Abstract
Purpose
In the last few years CBCT’s applications have expanded, especially in the field of musculoskeletal. In this study, we aim to analyze the diagnostic value and the use of CBCT in Emergency Radiology for the evaluation of extremity trauma.
Methods
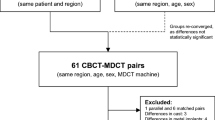
The present retrospective study included a total of 72 distal limb trauma cases who were admitted in the Emergency Radiology Department of “Policlinico Riuniti di Foggia” during September 2022 to December 2023. All the cases required further medical diagnostic investigation after an initial examination CR. Among these, 12 were excluded for suspected poly-traumas and MDCT was directly performed. Of the 60, divided into 2 groups, 42 had negative or non-diagnostic CR result, and CBCT was performed as second-level exam, 18 with a fracture confirmed by CR underwent CBCT for surgical planning.
Results
In the first group, 17 (40.5%) had negative CR results, and 25 (59.5%) had doubtful/non-diagnostic CR results. 25 (59.5%) presented a positive CBCT exam for fracture. In the second group, anyone required further diagnostic investigations for orthopedic surgery.
Conclusions
Thanks to high spatial resolution, low radiation dose, fast acquisition, and its three-dimensionality in space (3D), CBCT could be the first investigation in the cases of fractures clinically suspicious in locations with bone overlap.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Introduction
Cone beam computed tomography (CBCT), also known as digital volumetric tomography (DVT), was developed for imaging of the dento-maxillo-facial region in the late 1990s and the first CBCT equipment entering the European market in the early 2000s [1].
In recent years, CBCT is an increasingly used imaging modality [2] and it is currently installed in many radiology departments as an integral part of the imaging armamentarium [3].
Application of dedicated CBCT for musculoskeletal diagnostic is quite recent [4] and has recently been described and adopted for extremities imaging in orthopedics [5].
Technically, in CBCT systems, the X-ray beam forms a conical geometry between the source and the detector [6]. The field of view (FOV), representing the body area that is the object of study, is located among them.
Unlike MDCT, CBCT can produce volumetric images of the region of the interest with a single scan where the X-ray source and the detector simultaneously move around the patient [7]. More data can be acquired with a single rotation resulting lower radiation dose.
Depending upon manufacturers, the scanning time of CBCT equipment varies from nearly 5–40 s [8].
Hundreds of 2D images of a defined anatomical volume are acquired rather than the slice-by-slice imaging found in conventional CT [9].
Software programs incorporating sophisticated algorithms including back-filtered projection are applied to these image data to generate 3D volumetric data set, which can be used to provide primary reconstruction images in three orthogonal planes (axial, sagittal, and coronal) [10]. The images are reconstructed using the algorithm developed by Feldkamp et al. in 1994 [11] or its variation form [12].
In addition, CBCT volumetric data is isotropic, which means all three dimensions of the image voxels are the same, allowing to re-orient the images to fit the patient’s anatomic features and perform real-time measurements [13].
Overall, the CBCT is an imaging technique that uses an X-ray computed tomography and offers high spatial revolution, low radiation dose, and a relatively low cost of the equipment compared to MSCT [14].
The objective of this retrospective study is to investigate the diagnostic value and the use of CBCT in Emergency Radiology. The present state-of-the-art and the advantage of CBCT over MDCT and conventional X-ray are also discussed.
Materials and methods
The present retrospective study included a total of 72 patients who were admitted in the Emergency Radiology Department of “Policlinico Riuniti di Foggia” during September 2022 to December 2023.
Included patients had a history of distal limb trauma and high clinically suspected wrist, metacarpal, ankle, tarsal, metatarsal, phalangeal, knee, and elbow fractures.
Pregnant women and patients with pelvis, cervical, and shoulder suspected fractures were excluded.
Into the Emergency Radiology Department, all patients underwent an initial CR examination. Early radiographic investigation included a standard view series for district which contained at least two standards view, antero-posterior and lateral, in a neutral position. Additional different radiographic views were performed in ambiguous/non-diagnostic results selected cases and high clinical fracture suspicion.
After an initial examination CR, all 72 cases required further medical diagnostic investigation.
