Abstract
Background
Ursodeoxycholic acid (UDCA) is a secondary hydrophilic bile acid, metabolised in the gut, by microbiota. UDCA is currently prescribed for primary biliary cirrhosis, and of recently has shown β-cell protective effects, which suggests potential antidiabetic effects. Thus, this study aimed to design targeted-delivery microcapsules for oral uptake of UDCA and test its effects in type 1 diabetes (T1D).
Methods
UDCA microcapsules were produced using alginate-NM30 matrix. Three equal groups of mice (6–7 mice per group) were gavaged daily UDCA powder, empty microcapsules and UDCA microcapsules for 7 days, then T1D was induced by alloxan injection and treatments continued until mice had to be euthanised due to weight loss > 10% or severe symptoms develop. Plasma, tissues, and faeces were collected and analysed for bile acids’ concentrations.
Results
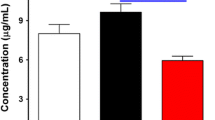
UDCA microcapsules brought about reduction in elevated blood glucose, reduced inflammation and altered concentrations of the primary bile acid chenodeoxycholic acid and the secondary bile acid lithocholic acid, without affecting survival rate of mice.
Conclusion
The findings suggest that UDCA exerted direct protective effects on pancreatic β-cells and this is likely to be associated with alterations of concentrations of primary and secondary bile acids in plasma and tissues.
Graphic abstract
Three equal groups of mice were gavaged daily UDCA (ursodeoxycholic acid) powder, empty microcapsules and UDCA microcapsules for 7 days, then T1D was induced and treatments continued until mice had to be euthanised. UDCA microcapsules brought about reduction in elevated blood glucose, reduced inflammation and altered concentrations of the primary bile acid chenodeoxycholic acid and the secondary bile acid lithocholic acid, without affecting survival rate of mice. The findings suggest that UDCA exerted direct protective effects on pancreatic β-cells and this is likely to be associated with alterations of concentrations of primary and secondary bile acids in plasma and tissues.






Similar content being viewed by others
Abbreviations
- BAs:
-
Bile acids
- CYP7A1:
-
Cholesterol-7-alphahydroxylase
- FXR:
-
Farnesoid X receptor
- T1D:
-
Type 1 diabetes
- UDCA:
-
Ursodeoxycholic acid
References
Conlon JM. Evolution of the insulin molecule: insights into structure-activity and phylogenetic relationships. Peptides. 2001;22(7):1183–93 (PMID:11569401).
O’Neill SM, Kenny LC, Khashan AS, West HM, Smyth RM, Kearney PM. Different insulin types and regimens for pregnant women with pre-existing diabetes. Cochrane Database Syst Rev. 2017;2:CD011880. https://doi.org/10.1002/14651858.cd011880.pub2.
Vahatalo MA, Viikari J, Ronnemaa T. Starting bedtime glargine versus NPH insulin in poorly controlled type 2 diabetic patients with various hyperglycemia types (fasting type or postprandial type). Acta Diabetol. 2014;51(2):233–8. https://doi.org/10.1007/s00592-013-0505-7.
Law GR, Bodansky HJ, McKinney PA. When do environmental factors initiate islet cell damage in children with Type 1 diabetes mellitus? Diabet Med. 2000;17(2):167–8 (PMID:11569401).
Thomas HE, Kay TW. How beta cells die in type 1 diabetes. Curr Dir Autoimmun. 2001;4:144–70 (PMID:11569401).
Genuth S. Insights from the diabetes control and complications trial/epidemiology of diabetes interventions and complications study on the use of intensive glycemic treatment to reduce the risk of complications of type 1 diabetes. Endocr Pract. 2006;12(Suppl 1):34–41. https://doi.org/10.4158/EP.12.S1.34.
Li T, Francl JM, Boehme S, Ochoa A, Zhang Y, Klaassen CD, et al. Glucose and insulin induction of bile acid synthesis: mechanisms and implication in diabetes and obesity. J Biol Chem. 2012;287(3):1861–73. https://doi.org/10.1074/jbc.M111.305789.
Vettorazzi JF, Ribeiro RA, Borck PC, Branco RC, Soriano S, Merino B, et al. The bile acid TUDCA increases glucose-induced insulin secretion via the cAMP/PKA pathway in pancreatic beta cells. Metabolism. 2016;65(3):54–63. https://doi.org/10.1016/j.metabol.2015.10.021.
