Abstract
Purpose
To assess the radiological morphometric parameters of OLIF surgical technique in lower lumbar spine among normal and in patients with adult degenerative spine (levoscoliosis and dextroscoliosis).
Method
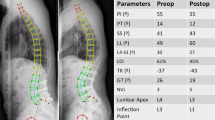
Standing AP radiographs and MRI in supine position were taken. Patients were divided into 3 groups based on Cobbs’ angle into normal, levo and dextro scoliosis. Moros classification was used to calculate bare window (BW), vascular window (VW), Psoas window (PW), psoas major height (pmh) and width (pmw) at lower lumbar levels and measurements were done on PACS.
Results
Seventy five patients (25 in each group) were assessed. BW has trend from L2-L3 > L3-L4 > L4-L5 in dextro and levoscoliosis. PW has trend from L3-L4 > L2-L3 > L4-L5 in levoscoliosis and normal group. VW has trend from L4-L5 > L3-L4 > L2-L3 in dextro and levoscoliosis; pmw has trend from L4-L5 > L3-L4 > L2-L3 in Levo and dextroscoliosis; pmh has trend from L4-L5 > L3-L4 > L2-L3 in levoscoliosis and normal group.
Conclusion
BW was noted to be highest at L3-4, lowest at L4-5 in normal group. VW was constant, BW showed a reverse trend with PW across all the levels. Though levoscoliosis group of patients had significantly higher BW, psoas retraction issues are to be kept in mind in view of anatomically taught psoas.








Similar content being viewed by others
References
Kaul R, Kumar H, Jeyaraman M et al (2021) MRI-based morphometric study regarding operative windows of oblique lumbar interbody fusion in Indian population. Indian J Orthop. https://doi.org/10.1007/s43465-021-00393-7
Silvestre C, Mac-Thiong JM, Hilmi R et al (2012) Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J 6(2):89–97. https://doi.org/10.4184/asj.2012.6.2.89
Wang Z, Liu L et al (2020) The OLIF working corridor based on magnetic resonance imaging: retrospective research. J Orthop Surg Res 15(1):141. https://doi.org/10.1186/s13018-020-01654-1
Ohtori S, Orita S et al (2015) Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for lumbar spinal degeneration disease. Yonsei Med J 56(4):1051. https://doi.org/10.3349/ymj.2015.56.4.1051
Sato J, Ohtori S, Orita S et al (2017) “Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis” by Jun by Jun Sato et al. Eur Spine J 2017(26):671–678. https://doi.org/10.1007/s00586-017-5326-x
Jin C, Jaiswal MS, Jeun S-S et al (2018) Outcomes of oblique lateral interbody fusion for degenerative lumbar disease in patients under or over 65 years of age. J Orthop Sur Res 13(1):38. https://doi.org/10.1186/s13018-018-0740-2
Ozgur BM, Aryan HE, Pimenta L et al (2006) Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 6(4):435–443. https://doi.org/10.1016/j.spinee.2005.08.012
Mayer HM (1997) A new microsurgical technique for minimally invasive anterior lumbar interbody fusion. Spine (Phila Pa 1976) 22:691–699
Moro T, Kikuchi S-I et al (2003) An anatomic study of the lumbar plexus with respect to retroperitoneal endoscopic surgery. Spine 28(5):423–427. https://doi.org/10.1097/01.brs.0000049226.87064.3b
Chen X, Chen J, Zhang F (2019) Imaging anatomic research of oblique lumbar interbody fusion in a Chinese population based on magnetic resonance. World Neurosurg 128:e51–e58. https://doi.org/10.1016/j.wneu.2019.03.244
Davis TT, Hynes RA et al (2014) Retroperitoneal oblique corridor to the L2–S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine 21:785–793. https://doi.org/10.3171/2014.7.SPINE13564
Watkins RG, Hanna R et al (2014) Sagittal alignment after lumbar interbody fusion. J Spinal Disord Tech 27(5):253–256. https://doi.org/10.1097/BSD.0b013e31828a8447
Fujibayashi S, Kawakami N et al (2017) Complications associated with lateral interbody fusion. Spine. https://doi.org/10.1097/brs.0000000000002139
LiMobbs JXRJ et al (2018) Morphometric MRI imaging study of the corridor for the oblique lumbar interbody fusion technique at L1-L5. World Neurosurg 111:e678–e685. https://doi.org/10.1016/j.wneu.2017.12.136
Elowitz E, Yanni D, Chwajol M et al (2011) Evaluation of indirect decompression of the lumbar spinal canal following minimally invasive lateral transpsoas interbody fusion: radiographic and outcome analysis. Min Minim Invasive Neurosurg 54:201–206. https://doi.org/10.1055/s-0031-1286334