Among these, 12 patients were excluded for suspected poly-traumas and MDCT was directly performed. GE Revolution 256-slice scanner has been used.
The remaining 60 patients underwent CBCT were divided into two groups: the first group included 42 patients with high clinically suspected fracture and negative or doubtful/non-diagnostic radiographs; the second group included 18 patients with a fracture confirmed by CR who required further examination for surgical planning.
Figure 1 details the above-described data collection process.
All the CBCT images were obtained by the same unit (Siemens Multitom Rax). The acquisition time was 10–20 s in a 169°–200° rotation. For the interpretation, image reconstruction contained three planes in space (axial, sagittal, and coronal) relative to the axis of the examined district. No iodine contrast product was injected.
Informed patient consent was obtained before every CBCT examination.
Results
In the first group, 17 patients (40.5%) had negative CR results, instead 25 patients (59.5%) had doubtful/non-diagnostic radiographs, and CBCT was performed as second-level exam.
On the contrary 25 (59.5%), CBCT exams were positive for distal limb fractures.
In the subgroup of negative CR, CBCT revealed fractures in 9 cases and confirmed negative radiographs in 8 cases.
On average, in the first group, 2.6 standard views were performed for ankle traumas, 2.4 for wrist traumas, 2.3 for knee traumas, 2.7 for hand traumas, 3.3 for foot traumas, and 2.8 for elbow traumas. 2 standard views were performed in one forearm trauma case and 3 in one thigh trauma case.
In the second group, 18 patients underwent CBCT for surgical planning. 6 patients had elbow fracture, 3 hand fracture, 3 wrist fracture, 2 ankle fracture, 2 knee fracture, 1 foot fracture, and 1 humerus fracture.
None of the patients examined with CBCT required further diagnostic investigations for orthopedic surgery. In addition, in 7 cases of this group, CBCT revealed further fractures that were unrecognized on conventional X-ray, favoring a precise surgical planning.
Discussion
After its introduction in dento-maxillo-facial imaging in 1998 by Mozzo et al. [15], the last decade witnessed a proliferation of cone-beam CT (CBCT) imaging technologies [16].
More recently, devices devoted to musculoskeletal imaging, notably of the extremities, have appeared on the market and obtained authorization for clinical use from the American FDA (Food and Drug Administration) and the EU with CE labeling [17].
Trauma is the one of the most common reasons of admission to emergency department [18]. Grunz et al. [19] have demonstrated that CBCT provides an advantage for the evaluation of acute small bone trauma by detecting and excluding extremity fractures more than radiographs. In Grunz’s study, CBCT detected more fractures than radiography (accuracy 0.98 vs 0.71).
Using a CBCT scanner, it is possible to obtain traditional 2D images as well as 3D views from the same scan. The addition of 3D scanning helps us to overcome the issues of structure superimposition, which can make interpretation difficult when assessing 2D pictures. To mitigate this with plain films, multiple views are often required (e.g., “foot series” or “scaphoid series”) [20].
As discussed by Grassi et al. [21], the CBCT software allows bone segment view under examination in three interactive views, coronal, sagittal, and axial, and the plane of interest can be moved within each section, allowing the entire volume of information to be scanned in the three planes (Fig. 2).
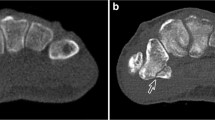
We evaluated the detection of fractures in distal limb trauma cases using conventional X-ray and CBCT. With CBCT, the presence of fracture was correctly diagnosed even when the CR examination was negative (Fig. 3).
CBCT also confirmed or excluded fractures suspected in radiography (Fig. 4).
50-year-old male patient presented to the emergency department with persistent left wrist pain following to a blunt trauma that occurred about a month earlier. The X-ray image showed probable fracture sequelae involving the radial styloid. CBCT examination confirmed a simple fracture of the radial styloid in reparative phase
CBCT has a higher diagnostic accuracy for scaphoid fracture than radiography [22]. MRI is the gold standard for detecting occult scaphoid fractures and it is a method recommended by the ACR [23].
Since MRI is costly and not always available in an emergency context, a CT scan is typically performed. The latter modality has a sensitivity of 91% and specificity of 98% for the diagnosis of scaphoid fractures. However, bone scanning is not an effective alternative in this context given its higher cost, long scan time, and higher level of radiation [4].
