Abstract
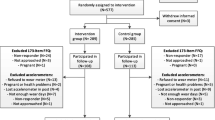
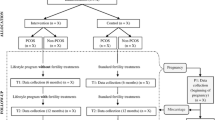
Atherogenic dyslipidemia—before or during pregnancy—may contribute to preeclampsia and subsequent cardiovascular disease risk. We performed a nested case-control study to further understand dyslipidemia associated with preeclampsia. The cohort consisted of participants in the randomized clinical trial “Improving Reproductive Fitness Through Pretreatment with Lifestyle Modification in Obese Women with Unexplained Infertility” (FIT-PLESE). FIT-PLESE was designed to study the effect of a pre-fertility treatment 16-week randomized lifestyle intervention program (Nutrisystem diet + exercise + orlistat vs. training alone) on improvement in live birth rate among obese women with unexplained infertility. Of the 279 patients in FIT-PLESE, 80 delivered a viable infant. Maternal serum was analyzed across five visits: before and after lifestyle interventions and also at three pregnancy visits (16, 24, and 32 weeks gestation). Apolipoprotein lipids were measured in a blinded fashion using ion mobility. Cases were those who developed preeclampsia. Controls also had a live birth but did not develop preeclampsia. Generalized linear and mixed models with repeated measures were used to compare the mean lipoprotein lipid levels of the two groups across all visits. Complete data were available for 75 pregnancies, and preeclampsia developed in 14.5% of the pregnancies. Cholesterol/high-density lipoprotein (HDL) ratios (p < 0.003), triglycerides (p = 0.012), and triglyceride/HDL ratios, all adjusted for BMI, were worse in patients with preeclampsia (p < 0.001). Subclasses a, b, and c of highly atherogenic, very small, low-density lipoprotein (LDL) particles were higher during pregnancy for the preeclamptic women (p < 0.05). Very small LDL particle subclass d levels were significantly greater only at 24 weeks (p = 0.012). The role of highly atherogenic, very small LDL particle excess in the pathophysiology of preeclampsia awaits further investigation.


Similar content being viewed by others
Data Availability
Yes, the corresponding author may be contacted to obtain.
Code Availability
Not applicable.
References
Mozaffarian D, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–360.
Mehta LS, et al. Cardiovascular considerations in caring for pregnant patients: a scientific statement from the American Heart Association. Circulation. 2020;141(23):e884–903.
Burton GJ, et al. Pre-eclampsia: pathophysiology and clinical implications. BMJ. 2019;366:l2381.
Spracklen CN, et al. Maternal hyperlipidemia and the risk of preeclampsia: a meta-analysis. Am J Epidemiol. 2014;180(4):346–58.
Gallos ID, et al. Pre-eclampsia is associated with, and preceded by, hypertriglyceridaemia: a meta-analysis. BJOG. 2013;120(11):1321–32.
Hubel CA. Dyslipidemia, iron, and oxidative stress in preeclampsia: assessment of maternal and feto-placental interactions. Semin Reprod Endocrinol. 1998;16(1):75–92.
Hubel CA, et al. Small low-density lipoproteins and vascular cell adhesion molecule-1 are increased in association with hyperlipidemia in preeclampsia. Metabolism. 1998;47(10):1281–8.
Spradley FT. Metabolic abnormalities and obesity's impact on the risk for developing preeclampsia. Am J Physiol Regul Integr Comp Physiol. 2017;312(1):R5–r12.
Zobel EH, et al. Global changes in food supply and the obesity epidemic. Curr Obes Rep. 2016;5(4):449–55.
Ogunwole SM, Zera CA, Stanford FC. Obesity management in women of reproductive age. JAMA. 2021;325(5):433–4.
Björnson E, et al. Kinetics of plasma triglycerides in abdominal obesity. Curr Opin Lipidol. 2017;28(1):11–8.
Best D, Bhattacharya S. Obesity and fertility. Horm Mol Biol Clin Investig. 2015;24(1):5–10.
