Abstract
Objective
Mandatory gunshot wound reporting laws have been enacted in much of Canada, yet there is a lack of evidence on whether these laws are effective in preventing firearm injuries. Our objective was to determine if the Gunshot Wounds Reporting Act in Nova Scotia had an effect on the number of firearm-related injuries in the province.
Methods
Pre–post-study of major trauma patients in Nova Scotia who sustained a gunshot wound injury before and after enactment of the Gunshot Wounds Reporting Act (Bill 10) in 2008. Data were collected from the Nova Scotia Trauma Registry and the Nova Scotia Medical Examiner Service for a 6-year pre-period (2002–2007) and an 11-year post-period (2009–2019), allowing for a 1-year washout period. Patient characteristics in the pre- and post-periods were compared using t tests and Chi-square analysis. Gunshot wound traumas were analyzed as a time series using the AutoRegressive Integrated Moving Average (ARIMA) model.
Results
A total of 722 firearm injuries were observed during the study period (pre-period = 259, post-period = 463). Mean age was 45.2 ± 19.3 years with males accounting for 95.3% (688/722) of cases. The majority of injuries were self-inflicted (65.1%; 470/722). The mean overall annualized rate of firearm injuries was 4.61 per 100,000 population in the pre-period and 4.45 per 100,000 in the post-period (reduction of 3.4%). No linear trends in the annual number of firearm injuries were observed over the study period. ARIMA modelling was an extremely poor predictor for gunshot wound trauma (R2 = 0.012).
Conclusions
Although our findings suggest that there is no association between the Gunshot Wounds Reporting Act and the incidence of firearm injury, it is difficult to draw firm conclusions due to the complexity of this topic. Physicians need to be aware of the legal requirements of mandatory reporting when they encounter patients with gunshot wounds.
Résumé
Objectif
Des lois obligatoires sur le signalement des blessures par balle ont été promulguées dans une grande partie du Canada, mais on manque de données probantes sur l'efficacité de ces lois pour prévenir les blessures par balle. Notre objectif était de déterminer si la Gunshot Wounds Reporting Act de la Nouvelle-Écosse a eu un effet sur le nombre de blessures liées aux armes à feu dans la province.
Méthodes
Étude pré-post des patients souffrant de traumatismes majeurs en Nouvelle-Écosse et ayant subi une blessure par balle avant et après la promulgation de la loi sur la déclaration des blessures par balle (projet de loi 10) en 2008. Les données ont été recueillies auprès du Nova Scotia Trauma Registry et du Nova Scotia Medical Examiner Service pour une période de 6 ans avant (2002–2007) et de 11 ans après (2009–2019), en tenant compte d'une période d'élimination d'un an. Les caractéristiques des patients avant et après les périodes ont été comparées à l’aide de tests- t et d’une analyse du chi-carré. Les traumatismes liés aux blessures par balle ont été analysés comme une série chronologique à l'aide du modèle ARIMA (AutoRegressive Integrated Moving Average).
Résultats
Au total, 722 blessures par arme à feu ont été observées au cours de la période d'étude (avant la période = 259, après la période = 463). L'âge moyen était de 45,2 ± 19,3 ans, les hommes représentant 95,3% (688/722) des cas. La majorité des blessures étaient auto-infligées (65,1%; 470/722). Le taux global moyen annualisé de blessures par arme à feu était de 4,61 pour 100 000 habitants pendant la période antérieure et de 4,45 pour 100 000 pendant la période postérieure (réduction de 3,4%). Aucune tendance linéaire du nombre annuel de blessures par arme à feu n'a été observée au cours de la période d'étude. Le modèle ARIMA s'est avéré être un très mauvais prédicteur des traumatismes liés aux blessures par balle (R2 = 0,012).