Nonetheless, it is not always possible to perform MRI immediately following trauma and MRI cannot be performed in every patient, due to potential contraindications or lesser accessibility. Therefore, CBCT should be considered as a second-line imaging modality in assessing complex anatomical sites with multiple overlapping bones, such as wrist and foot, in case of negative CR but with high clinical suspicion of a fracture (Fig. 5) [3].
3D imaging technique can reveal most of these fractures that remain invisible to conventional X-ray. For many years, MDCT was the imaging technique of choice, but a high dose of radiation is required.
Many studies present a significantly lower dose in CBCT protocols compared to MDCT protocols [24]. The data reported in the literature concerning the CBCT effective dose (ED) are about 12 times lower than the MDCT [5]. Moreover, collimation of the CBCT primary X-ray beam enables limitation of the X-radiation to the area of interest [25].
CBCT system generates a complete volumetric dataset with the patient stationary via a single rotation of the X-ray source and detector [5]. The rotation angle, during images acquisition, varied between 180° and 360° [26]. The selected FOV for CBCT images is directly related to voxel size and affects the resolution and contrast [27]. Consequently, it has a higher spatial resolution, corresponding to 80–130 microns compared to 500–700 microns of MDCT [21].
The greater spatial resolution allows the fine details’ evaluations, facilitating the precise diagnosis of occult fractures.
CBCT in emergency contexts could reduce misdiagnosed fractures. It is the most common diagnostic error, which may account for 41–80% of diagnostic error in emergency department [28] and may determine a delayed treatment and poor outcome for patients and leading to medical legal claims [29].
The main advantages of CBCT are summarized in Table 1.
CBCT is also indicated for the pre-operative planning of fractures (Fig. 6) as well as for the evaluation of the post-surgical treatment and the healing process, even in the presence of internal metal fixation systems. Metal artifacts are significantly reduced in CBCT compared to MDCT, thanks to artifact reduction algorithms, MAR (Metal Artifact Reduction) [21]. When the 3D techniques are performed, the features can lead the orthopedist to modify the pre-operative treatment based on radiographs [30].
Further applications of CBCT in musculoskeletal are shown in Table 2 [3].
Among the limitations of CBCT should be mentioned are: the relatively longer exposure time, which may increase the risk of motion artifacts [31], and it isn’t indicated for the soft tissue pathology due to reduction of contrast resolution [32].
In agreement with Jacques et al. [17], CBCT in emergency contexts accelerates turnover of trauma. It has easy access while MDCT is available for emergencies in other specialties, and it ease of patient positioning.
The main present study limitation is due to different radiologists who interpreted the initial CR examination. The results of a single-center retrospective study design are also influenced by local practices.
Conclusions
In emergency contexts, CBCT has demonstrated greater possibility of documenting intra-articular fractures, greater confidence in excluding doubtful fractures, and the possibility of precise surgical planning.
Use of CBCT, compared to MDCT, can accelerate with numerous advantages the diagnosis of fracture and, consequently, facilitate elective treatments.
In conclusion, thanks to high spatial resolution, low radiation dose, fast acquisition, and its three-dimensionality in space (3D), CBCT could be the first investigation in emergency radiology in the cases of fractures clinically suspicious in locations with bone overlap.
Data availability statement
The reported data come from the register of daily activities of Emergency Radiology Department of Policlinico Riuniti di Foggia.