Legro RS, et al. Effects of preconception lifestyle intervention in infertile women with obesity: the FIT-PLESE randomized controlled trial. PLoS Med. 2022;19(1):e1003883.
Llurba E, et al. Atherogenic lipoprotein subfraction profile in preeclamptic women with and without high triglycerides: different pathophysiologic subsets in preeclampsia. Metabolism. 2005;54(11):1504–9.
Kim-Dorner SJ, et al. Should triglycerides and the triglycerides to high-density lipoprotein cholesterol ratio be used as surrogates for insulin resistance? Metabolism. 2010;59(2):299–304.
Salma U. Relationship of serum lipid profiles in preeclampsia and normal pregnancy. Bangladesh. Afr Health Sci. 2022;22(2):475–9.
Tesfa E, Nibret E, Munshea A. Maternal lipid profile and risk of pre-eclampsia in African pregnant women: a systematic review and meta-analysis. PLoS One. 2020;15(12):e0243538.
Roberts JM, Redman CW. Pre-eclampsia: more than pregnancy-induced hypertension. Lancet. 1993;341(8858):1447–51.
Roberts JM, et al. Preeclampsia: an endothelial cell disorder. Am J Obstet Gynecol. 1989;161(5):1200–4.
Hulthe J, et al. LDL particle size in relation to intima-media thickness and plaque occurrence in the carotid and femoral arteries in patients with hypercholesterolaemia. J Intern Med. 2000;248(1):42–52.
Wolfrum S, Jensen KS, Liao JK. Endothelium-dependent effects of statins. Arterioscler Thromb Vasc Biol. 2003;23(5):729–36.
Furchgott RF, Vanhoutte PM. Endothelium-derived relaxing and contracting factors. Faseb J. 1989;3(9):2007–18.
Salafia Carolyn SR, Thomas T, Paneth N, Abela G, Wild RA. Pregnancy-induced hypertension: the potential role of cholesterol crystals in the maternal decidua. J Clin Lipidol. 2022;23(11):41.
El Khouly NI, et al. Value of first-trimester serum lipid profile in early prediction of preeclampsia and its severity: a prospective cohort study. Hypertens Pregnancy. 2016;35(1):73–81.
Adank MC, et al. Is maternal lipid profile in early pregnancy associated with pregnancy complications and blood pressure in pregnancy and long term postpartum? Am J Obstet Gynecol. 2019;221(2):150.e1–150.e13.
Ardalić D, et al. Lipid profile and lipid oxidative modification parameters in the first trimester of high- risk pregnancies - possibilities for preeclampsia prediction. Clin Biochem. 2020;81:34–40.
Rasmussen M, et al. RNA profiles reveal signatures of future health and disease in pregnancy. Nature. 2022;601(7893):422–7.
Hauspurg A, et al. Association of N-terminal pro-brain natriuretic peptide concentration in early pregnancy with development of hypertensive disorders of pregnancy and future hypertension. JAMA Cardiol. 2022;7(3):268–76.
Funding
This study work was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) grants U10HD077680 Reproductive Medicine Network (RMN) and 1 R03 HD101893-01 and a contract for blind analysis of the lipoprotein lipids from Quest Diagnostics. Presented in part at the Society for Reproductive Investigation (SRI) 68th Annual Meeting in Boston, Massachusetts: Abstract O-010 Reproductive Sciences Vol 28, Supplement 1, July 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
IRB approval obtained from the University of Oklahoma
Consent to Participate
For all authors, yes.
Consent for Publication
For all authors, yes.
Competing Interests
None related to this manuscript. Dr. Wren was the Clinical Director of Quest laboratories at the time of the lipoprotein analysis.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wild, R.A., Edwards, R.K., Zhao, D. et al. Highly Atherogenic Lipid Particles are Associated with Preeclampsia After Successful Fertility Treatment for Obese Women who have Unexplained Infertility. Reprod. Sci. 30, 2495–2502 (2023). https://doi.org/10.1007/s43032-023-01197-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-023-01197-w