Abstract
Study design
Retrospective comparative study.
Objectives
In patients with cerebral palsy (CP), we determine the impact of intrathecal baclofen pumps (ITBPs) on scoliosis curve progression before posterior spine fusion (PSF) and its effects on surgical outcome.
Background
Children with CP can have rapid scoliosis progression, and high rates of surgical complications can be encountered. It is unknown whether the presence of pre-existing ITBP results in more difficult surgery and higher complication rates in similarly affected children.
Methods
This is a single-center retrospective study of CP patients undergoing PSF over a 15-year period. Demographics, comorbidities, curve magnitudes, and surgical methods were compared between patients with ITBP and those without. Postoperative complications, length of intensive care unit/hospital stay, drain use and output volume, and need for further surgery were also compared. Curve progression analysis after ITBP placement was performed on a subgroup of patients with high-quality consistent radiographs.
Results
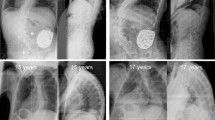
Nineteen patients with ITBP and 49 patients without ITBP met inclusion criteria. Age, comorbidities, number of levels fused, and fixation techniques during PSF were not significantly different between cohorts. ITBP patients were more likely to have PSF with osteotomy (p = 0.022). Increased intraoperative neurosurgical consultations were found for patients with ITBP (42.1% vs. 4.0%; p < 0.001). Median surgical time was 1.2 h greater in patients with ITBP (6.7 vs. 5.5 h, p = 0.039). There was no difference in hospital course and complications in patients with ITBP and those without ITBP. Thirty-one patients without ITB were compared with 15 ITBP patients for curve progression before PSF, demonstrating a mean rate of scoliosis progression of 9.6° ± 6.7°/year and 14.8° ± 9.1°/year (p = 0.0346), respectively.
Conclusion
The presence of an ITBP appears to be associated with the increase in scoliosis progression; and these patients will likely have a more challenging spine fusion. Fortunately, the final outcome is not affected by ITBP.
Level of evidence
Level III.

Similar content being viewed by others
References
Data and statistics for cerebral palsy [CDC Web site], May 2, 2016. http://www.cdc.gov/ncbddd/cp/data.html. Accessed 25 Feb 2017
Jones-Quaidoo SM, Yang S, Arlet V (2010) Surgical management of spinal deformities in cerebral palsy: a review. J Neurosurg Spine 13:672–685
Morrell DS, Pearson JM, Sauser DD (2002) Progressive bone and joint abnormalities of the spine and lower extremities in cerebral palsy. Radiographics 22:257–268
Sarwark J, Sarwahi V (2007) New strategies and decision making in the management of neuromuscular scoliosis. Orthop Clin North Am 38:485–496
Scannell B, Yaszay B (2015) Scoliosis, spinal fusion and intrathecal baclofen pump implantation. Phys Med Rehabil Clin N Am 26:79–88
Watanabe K, Lenke LG, Daubs MD et al (2009) Is spinal deformity surgery in patients with spastic cerebral palsy truly beneficial? Spine 34:2222–2232
Mohamad F, Parent S, Pawelek J et al (2007) Perioperative complications after surgical correction in neuromuscular scoliosis. J Pediatr Orthop 27:392–397
Master DL, Son-Hing JP, Poe-Kochert C et al (2011) Risk factors for major complications after surgery for neuromuscular scoliosis. Spine (Phila Pa 1976) 36:564–571
Albright AL, Cervi A, Singletary J (1991) Intrathecal baclofen for spasticity in cerebral palsy. JAMA 265:1418–1422
Walter M, Altermatt S, Furrer C et al (2014) Intrathecal baclofen therapy in children with severe spasticity: outcome and complications. Dev Neurorehabil 17:368–374
Saulino M, Ivanhoe CB, McGuire JR et al (2016) Best practices for intrathecal baclofen therapy: patient selection. Neuromodulation 19:607–615
Yaszay B, Scannell BP, Bomar JD et al (2015) Although inconvenient, baclofen pumps do not complicate scoliosis surgery in patients with cerebral palsy. Spine (Phila Pa 1976) 40:E504–E509
Lynn AK, Turner M, Chambers HG (2009) Surgical management of spasticity in persons with cerebral palsy. PMR 1:834–838
Kim YJ, Bridwell KH, Lenke LG et al (2005) Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Spine (Phila Pa 1976) 30:2045–2050
Glattes RC, Bridwell KH, Lenke LG et al (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine 30:1643–1649
Cobb JR (1948) Outline of the study of scoliosis. Instr Course Lect 5:261–271
Gupta MC, Wijesekera S, Sossan A et al (2007) Reliability of radiographic parameters in neuromuscular scoliosis. Spine 32:691–695
Hostin R, McCarthy I, O’Brien M et al (2013) Incidence, mode, and location of acute proximal junctional failures after surgical treatment of adult spinal deformity. Spine 20(38):1008–1015
Borowski A, Shah SA, Littleton AG et al (2008) Baclofen pump implantation and spinal fusion in children: techniques and complications. Spine (Phila Pa 1976) 33:1995–2000
Caird MS, Palanca AA, Garton H et al (2008) Outcomes of posterior spinal fusion and instrumentation in patients with continuous intrathecal baclofen infusion pumps. Spine (Phila Pa 1976) 33:E94–E99
Li G, Sun TW, Luo G, Zhang C (2017) Efficacy of antifibrinolytic agents on surgical bleeding and transfusion requirements in spine surgery: a meta-analysis. Eur Spine J 26:140–154
McNicol ED, Tzortzopoulou A, Schumann R et al (2016) Antifibrinolytic agents for reducing blood loss in scoliosis surgery in children. Cochrane Database Syst Rev 9:CD006883
Sethna NF, Zurakowski D, Brustowicz RM et al (2005) Tranexamic acid reduces intraoperative blood loss in pediatric patients undergoing scoliosis surgery. Anesthesiology 102:727–732
Dhawale AA, Shah SA, Sponseller PD et al (2012) Are antifibrinolytics helpful in decreasing blood loss and transfusions during spinal fusion surgery in children with cerebral palsy scoliosis? Spine (Phila Pa 1976) 37:E549–E555
Elgafy H, Bransford RJ, McGuire RA et al (2010) Blood loss in major spine surgery: are there effective measures to decrease massive hemorrhage in major spine fusion surgery? Spine (Phila Pa 1976) 35:S47–S56
Jain A, Sponseller PD, Shah SA et al (2017) Incidence of and risk factors for loss of 1 blood volume during spinal fusion surgery in patients with cerebral palsy. J Pediatr Orthop 37:e484–e487
Ginsburg GM, Lauder AJ (2007) Progression of scoliosis in patients with spastic quadriplegia after the insertion of an intrathecal baclofen pump. Spine (Phila Pa 1976) 32:2745–2750
Saito N, Ebara S, Ohotsuka K et al (1998) Natural history of scoliosis in spastic cerebral palsy. Lancet 351:1687–1692
Funding
Shapiro Summer Research; UW Department of Orthopedics and Rehabilitation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
LABL (none), AVN (none), MAH (none), SJH (none), KJN (a patent “Spine Implants” with royalties paid to Biomet).
IRB approval
Approval was obtained from the University of Wisconsin institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lins, L.A.B., Nechyporenko, A.V., Halanski, M.A. et al. Does an intrathecal baclofen pump impact scoliosis progression and complicate posterior spine fusion in patients with cerebral palsy?. Spine Deform 8, 115–121 (2020). https://doi.org/10.1007/s43390-020-00034-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00034-3