Conclusions
Bien que nos résultats suggèrent qu'il n'y a pas de lien entre la loi sur le signalement des blessures par balle et l'incidence des blessures par arme à feu, il est difficile de tirer des conclusions définitives en raison de la complexité de ce sujet. Les médecins doivent être conscients des obligations légales de déclaration obligatoire lorsqu'ils rencontrent des patients présentant des blessures par balle.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
What is known about the topic? |
The effect of mandatory gunshot wound reporting laws on firearm injuries has not been studied to date. |
What did this study ask? |
Did the incidence of firearm-related injuries in Nova Scotia change following enactment of the 2008 Gunshot Wounds Reporting Act? |
What did this study find? |
There was no association between the Gunshot Wounds Reporting Act and the number of firearm injuries in the province. |
Why does this study matter to clinicians? |
Physicians need to be aware of the legal requirements of mandatory reporting when they encounter patients with gunshot wounds. |
Introduction
Over the last 50 years, Canadian governments have implemented various laws to prevent firearm-related injury and death. Although these legislative initiatives have largely focused on strengthening regulations governing the sale, purchase, storage, and transportation of firearms, most provinces and territories in Canada have also implemented laws requiring health care facilities to report gunshot wounds to local law enforcement [1]. Mandatory gunshot wound reporting laws have elicited much debate over whether they improve public safety and injury prevention, and if so, whether that improvement is worth the breach in patient-physician confidentiality [1, 2]. There are concerns such laws will deter gunshot wound patients from seeking medical attention and that those who do present may be induced to provide inaccurate information [2]. Proponents, including the Canadian Association of Emergency Physicians, argue that these laws are an important part of a multifaceted approach towards preventing firearm-related injuries and deaths [3]. To date, no studies have investigated the effect of mandatory gunshot wound reporting laws on firearm-injury rates.
In some provinces, the intent of these laws is to help combat crime by facilitating investigation of stabbings or shootings soon after the incident; Nova Scotia is one such example, having enacted the Gunshot Wound Reporting Act (Bill 10) in 2008 [4, 5]. Following the 2020 mass shooting in Nova Scotia which pushed the annual number of homicides in Canada to its highest level in nearly 30 years, we sought to gain a better understanding of the burden of gunshot wound injury. The objective of this study was to determine if the Gunshot Wound Reporting Act had an effect on the number of firearm-related major traumas seen in the province.
Methods
Study design and setting
A pre–post-study of major trauma patients in Nova Scotia with firearm-related injuries before and after enactment of the Gunshot Wounds Reporting Act. This study was performed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for reporting observational studies. Ethical approval was obtained from the Nova Scotia Health Research Ethics Board (File #1025951).
Study population
Included were all major trauma patients with a firearm-related injury (based on ICD-10-CA coding) during a 6-year pre-legislation period (January 1 2002—December 31 2007) and an 11-year post-legislation period (January 1 2009—December 31 2019), allowing for a 1-year washout period in 2008. Any deaths at the scene or during transport were included.
Data collection and outcome measurements
Data was collected from the Nova Scotia Trauma Registry (NSTR), a provincial population-based registry under the Nova Scotia Department of Health and Wellness. The NSTR contains data on all major trauma patients with an Injury Severity Score (ISS) ≥ 12 and an appropriate ICD-10-CA code, as well as all penetrating traumas with an ISS ≥ 9, all trauma team activations regardless of ISS, and traumas resulting in death prior to hospital arrival or in the emergency department (ED). As data on homicides may be not captured in the NSTR for legal reasons, we also collected homicide data from the Nova Scotia Medical Examiner Service. Data were collected on patient demographics (age, sex, and postal code), injury characteristics (mechanism, intentionality), injury severity (ISS and Glasgow Coma Scale at scene and on ED arrival), intubation (at scene or in ED), trauma team activation, and mortality.
Statistical analysis
Descriptive statistics including means, standard deviations, medians, interquartile ranges, and proportions were used to characterize the study population. Patient characteristics were compared between the pre- and post-periods using t tests and Chi-square analysis as appropriate. Injury rates were calculated based on 100,000 population (all ages) using population estimates from Statistics Canada. Data on gunshot wound traumas were analyzed as a time series for the period using the AutoRegressive Integrated Moving Average (ARIMA) model. All analyses were performed using SPSS software (version 26; IBM, Chicago).