Thomsen OO, Larsen JA. Interaction of insulin, glucagon, and DBcAMP on bile acid-independent bile production in the rat. Scand J Gastroenterol. 1982;17(5):687–93 (PMID:6294819).
Twisk J, Hoekman MF, Lehmann EM, Meijer P, Mager WH, Princen HM. Insulin suppresses bile acid synthesis in cultured rat hepatocytes by down-regulation of cholesterol 7 alpha-hydroxylase and sterol 27-hydroxylase gene transcription. Hepatology. 1995;21(2):501–10 (PMID:7843724).
Renga B, Mencarelli A, Vavassori P, Brancaleone V, Fiorucci S. The bile acid sensor FXR regulates insulin transcription and secretion. Biochem Biophys Acta. 2010;1802(3):363–72. https://doi.org/10.1016/j.bbadis.2010.01.002.
Mikov M, Boni NS, Al-Salami H, Kuhajda K, Kevresan S, Golocorbin-Kon S, et al. Bioavailability and hypoglycemic activity of the semisynthetic bile acid salt, sodium 3alpha,7alpha-dihydroxy-12-oxo-5beta-cholanate, in healthy and diabetic rats. Eur J Drug Metab Pharmacokinet. 2007;32(1):7–12 (PMID:17479538).
Mathavan S, Chen-Tan N, Arfuso F, Al-Salami H. A comprehensive study of novel microcapsules incorporating gliclazide and a permeation enhancing bile acid: hypoglycemic effect in an animal model of Type-1 diabetes. Drug Deliv. 2016;23(8):2869–80. https://doi.org/10.3109/10717544.2015.1110846.
Al-Salami H, Mamo JC, Mooranian A, Negrulj R, Lam V, Elahy M, et al. Long-term supplementation of microencapsulated ursodeoxycholic acid prevents hypertension in a mouse model of insulin resistance. Exper Clin Endocrinol Diabetes. 2017;125(1):28–32. https://doi.org/10.1055/s-0042-106084.
Mooranian A, Negrulj R, Al-Salami H. The influence of stabilized deconjugated ursodeoxycholic acid on polymer-hydrogel system of transplantable NIT-1 cells. Pharm Res. 2016;33(5):1182–90. https://doi.org/10.1007/s11095-016-1863-y.
Mooranian A, Takechi R, Jamieson E, Morahan G, Al-Salami H. The effect of molecular weights of microencapsulating polymers on viability of mouse-cloned pancreatic beta-cells: biomaterials, osmotic forces and potential applications in diabetes treatment. Pharm Dev Technol. 2018;23(2):145–50. https://doi.org/10.1080/10837450.2017.1321664.
Mooranian A, Negrulj R, Takechi R, Mamo J, Al-Sallami H, Al-Salami H. The biological effects of the hypolipidaemic drug probucol microcapsules fed daily for 4 weeks, to an insulin-resistant mouse model: potential hypoglycaemic and anti-inflammatory effects. Drug Deliv Transl Res. 2018;8(3):543–51. https://doi.org/10.1007/s13346-017-0473-5.
Mooranian A, Negrulj R, Takechi R, Jamieson E, Morahan G, Al-Salami H. Electrokinetic potential-stabilization by bile acid-microencapsulating formulation of pancreatic beta-cells cultured in high ratio poly-l-ornithine-gel hydrogel colloidal dispersion: applications in cell-biomaterials, tissue engineering and biotechnological applications. Artif Cells Nanomed Biotechnol. 2018;46(6):1156–62. https://doi.org/10.1080/21691401.2017.1362416.
Takechi R, Lam V, Brook E, Giles C, Fimognari N, Mooranian A, et al. Blood-brain barrier dysfunction precedes cognitive decline and neurodegeneration in diabetic insulin resistant mouse model: an implication for causal link. Fronti Aging Neurosci. 2017;9:399. https://doi.org/10.3389/fnagi.2017.00399.
Mooranian A, Tackechi R, Jamieson E, Morahan G, Al-Salami H. Innovative microcapsules for pancreatic beta-cells harvested from mature double-transgenic mice: cell imaging, viability, induced glucose-stimulated insulin measurements and proinflammatory cytokines analysis. Pharm Res. 2017;34(6):1217–23. https://doi.org/10.1007/s11095-017-2138-y.