Oliveira L, Marchi L et al (2010) A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine 35(Supplement):S331–S337. https://doi.org/10.1097/brs.0b013e3182022db0
Yuan W, Kaliya-Perumal A-K et al (2019) Does lumbar interbody cage size influence subsidence? A biomechanical study. Spine. https://doi.org/10.1097/brs.0000000000003194
Zhu G, Hao Y et al (2018) Comparing stand-alone oblique lumbar interbody fusion with posterior lumbar interbody fusion for revision of rostral adjacent segment disease. Medicine 97(40):e12680. https://doi.org/10.1097/MD.0000000000012680
Kim D-B, Shin M-H et al (2018) Vertebral body rotation in patients with lumbar degenerative scoliosis: surgical implication for oblique lumbar interbody fusion. World Neurosurg. https://doi.org/10.1016/j.wneu.2018.12.073
Ng JP, Kaliya-Perumal AK, Tandon AA et al (2020) The oblique corridor at L4–L5: a radiographic-anatomical study into the feasibility for lateral interbody fusion. Spine (Phila Pa 1976) 45(10):E552–E559. https://doi.org/10.1097/BRS.0000000000003346
Regev GJ, Kim CW (2014) Safety and the anatomy of the retroperitoneal lateral corridor with respect to the minimally invasive lateral lumbar intervertebral fusion approach. Neurosurg Clin N Am 25(2):211–218. https://doi.org/10.1016/j.nec.2013.12.001
Silva FE, Lenke LG (2010) Adult degenerative scoliosis: evaluation and management. Neurosurg Focus 28(3):E1. https://doi.org/10.3171/2010.1.focus09271
TempelGandhoke ZJGS et al (2014) Radiographic and clinical outcomes following combined lateral lumbar interbody fusion and posterior segmental stabilization in patients with adult degenerative scoliosis. Neurosurg Focus 36(5):E11. https://doi.org/10.3171/2014.3.focus13368
Birknes JK, Harrop JS et al (2008) Adult degenerative scoliosis. Neurosurgery 63(Supplement):A94–A103. https://doi.org/10.1227/01.neu.0000325485.49323.b2
Aebi M (2005) The adult scoliosis. Eur Spine J 14(10):925–948. https://doi.org/10.1007/s00586-005-1053-9
Molinares DM, Davis TT et al (2016) Retroperitoneal oblique corridor to the L2–S1 intervertebral discs: an MRI study. J Neurosurg Spine 24(2):248–255. https://doi.org/10.3171/2015.3.SPINE13976
Liu L, LiangZhang YH et al (2016) Imaging anatomical research on the operative windows of oblique lumbar interbody fusion. PLoS ONE 11(9):e0163452. https://doi.org/10.1371/journal.pone.0163452
Zhang F, Xu H et al (2017) Does right lateral decubitus position change retroperitoneal oblique corridor? A radiographic evaluation from L1 to L5. Eur Spine J 26(3):646–650. https://doi.org/10.1007/s00586-016-4645-7
Milbrandt TA, Sucato DJ (2007) The position of the aorta relative to the spine in patients with left thoracic scoliosis. Spine 32(12):E348–E353. https://doi.org/10.1097/brs.0b013e318059aeda
Sevastik B, Xiong B, Hedlund R et al (1996) The position of the aorta in relation to the vertebra in patients with idiopathic thoracic scoliosis. Surg Radiol Anat 18(1):51–56. https://doi.org/10.1007/bf03207763
Liang Yan, Shuai Xu, Zhao Yongfei et al (2021) The effects of vertebral rotation on the position of the aorta relative to the spine in patients with adult degenerative scoliosis. Therapeutic. https://doi.org/10.1177/20206223211027108
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
DD: approved the version to be published, drafted the article. VP: acquisition/analysis/interpretation of data. BD: conception of work. AK: drafted the work. SM: drafted the work. RRR: interpretation of data. SB: acquisition and analysis of data. PA: approved the article version. PA: investigated and resolved questions related to the integrity of work.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest.
Ethical approval
The study was approved institutional ethical committee and has been registered in the clinical trial registration of India (CTRI/2022/02/040128).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Degulmadi, D., Parmar, V., Dave, B. et al. A comparative morphometric analysis of operative windows for performing OLIF among normal and deformity group in lower lumbar spine. Spine Deform 11, 455–462 (2023). https://doi.org/10.1007/s43390-022-00594-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00594-6