Abstract
Objective
Our primary objective was to determine agreement between non-suicidal self-injury recorded at triage and during subsequent mental health assessment. The secondary objective was to describe patients who reported non-suicidal self-injury.
Methods
This is a health records review of patients aged 12–18 years who had an Emergency Mental Health Triage form on their health record from an ED visit June 1, 2017–May 31, 2018. We excluded patients with diagnoses of autism spectrum disorder or schizophrenia. We abstracted data from the Mental Health Triage form, Emergency Mental Health and Addictions Service Assessment forms and Assessment of Suicide and Risk Inventory. We calculated Cohen’s Kappa coefficient, sensitivity, and negative predictive value to describe the extent to which the forms agreed and the performance of triage for identifying non-suicidal self-injury. We compared the cohort who reported non-suicidal self-injury with those who did not, using t-tests, Wilcoxon rank-sum tests, and chi-square tests.
Results
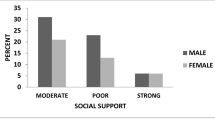
We screened 955 ED visits and included 914 ED visits where 558 (58.4%) reported a history of non-suicidal self-injury. There were significantly more females in the group reporting non-suicidal self-injury (82.1%, n = 458) compared to the group not reporting non-suicidal self-injury (45.8%, n = 163). Patients reporting non-suicidal self-injury did so in triage and detailed Mental Health Assessment 64.7% of the time (Cohen’s Kappa Coefficient 0.6); triage had sensitivity of 71.5% (95% CI 67.3–75.4) and negative predictive value of 71.2% (95% CI 68.2–74.0). Cutting was the most common method of non-suicidal self-injury (80.3%).
Conclusion
Screening at triage was moderately effective in identifying non-suicidal self-injury compared to a detailed assessment by a specialised mental health team. More than half of children and adolescents with a mental health-related concern in our ED reported a history of non-suicidal self-injury, most of which were female. This symptom is important for delineating patients’ coping strategies.
Résumé
Objectifs
Notre objectif principal était de déterminer l’accord entre les blessures non suicidaires enregistrées au triage et lors de l’évaluation subséquente de la santé mentale. L’objectif secondaire était de décrire les patients qui ont déclaré une automutilation non suicidaire.
Méthodes
Il s’agit d’un examen des dossiers de santé de patients âgés de 12 à 18 ans qui avaient un formulaire de triage d’urgence en santé mentale dans leur dossier de santé à la suite d’une visite à l’urgence du 1er juin 2017 au 31 mai 2018. Nous avons exclu les patients présentant un diagnostic de trouble du spectre autistique ou de schizophrénie. Nous avons extrait des données du formulaire de triage en santé mentale, des formulaires d’évaluation des services d’urgence en santé mentale et en toxicomanie et de l’évaluation du suicide et de l’inventaire des risques. Nous avons calculé le coefficient de Kappa de Cohen, la sensibilité et la valeur prédictive négative pour décrire la mesure dans laquelle les formes étaient d’accord et la performance du triage pour identifier l’automutilation non suicidaire. Nous avons comparé la cohorte qui a déclaré une automutilation non suicidaire avec celles qui ne l’ont pas fait, en utilisant des tests t-tests, des tests Wilcoxon rank-sum et des tests chi-carrés.
Résultats
Nous avons examiné 955 visites à l’urgence et inclus 914 visites à l’urgence où 558 (58,4 %) ont signalé des antécédents d’automutilation non suicidaire. Il y avait beaucoup plus de femmes dans le groupe déclarant une automutilation non suicidaire (82,1 %, n = 458) que dans le groupe ne déclarant pas une automutilation non suicidaire (45,8 %, n = 163). Les patients ayant déclaré une automutilation non suicidaire l’ont fait dans le cadre du triage et de l’évaluation détaillée de la santé mentale 64,7 % du temps (coefficient de Kappa de Cohen 0,6); le triage avait une sensibilité de 71,5 % (IC à 95 % 67,3–75,4) et une valeur prédictive négative de 71,2 % (IC à 95 % 68,2–74,0). La coupe était la méthode la plus courante d’automutilation non suicidaire (80,3 %).
Conclusion
Le dépistage au triage a été modérément efficace pour identifier les blessures non suicidaires comparativement à une évaluation détaillée par une équipe spécialisée en santé mentale. Plus de la moitié des enfants et des adolescents ayant un problème de santé mentale à notre DE ont signalé des antécédents d’automutilation non suicidaire, dont la plupart étaient des femmes. Ce symptôme est important pour délimiter les stratégies d’adaptation des patients.