Mooranian A, Negrulj R, Takechi R, Jamieson E, Morahan G, Al-Salami H. Influence of biotechnological processes, speed of formulation flow and cellular concurrent stream-integration on insulin production from β-cells as a result of co-encapsulation with a highly lipophilic bile acid. Cell Mol Bioeng. 2017. https://doi.org/10.1007/s12195-017-0510-y.
Mooranian A, Negrulj R, Takechi R, Jamieson E, Morahan G, Al-Salami H. Alginate-combined cholic acid increased insulin secretion of microencapsulated mouse cloned pancreatic beta cells. Ther Deliv. 2017;8(10):833–42. https://doi.org/10.4155/tde-2017-0042.
Mooranian A, Negrulj R, Takechi R, Jamieson E, Morahan G, Al-Salami H. New biotechnological microencapsulating methodology utilizing individualized gradient-screened jet laminar flow techniques for pancreatic beta-cell delivery: bile acids support cell energy-generating mechanisms. Mol Pharm. 2017. https://doi.org/10.1021/acs.molpharmaceut.7b00220.
Mooranian A, Negrulj R, Mathavan S, Martinez J, Sciarretta J, Chen-Tan N, et al. An advanced microencapsulated system: a platform for optimized oral delivery of antidiabetic drug-bile acid formulations. Pharm Dev Technol. 2015;20(6):702–9. https://doi.org/10.3109/10837450.2014.915570.
Mooranian A, Negrulj R, Arfuso F, Al-Salami H. The effect of a tertiary bile acid, taurocholic acid, on the morphology and physical characteristics of microencapsulated probucol: potential applications in diabetes: a characterization study. Drug Deliv Transl Res. 2015;5(5):511–22. https://doi.org/10.1007/s13346-015-0248-9.
Mooranian A, Negrulj R, Al-Sallami HS, Fang Z, Mikov M, Golocorbin-Kon S, et al. Probucol release from novel multicompartmental microcapsules for the oral targeted delivery in type 2 diabetes. AAPS PharmSciTech. 2015;16(1):45–52 (PMCID:PMC4309805).
Mooranian A, Negrulj R, Al-Sallami HS, Fang Z, Mikov M, Golocorbin-Kon S, et al. Release and swelling studies of an innovative antidiabetic-bile acid microencapsulated formulation, as a novel targeted therapy for diabetes treatment. J Microencapsul. 2015;32(2):151–6. https://doi.org/10.3109/02652048.2014.958204.
Mooranian A, Negrulj R, Mathavan S, Martinez J, Sciarretta J, Chen-Tan N, et al. Stability and release kinetics of an advanced gliclazide-cholic acid formulation: the use of artificial-cell microencapsulation in slow release targeted oral delivery of antidiabetics. J Pharm Innov. 2014. https://doi.org/10.1007/s12247-014-9182-5.
Mooranian A, Negrulj R, Chen-Tan N, Watts GF, Arfuso F, Al-Salami H. An optimized probucol microencapsulated formulation integrating a secondary bile acid (deoxycholic acid) as a permeation enhancer. Drug Des Devel Ther. 2014;8:1673–83. https://doi.org/10.2147/DDDT.S68247.
Mooranian A, Negrulj R, Chen-Tan N, Al-Sallami HS, Fang Z, Mukkur TK, et al. Microencapsulation as a novel delivery method for the potential antidiabetic drug, Probucol. Drug Des Devel Ther. 2014;8:1221–30. https://doi.org/10.2147/DDDT.S67349.
Mooranian A, Negrulj R, Chen-Tan N, Al-Sallami HS, Fang Z, Mukkur T, et al. Novel artificial cell microencapsulation of a complex gliclazide-deoxycholic bile acid formulation: a characterization study. Drug Des Dev Ther. 2014;8:1003–12. https://doi.org/10.2147/DDDT.S65396.
Fakhoury M, Negrulj R, Mooranian A, Al-Salami H. Inflammatory bowel disease: clinical aspects and treatments. J Inflamm Res. 2014;7:113–20. https://doi.org/10.2147/JIR.S65979.
Negrulj R, Mooranian A, Al-Salami H. Potentials and limitations of bile acids in type 2 diabetes mellitus: applications of microencapsulation as a novel oral delivery system. J Endocrinol Diabetes Mellit. 2013;1(2):49–59. https://doi.org/10.12970/2310-9971.2013.01.02.4.