References
Horner K, Jacobs R, Schulze R (2013) Dental CBCT equipment and performance issues. Radiat Prot Dosimetry 153(2):212–218. https://doi.org/10.1093/rpd/ncs289
Werbrouck C, Koen M, Casselman J (2021) New CBCT Indications in Musculoskeletal Imaging. J Belg Soc Radiol 105(1):69, 1–4. https://doi.org/10.5334/jbsr.2649
Posadzy M, Desimpel J, Vanhoenacker F (2018) Cone beam CT of the musculoskeletal system: clinical applications. Insights Imaging 9(1):35–45. https://doi.org/10.1007/s13244-017-0582-1
Borel C, Larbi A, Delclaux S, Lapegue F, Chiavassa-Gandois H, Sans N, Faruch-Bilfeld M (2017) Diagnostic value of cone beam computed tomography (CBCT) in occult scaphoid and wrist fractures. Eur J Radiol 97:59–64. https://doi.org/10.1016/j.ejrad.2017.10.010
Ricci PM, Boldini M, Bonfante E, Sambugaro E, Vecchini E, Schenal G, Magnan B, Montemezzi S (2019) Cone-beam computed tomography compared to X-ray in diagnosis of extremities bone fractures: a study of 198 cases. Eur J Radiol Open 13(6):119–121. https://doi.org/10.1016/j.ejro.2019.01.009. (Erratum in: Eur J Radiol Open. 2020;8:100308)
Miracle AC, Mukherji SK (2009) Conebeam CT of the head and neck, part 1: physical principles. AJNR Am J Neuroradiol 30(6):1088–1095. https://doi.org/10.3174/ajnr.A1653
Kumar M, Shanavas M, Sidappa A, Kiran M (2015) Cone beam computed tomography - know its secrets. J Int Oral Health 7(2):64–68
Venkatesh E, Elluru SV (2017) Cone beam computed tomography: basics and applications in dentistry. J Istanb Univ Fac Dent 51(3 Suppl 1):S102–S121. https://doi.org/10.17096/jiufd.00289
Alamri HM, Sadrameli M, Alshalhoob MA, Sadrameli M, Alshehri MA (2012) Applications of CBCT in dental practice: a review of the literature. Gen Dent 60(5):390–400 (quiz 401–402)
John GP, Joy TE, Mathew J, Kumar VR (2015) Fundamentals of cone beam computed tomography for a prosthodontist. J Indian Prosthodont Soc 15(1):8–13. https://doi.org/10.4103/0972-4052.157001
Feldkamp LA (1984) Practical cone-beam algorithm Sfrdr I _ f. America (NY) 1(6):612–619
Giacometti V, Hounsell AR, McGarry CK (2020) A review of dose calculation approaches with cone beam CT in photon and proton therapy. Phys Med 76:243–276. https://doi.org/10.1016/j.ejmp.2020.06.017
Adibi S, Zhang W, Servos T, O’Neill PN (2012) Cone beam computed tomography in dentistry: what dental educators and learners should know. J Dent Educ 76(11):1437–1442
Faccioli N, Santi E, Foti G, Mansueto G, Corain M (2022) Cost-effectiveness of introducing cone-beam computed tomography (CBCT) in the management of complex phalangeal fractures: economic simulation. Musculoskelet Surg 106(2):169–177. https://doi.org/10.1007/s12306-020-00687-3
Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IA (1998) A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol 8(9):1558–1564. https://doi.org/10.1007/s003300050586
Schafer S, Nithiananthan S, Mirota DJ, Uneri A, Stayman JW, Zbijewski W, Schmidgunst C, Kleinszig G, Khanna AJ, Siewerdsena JH (2011) Mobile C-arm cone-beam CT for guidance of spine surgery: image quality, radiation dose, and integration with interventional guidance. Med Phys 38(8):4563–4574. https://doi.org/10.1118/1.3597566
Jacques T, Morel V, Dartus J, Badr S, Demondion X, Cotten A (2021) Impact of introducing extremity cone-beam CT in an emergency radiology department: a population-based study. Orthop Traumatol Surg Res 107(2):102834. https://doi.org/10.1016/j.otsr.2021.102834
Püsküllüoğlu S et al (2015) Analysis of adult trauma patients admitted to emergency department. Cukurova Med J 40(3):569–577. https://doi.org/10.17826/cutf.68238
Grunz JP, Pennig L, Fieber T, Gietzen CH, Heidenreich JF, Huflage H, Gruschwitz P, Kuhl PJ, Petritsch B, Kosmala A, Bley TA, Gassenmaier T (2021) Twin robotic x-ray system in small bone and joint trauma: impact of cone-beam computed tomography on treatment decisions. Eur Radiol 31(6):3600–3609. https://doi.org/10.1007/s00330-020-07563-5