Similar content being viewed by others
Data availability
The de-identified data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Muehlenkamp JJ, Gutierrez PM. An investigation of differences between self-injurious behavior and suicide attempts in a sample of adolescents. Suicide Life Threat Behav. 2004;34(1):12–23.
Whitlock J, Eckenrode J, Silverman D. Self-injurious behaviors in a college population. Pediatrics. 2006;117(6):1939–48.
Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat Behav. 2014;44(3):273–303.
Muehlenkamp JJ, Claes L, Havertape L, Plener PL. International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child Adolesc Psychiatry Ment Health. 2012;30(6):10.
Liu RT, Walsh RFL, Sheehan AE, Cheek SM, Sanzari CM. Prevalence and correlates of suicide and nonsuicidal self-injury in children: a systematic review and meta-analysis. JAMA Psychiat. 2022;79(7):718–26.
Wong BHC, Cross S, Zavaleta-Ramírez P, Bauda I, Hoffman P, Ibeziako P, et al. Self-harm in children and adolescents who presented at emergency units during the COVID-19 pandemic: an international retrospective cohort study. J Am Acad Child Adolesc Psychiatry. 2023;16:S0890-8567.
Sara G, Wu J, Uesi J, Jong N, Perkes I, Knight K, et al. Growth in emergency department self-harm or suicidal ideation presentations in young people: comparing trends before and since the COVID-19 first wave in New South Wales. Australia Aust N Z J Psychiatry. 2023;57(1):58–68.
Poonai N, Freedman SB, Newton AS, Sawyer S, Gaucher N, Ali S, et al. Emergency department visits and admissions for suicidal ideation and self-harm in Canadian adolescents during the COVID-19 pandemic. CMAJ. 2023;195(36):E1221–30. https://doi.org/10.1503/cmaj.220507.
Klonsky ED, Victor SE, Saffer BY. Nonsuicidal self-injury: What we know, and what we need to know. Can J Psychiatry Rev Can Psychiatr. 2014;59(11):565–8.
Say DF, Carison A, Hill A, Hiscock H, Babl FE, O’Donnell SM. Mental health presentations to the paediatric emergency department: a retrospective study. J Paediatr Child Health. 2021;57(5):684–95.
Qian J, Wong Q, Burnett A, McGillivray L, Han J, Larsen M, et al. Risk of repeat self-harm and suicide death following an episode of hospital self-harm presentation among adolescents and young adults. J Affect Disord. 2023;15(321):191–200.
Bethell J, Bondy SJ, Lou WYW, Guttmann A, Rhodes AE. Emergency department presentations for self-harm among Ontario youth. Can J Public Health Rev Can Sante Pub. 2013;104(2):e124-130.
Goldman-Mellor SJ, Bhat HS, Allen MH, Schoenbaum M. Suicide risk among hospitalized versus discharged deliberate self-harm patients: generalized random forest analysis using a large claims data set. Am J Prev Med. 2022;62(4):558–66.
Black T. Assessment of Suicide and Risk Inventory [Internet]. 2013 [cited 2023 Aug 3]. Available from: http://www.asari.ca/ASARI-general.pdf
Nixon MK, Cloutier PF, Aggarwal S. Affect regulation and addictive aspects of repetitive self-injury in hospitalized adolescents. J Am Acad Child Adolesc Psychiatry. 2002;41(11):1333–41.
Howowritz LM, Bridge JA, Teach SJ. Ask suicide-screening questions (ASQ) a brief instrument for the pediatric emergency department. Arch Pediatr Adolesc Med. 2012;166(12):1170–6.
Lee A, Deevska M, Stillwell K, Black T, Meckler G, Park D, Eslami A, Doan Q. A psychosocial assessment and management tool for children and youth in crisis. CJEM. 2019;21(1):87–96.
American Psychiatric Association. Conditions for Further Study. In: Diagnostic and statistical manual of mental disorders (5th ed, text rev) [Internet]. [cited 2023 Aug 14]. Available from: https://dsm.psychiatryonline.org/doi/full/https://doi.org/10.5555/appi.books.9780890425787.Conditions_for_Further_Study#x30791.2818342
Acknowledgements
We would like to acknowledge research assistants Natalie William and Kathleen Kennedy who reviewed patient records and entered data for this study.
Funding
This work was funded by the Public Health Agency of Canada through the Canadian Hospitals Injury Reporting and Prevention Program (CHIRPP).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or non-financial conflicts of interest to report.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cherry, J.C., Fitzpatrick, E.A., Sandila, N.K. et al. Non-suicidal self-injury at a Canadian paediatric emergency department. Can J Emerg Med 26, 259–265 (2024). https://doi.org/10.1007/s43678-024-00657-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-024-00657-9