everyday activities. The use of the ICF model allows for ease of communication among HCPs and researchers from different disciplines. The OCCS is working collaboratively to enable the construction of a database to yield high-quality evidence to inform a “big-picture approach” to concussion care across Ontario. The spread of CDEs will help shift Ontario toward a stronger evidence-based approach to care. The implementation of CDEs aligns Ontario with the international movement toward standardized data that is currently being undertaken in the United States and Europe, thereby positioning the province to contribute significantly to reducing the burden of concussion.
Acknowledgments
This project has been supported by the generous donations of Mr. Richard Currie, the CUMBA Foundation, and the Ontario Neurotrauma Foundation. We also thank the partners in OCCS, including The Ottawa Hospital, the Toronto Rehabilitation Institute, the Fowler Kennedy Sports Medicine Clinic, Holland Bloorview Hospital, and Lakehead University.
Disclosures
All the authors hereby declare that they have nothing to disclose.
Statement of Authorship
All authors are members of the OCCS Common Data Element Committee and have assisted in the identification and implementation of CDEs as well as in the review of this manuscript.