Results
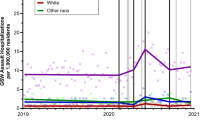
Overall, 722 firearm injuries occurred during the study period (pre-period n = 259; post-period n = 463). Figure 1 shows the overall firearm-injury rates per 100,000 population during the pre- and post-periods, as well as rates of assault/homicide and intentional self-harm. No linear trends in injury rates were observed during the study period. The mean overall rate of firearm injury during the pre-period was 4.61 per 100,000 population per year, which decreased by 3.4% to 4.45 in the post-period. The annual assault rate increased by 19.9% from the pre-period (1.14 per 100,000 per year) to the post-period (1.36 per 100,000 per year), while firearm injuries due to intentional self-harm decreased by 11.6% from the pre-period (3.13 per 100,000 per year) to the post-period (2.77 per 100,000 per year).
Mortality was 72.6% (524/722) and the majority of deaths occurred in the prehospital setting (65.4%, 472/722). Mortality rates were similar in the pre- and post-periods. Characteristics of trauma patients in the pre- and post-periods are compared in Online Resource 1. Age, sex, injury severity, and the intent of injury (self-inflicted, homicide/assault, and unintentional/undetermined) were similar in both periods. Patients injured during the post-period were more likely to be urban residents and to require activation of the trauma team. Time series analysis showed that gunshot wound traumas were predicted poorly by the ARIMA model (R2 = 0.012).
Discussion
Interpretation of findings
Our findings suggest the 2008 Gunshot Wounds Reporting Act had no effect on the number of firearm-related major traumas in Nova Scotia; however, it is difficult to draw firm conclusions based on the data available for this study. Although Bill 10 was not intended to prevent firearm injuries, this study is a step towards improving our understanding of the burden of gunshot wound trauma and serves to highlight the responsibility of physicians in advocating for comprehensive and transparent public health and safety measures to prevent firearm-related injuries.
Comparison to previous studies
Numerous studies have investigated the association between firearm legislation and firearm-related injuries with some finding evidence of a reduction in deaths, especially in countries which simultaneously implemented laws targeting multiple elements of firearms regulations; however, none of these studies examined the effect of mandatory gunshot wound reporting laws on firearm injury [6]. The first mandatory gunshot wound reporting law in Canada was enacted in Ontario in 2005. Ovens and colleagues surveyed emergency physicians, police, and the public in Ontario regarding the Mandatory Gunshot Wounds Reporting Act (Bill 110) [7]. Only 4% of emergency physicians who saw a gunshot wound reported to police felt the law negatively impacted the patient–physician relationship, and 3% had encountered a gunshot wound patient who deferred medical attention from fear of being reported. Furthermore, there was strong public support with 95% of respondents agreeing with the law, and 100% of police felt that the law was helpful in investigating shootings.
We observed most firearm injuries in Nova Scotia were self-inflicted, similar to findings from Ontario where self-harm accounted for 68% of all firearm deaths [8]. Data from the United States show that sales of firearms surged after the start of the COVID-19 pandemic and that gun violence rose by 31% during the first year of the pandemic compared to the previous year [9]. There is some evidence that gun violence has also risen in Canada during the pandemic. Data from Alberta show the overall number of severe injuries due to intentional violence remained stable during the first 3 months of the COVID-19 pandemic; however, there was a dramatic decrease in blunt assaults and a significant increase in penetrating trauma from gunshot wounds [10].
Strengths and limitations
Our findings should be interpreted with caution. First and foremost, gunshot wound epidemiology is a complex topic that is influenced by numerous systemic factors other than legislation. We were unable to account for potential confounding variables such as unemployment rates, divorce rates, and other societal factors. Importantly, there were no data available on the actual number of gunshot wound patients reported to police during the study period or whether enactment of Bill 10 and any negative effects on patient-physician relations. While the NSTR has quality control procedures to ensure accurate and complete data entry, some patients were missing data. Finally, our findings are based on the population of Nova Scotia and may not be generalizable to other provinces.
Research implications
Further studies should evaluate the effect of mandatory gunshot wound reporting on firearm-injury rates in other provinces and territories, and whether such laws negatively affect the patient–physician relationship. Outcomes, including the number of reports made, charges laid, and guns confiscated, should be examined to establish how reports are being used by police and whether they aid in preventing firearm injuries. Sharing this information between police and researchers would help inform quality improvement, epidemiological, and policy initiatives.
Clinical implications
Physicians in Canada should be aware of the legal requirements of mandatory reporting when they encounter a gunshot wound victim, as requirements vary by province and institution. In addition, physicians should be aware that the benefits and harms of mandatory reporting have not been adequately determined with respect to patients, health care workers, and society in general.