Mooranian A, Negrulj R, Chen-Tan N, Fakhoury M, Arfuso F, Jones F, et al. Advanced bile acid-based multi-compartmental microencapsulated pancreatic beta-cells integrating a polyelectrolyte-bile acid formulation, for diabetes treatment. Artif Cells Nanomed Biotechnol. 2016;44(2):588–95. https://doi.org/10.3109/21691401.2014.971806.
Mooranian A, Negrulj R, Arfuso F, Al-Salami H. Characterization of a novel bile acid-based delivery platform for microencapsulated pancreatic beta-cells. Artif Cells Nanomed Biotechnol. 2016;44(1):194–200. https://doi.org/10.3109/21691401.2014.934457.
Mooranian A, Negrulj R, Arfuso F, Al-Salami H. Multicompartmental, multilayered probucol microcapsules for diabetes mellitus: formulation characterization and effects on production of insulin and inflammation in a pancreatic beta-cell line. Artif Cells Nanomed Biotechnol. 2016;44(7):1642–53. https://doi.org/10.3109/21691401.2015.1069299.
Mooranian A, Negrulj R, Al-Salami H, Morahan G, Jamieson E. Designing anti-diabetic beta-cells microcapsules using polystyrenic sulfonate, polyallylamine, and a tertiary bile acid: morphology, bioenergetics, and cytokine analysis. Biotechnol Prog. 2016;32(2):501–9. https://doi.org/10.1002/btpr.2223.
Mooranian A, Negrulj R, Al-Salami H. Alginate-deoxycholic Acid Interaction and its impact on pancreatic Β-cells and insulin secretion and potential treatment of type 1 diabetes. J Pharm Innov. 2016;11(2):156–61.
Mooranian A, Negrulj R, Al-Salami H. Flow vibration-doubled concentric system coupled with low ratio amine to produce bile acid-macrocapsules of beta-cells. Ther Deliv. 2016;7(3):171–8.
Mooranian A, Negrulj R, Al-Salami H. The impact of allylamine-bile acid combinations on cell delivery microcapsules in diabetes. J Microencapsul. 2016;33(6):569–74.
Mooranian A, Negrulj R, Al-Salami H. The incorporation of water-soluble gel matrix into bile acid-based microcapsules for the delivery of viable beta-cells of the pancreas, in diabetes treatment: biocompatibility and functionality studies. Drug Deliv Transl Res. 2016;6(1):17–23. https://doi.org/10.4155/tde-2015-0001.
Mooranian A, Negrulj R, Al-Salami H. Primary bile acid chenodeoxycholic acid-based microcapsules to examine β-cell survival and the inflammatory response. BioNanoScience. 2016;6(2):103–9.
Mooranian A, Negrulj R, Al-Salami H. Viability and topographical analysis of microencapsulated β-cells exposed to a biotransformed tertiary bile acid: an ex vivo study. Int J Nano Biomater. 2016;6(2):74–82. https://doi.org/10.1504/IJNBM.2016.079684.
Al-Salami H, Butt G, Tucker I, Mikov M. Influence of the semisynthetic bile acid (MKC) on the ileal permeation of gliclazide in healthy and diabetic rats. Methods Find Exp Clin Pharmacol. 2008;30(2):107–13. https://doi.org/10.1358/mf.2008.30.2.1159652.
Al-Salami H, Butt G, Tucker I, Golocorbin-Kon S, Mikov M. Probiotics decreased the bioavailability of the bile acid analog, monoketocholic acid, when coadministered with gliclazide, in healthy but not diabetic rats. Eur J Drug Metab Pharmacokinet. 2012;37(2):99–108. https://doi.org/10.1007/s13318-011-0060-y.
Al-Salami H, Butt G, Tucker I, Fawcett PJ, Golocorbin-Kon S, Mikov I, et al. Gliclazide reduces MKC intestinal transport in healthy but not diabetic rats. Eur J Drug Metab Pharmacokinet. 2009;34(1):43–50. https://doi.org/10.1007/BF03191383.