Bailey J, Solan M, Moore E (2022) Cone-beam computed tomography in orthopaedics. Orthopaed Trauma 36(4):194–201
Grassi R, Guerra E, Berritto D (2023) Bone fractures difficult to recognize in emergency: may be cone beam computed tomography (CBCT) the solution? Radiol Med 128(1):1–5. https://doi.org/10.1007/s11547-022-01584-4
Neubauer J, Benndorf M, Ehritt-Braun C, Reising K, Yilmaz T, Klein C, Zajonc H, Kotter E, Langer M, Goerke SM (2018) Comparison of the diagnostic accuracy of cone beam computed tomography and radiography for scaphoid fractures. Sci Rep 8(1):3906. https://doi.org/10.1038/s41598-018-22331-8
Edlund R, Skorpil M, Lapidus G, Bäcklund J (2016) Cone-beam CT in diagnosis of scaphoid fractures. Skelet Radiol 45(2):197–204. https://doi.org/10.1007/s00256-015-2290-6
Neubauer J, Neubauer C, Gerstmair A, Krauss T, Reising K, Zajonc H, Kotter E, Langer M, Fiebich M, Voigt J (2016) Comparison of the radiation dose from cone beam computed tomography and multidetector computed tomography in examinations of the hand. Rofo 188(5):488–493. https://doi.org/10.1055/s-0042-101251
Scarfe WC, Farman AG (2008) What is cone-beam CT and how does it work? Dent Clin N Am 52(4):707–30, v. https://doi.org/10.1016/j.cden.2008.05.005
Nemtoi A, Czink C, Haba D, Gahleitner A (2013) Cone beam CT: a current overview of devices. Dentomaxillofac Radiol 42(8):20120443. https://doi.org/10.1259/dmfr.20120443
Fakhar HB, Mallahi M, Panjnoush M, Kashani PM (2016) Effect of voxel size and object location in the field of view on detection of bone defects in cone beam computed tomography. J Dent (Tehran). 13(4):279–286
Pinto A, Reginelli A, Pinto F, Lo Re G, Midiri F, Muzj C, Romano L, Brunese L (2016) Errors in imaging patients in the emergency setting. Br J Radiol 89(1061):20150914. https://doi.org/10.1259/bjr.20150914
Pinto A, Berritto D, Russo A, Riccitiello F, Caruso M, Belfiore MP, Papapietro VR, Carotti M, Pinto F, Giovagnoni A, Romano L, Grassi R (2018) Traumatic fractures in adults: missed diagnosis on plain radiographs in the Emergency Department. Acta Biomed 89(1-S):111–123. https://doi.org/10.23750/abm.v89i1-S.7015
Macarini L, Murrone M, Marini S, Calbi R, Solarino M, Moretti B (2004) Tibial plateau fractures: evaluation with multidetector-CT. Radiol Med 108(5–6):503–514 (English, Italian)
Helal RA, Jacob R, Elshinnawy MA, Othman AI, Al-Dhamari IM, Paulus DW, Abdelaziz TT (2021) Cone-beam CT versus multidetector CT in postoperative cochlear implant imaging: evaluation of image quality and radiation dose. AJNR Am J Neuroradiol 42(2):362–367. https://doi.org/10.3174/ajnr.A6894
Han M, Kim HJ, Choi JW, Park DY, Han JG (2022) Diagnostic usefulness of cone-beam computed tomography versus multi-detector computed tomography for sinonasal structure evaluation. Laryngoscope Investig Otolaryngol 7(3):662–670. https://doi.org/10.1002/lio2.792
Acknowledgements
None.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Francesco Boccia: conception and design of the study; acquisition of data; analysis and interpretation of data; manuscript co-drafting. All authors contributed to the study conception and design, manuscript co-drafted and revised the article. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no conflict of interest.
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki. The Institutional Review Board is not applicable, considering the retrospective nature of the study.
Consent for publication
Informed patient consent was obtained before every cone-beam computed tomography examination.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lo Mastro, A., Boccia, F., Berritto, D. et al. Unrecognized bone fractures of the extremities in Emergency Radiology: the invisible become visible on 3D 80 micron. J Med Imaging Intervent Radiol 11, 6 (2024). https://doi.org/10.1007/s44326-024-00006-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44326-024-00006-1