Conclusion
In this pre–post-study, we found no association between the 2008 Gunshot Wounds Reporting Act and the number of firearm-related injuries in Nova Scotia. Physicians should be aware of the legal requirements of mandatory reporting when they encounter a gunshot wound victim.
Availability of data and materials
Study data are not available.
Code availability
Not applicable.
References
Martin AF. The adoption of mandatory gunshot wound reporting legislation in Canada: a decade of tension in lawmaking at the intersection of law enforcement and public health. McGill JL Health. 2015;9:173.
Mackay B. Gunshot wounds: the new public health issue. CMAJ. 2004;170(5):780.
Snider CE, Ovens H, Drummond A, Kapur AK. CAEP position statement on gun control. CJEM. 2009;11(1):64–72.
Nova Scotia Legislature. Gunshot and stab wounds mandatory reporting act - Bill 10. 2007. https://nslegislature.ca/legislative-business/bills-statutes/bills/assembly-60-session-2/bill-10. Accessed 27 Dec 2021.
Acharya N. Provinces propose mandatory reporting laws. 2007. https://www.constitutionalstudies.ca/2007/12/provinces-propose-mandatory-reporting-laws/. Accessed 27 Dec 2021.
Santaella-Tenorio J, Cerdá M, Villaveces A, Galea S. What do we know about the association between firearm legislation and firearm-related injuries? Epidemiol Rev. 2016;38(1):140–57.
Ovens H, Park H, Borgundvaag B. Reaction in Ontario to Bill 110: Canada’s first mandatory gunshot wound reporting law. CJEM. 2009;11(1):3–13.
Gomez D, Saunders N, Greene B, Santiago R, Ahmed N, Baxter NN. Firearm-related injuries and deaths in Ontario, Canada, 2002–2016: a population-based study. CMAJ. 2020;192(42):E1253–63.
Ssentongo P, Fronterre C, Ssentongo AE, Advani S, Heilbrunn ES, Hazelton JP, et al. Gun violence incidence during the COVID-19 pandemic is higher than before the pandemic in the United States. Sci Rep. 2021;11:20654.
Ball CG. The Canadian-specific impact of COVID-19 on severe injuries from intentional violence, unintentional trauma and suicide-related causes. Can J Surg. 2021;64(2):E228–9.
Acknowledgements
The authors thank Karen Ssebazza (Nova Scotia Trauma Registry Coordinator) and Sherry Courtemanche (Nova Scotia Medical Examiner Service Case Records Manager) for assisting with data collection. We also thank Dr. Matthew Bowes (Nova Scotia Chief Medical Officer) for facilitating data collection from the Nova Scotia Medical Examiner Service. Data used in this research were made available by the Nova Scotia Department of Health and Wellness and the Nova Scotia Medical Examiner Service. Any opinions expressed by the authors do not necessarily reflect the opinion of the Nova Scotia Department of Health and Wellness, the Nova Scotia Health Trauma Program, or the Nova Scotia Medical Examiner Service.
Funding
This research was funded by a research studentship from Dalhousie University Faculty of Medicine.
Author information
Authors and Affiliations
Consortia
Contributions
This study was conceived and designed by RSG, NB, MK, and ME Data acquisition was performed by ME. Data analysis was performed by ME and NK. All authors contributed to interpretation of the results. The manuscript was drafted by NB and ME. All authors were involved in critically reviewing the manuscript, provided final approval of the version submitted for publication, and have agreed to be accountable for all aspects of the work presented in the manuscript
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical approval
Ethics approval was obtained from the Nova Scotia Health Research Ethics Board (File #1025951).
Consent to participate
Waiver of consent was granted by the Nova Scotia Health Research Ethics Board.
Consent for publication
Waiver of consent was granted by the Nova Scotia Health Research Ethics Board.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bennett, N., Erdogan, M., Karkada, M. et al. Mandatory gunshot wound reporting in Nova Scotia: a pre–post-evaluation of firearm-related injury rates. Can J Emerg Med 24, 439–443 (2022). https://doi.org/10.1007/s43678-022-00288-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-022-00288-y