Mooranian A, Negrulj R, Takechi R, Mamo JC, Al-Sallami H, Al-Salami H. The biological effects of the hypolipidaemic drug probucol incorporated into bile acid-microcapsules and fed daily for 4-weeks, to an insulin-resistant mouse model: potential hypoglycaemic and anti-inflammatory effects. Drug Deliv and Transl Res. 2018. https://doi.org/10.1007/s13346-017-0473-5(In press).
Engin F, Yermalovich A, Nguyen T, Hummasti S, Fu W, Eizirik DL, et al. Restoration of the unfolded protein response in pancreatic beta cells protects mice against type 1 diabetes. Sci Transll Med. 2013;5(211):211ra156. https://doi.org/10.1126/scitranslmed.3006534.
Mooranian A, Negrulj R, Salami HA. Viability and topographical analysis of microencapsulated β-cells exposed to a biotransformed tertiary bile acid: an ex vivo study. Int J Nano Biomater. 2016;6(2):74–82. https://doi.org/10.1007/s11095-017-2138-y.
Shen A. A gut odyssey: the impact of the microbiota on clostridium difficile spore formation and germination. PLoS Pathog. 2015;11(10):e1005157. https://doi.org/10.1371/journal.ppat.1005157.
Einarsson C, Hillebrant CG, Axelson M. Effects of treatment with deoxycholic acid and chenodeoxycholic acid on the hepatic synthesis of cholesterol and bile acids in healthy subjects. Hepatology. 2001;33(5):1189–93. https://doi.org/10.1053/jhep.2001.23790.
Yasukawa K, Iida T, Fujimoto Y. Relative inhibitory activity of bile acids against 12-O-tetradecanoylphorbol-13-acetate-induced inflammation, and chenodeoxycholic acid inhibition of tumour promotion in mouse skin two-stage carcinogenesis. J Pharm Pharmacol. 2009;61(8):1051–6. https://doi.org/10.1211/jpp/61.08.0009.
Uchida A, Yamada T, Hayakawa T, Hoshino M. Taurochenodeoxycholic acid ameliorates and ursodeoxycholic acid exacerbates small intestinal inflammation. Am J Physiol. 1997. https://doi.org/10.1152/ajpgi.1997.272.5.g1249.
Woolbright BL, Li F, Xie Y, Farhood A, Fickert P, Trauner M, et al. Lithocholic acid feeding results in direct hepato-toxicity independent of neutrophil function in mice. Toxicol Lett. 2014;228(1):56–66. https://doi.org/10.1016/j.toxlet.2014.04.001.
Yu J, Lo JL, Huang L, Zhao A, Metzger E, Adams A, et al. Lithocholic acid decreases expression of bile salt export pump through farnesoid X receptor antagonist activity. J Biol Chem. 2002;277(35):31441–7. https://doi.org/10.1074/jbc.M200474200.
Acknowledgements
The authors would like to acknowledge the Australian Postgraduate Award (APA) and Curtin Research Scholarship (CRS). The authors also acknowledge the Curtin-seeding grant for the support and also acknowledge the use of laboratory equipment, scientific and technical assistance of Microscopy and Microanalysis Facility at Curtin University which has been partially funded by the University, State and Commonwealth Governments. The work is partially supported by the European Union Horizon 2020 research project and innovation program under the Marie Skłodowska-Curie Grant Agreement No 872370.
Author information
Authors and Affiliations
Contributions
Conception and design of the project: AM, RT, GL, BK, HA-S. Analysis and interpretation of research data: AM, NZ. CI, RT, GL, MM, S G-K, HA-S. Drafting significant part of the work or critically revising it, which contributes to the interpretation: AM, NZ, CI, RT, GL, MM, SG-K, BK, HA-S. Significant contribution to data interpretation and presentation resulting in significant improvement of quality: AM, NZ, CI, HA-S. Provided data or analytical skills, which add significantly to the design, quality and readability of the work: AM, NZ, CI, HA-S.
Corresponding author
Ethics declarations
Conflict of interest
Al-Salami H has been and is currently receiving of funding from Beijing Nat-Med Biotechnology Co. Ltd. The other authors have no conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Mooranian, A., Zamani, N., Ionescu, C.M. et al. Oral gavage of nano-encapsulated conjugated acrylic acid-bile acid formulation in type 1 diabetes altered pharmacological profile of bile acids, and improved glycaemia and suppressed inflammation. Pharmacol. Rep 72, 368–378 (2020). https://doi.org/10.1007/s43440-019-00030-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-019-00030-z