Abstract
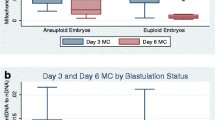
The purpose of this study was to determine if morphometric parameters that can be measured quantitatively using a time-lapse embryo incubator are associated with aneuploidy. Embryos cultured in a time-lapse incubator and assessed with preimplantation genetic testing for aneuploidy (PGT-A) were analyzed retrospectively. Morphokinetic analysis included timing of cell divisions. Quantitative morphometric measurements included the distance between the second and first polar body, zona pellucida thickness at the pronuclear stage and at the 2-cell stage, and blastomere area at the 2- and 4-cell stages. Symmetry at the 2-cell stage was determined by percent difference between blastomeres; symmetry at the 4-cell stage was the percent difference between the smallest and largest blastomeres. Maternal age, blastocyst grade and day of biopsy were recorded. Euploid embryo characteristics were compared to aneuploid embryos. A receiver operating characteristic (ROC) curve was used to evaluate cell symmetry as a predictor of aneuploidy. Embryos (n = 182) from 21 patients (age 22–43; median = 34) were analyzed. Of the 182 embryos, 45% were euploid. Euploid and aneuploid embryos had similar morphokinetics and morphometry across many measures. As expected, age and blastocyst grade were associated with embryo ploidy. It was notable that, additionally, symmetry at the 4-cell stage (27% vs 31%, p = 0.01) was also associated with embryo ploidy. The optimized cutoff from the ROC curve to predict aneuploidy was determined to be 21%. Embryos with > 21% asymmetry at the 4-cell stage had high rates of aneuploidy while morphokinetic parameters were similar. In conclusion, this suggests that embryo selection models using time-lapse parameters would improve if they incorporate cleavage-stage morphometrics.



Similar content being viewed by others
Data availability
Upon request.
Code availability
Not applicable.
References
Glujovsky D, Farquhar C, QuinteiroRetamar AM, Alvarez Sedo CR, Blake D. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev. 2016;6:CD002118.
Schoolcraft WB, Treff NR, Stevens JM, Ferry K, Katz-Jaffe M, Scott RT Jr. Live birth outcome with trophectoderm biopsy, blastocyst vitrification, and single-nucleotide polymorphism microarray-based comprehensive chromosome screening in infertile patients. Fertil Steril. 2011;96(3):638–40.
Scott RT Jr, Ferry K, Su J, Tao X, Scott K, Treff NR. Comprehensive chromosome screening is highly predictive of the reproductive potential of human embryos: a prospective, blinded, nonselection study. Fertil Steril. 2012;97(4):870–5.
Scott RT Jr, Upham KM, Forman EJ, Hong KH, Scott KL, Taylor D, et al. Blastocyst biopsy with comprehensive chromosome screening and fresh embryo transfer significantly increases in vitro fertilization implantation and delivery rates: a randomized controlled trial. Fertil Steril. 2013;100(3):697–703.
Kang HJ, Melnick AP, Stewart JD, Xu K, Rosenwaks Z. Preimplantation genetic screening: who benefits? Fertil Steril. 2016;106(3):597–602.
Munne S, Kaplan B, Frattarelli JL, Child T, Nakhuda G, Shamma FN, et al. Preimplantation genetic testing for aneuploidy versus morphology as selection criteria for single frozen-thawed embryo transfer in good-prognosis patients: a multicenter randomized clinical trial. Fertil Steril. 2019;112(6):1071-9e7.
Campbell A, Fishel S, Bowman N, Duffy S, Sedler M, Hickman CF. Modelling a risk classification of aneuploidy in human embryos using non-invasive morphokinetics. Reprod Biomed Online. 2013;26(5):477–85.
Campbell A, Fishel S, Bowman N, Duffy S, Sedler M, Thornton S. Retrospective analysis of outcomes after IVF using an aneuploidy risk model derived from time-lapse imaging without PGS. Reprod Biomed Online. 2013;27(2):140–6.
Kramer YG, Kofinas JD, Melzer K, Noyes N, McCaffrey C, Buldo-Licciardi J, et al. Assessing morphokinetic parameters via time lapse microscopy (TLM) to predict euploidy: are aneuploidy risk classification models universal? J Assist Reprod Genet. 2014;31(9):1231–42.
Liu Y, Qi F, Matson P, Morbeck DE, Mol BW, Zhao S, et al. Between-laboratory reproducibility of time-lapse embryo selection using qualitative and quantitative parameters: a systematic review and meta-analysis. J Assist Reprod Genet. 2020;37(6):1295–302.
Coticchio G, Mignini Renzini M, Novara PV, Lain M, De Ponti E, Turchi D, et al. Focused time-lapse analysis reveals novel aspects of human fertilization and suggests new parameters of embryo viability. Hum Reprod. 2018;33(1):23–31.
Derrick R, Hickman C, Oliana O, Wilkinson T, Gwinnett D, Whyte LB, et al. Perivitelline threads associated with fragments in human cleavage stage embryos observed through time-lapse microscopy. Reprod Biomed Online. 2017;35(6):640–5.
Luke B, Brown MB, Stern JE, Jindal SK, Racowsky C, Ball GD. Using the Society for Assisted Reproductive Technology Clinic Outcome System morphological measures to predict live birth after assisted reproductive technology. Fertil Steril. 2014;102(5):1338–44.
Kovacs P. Embryo selection: the role of time-lapse monitoring. Reprod Biol Endocrinol. 2014;12:124.
Franasiak JM, Forman EJ, Hong KH, Werner MD, Upham KM, Treff NR, et al. The nature of aneuploidy with increasing age of the female partner: a review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil Steril. 2014;101(3):656-63e1.
Capalbo A, Rienzi L, Cimadomo D, Maggiulli R, Elliott T, Wright G, et al. Correlation between standard blastocyst morphology, euploidy and implantation: an observational study in two centers involving 956 screened blastocysts. Hum Reprod. 2014;29(6):1173–81.
Greco E, Minasi MG, Fiorentino F. Healthy babies after intrauterine transfer of mosaic aneuploid blastocysts. N Engl J Med. 2015;373(21):2089–90.
Neal SA, Morin SJ, Franasiak JM, Goodman LR, Juneau CR, Forman EJ, et al. Preimplantation genetic testing for aneuploidy is cost-effective, shortens treatment time, and reduces the risk of failed embryo transfer and clinical miscarriage. Fertil Steril. 2018;110(5):896–904.
Rubio I, Galan A, Larreategui Z, Ayerdi F, Bellver J, Herrero J, et al. Clinical validation of embryo culture and selection by morphokinetic analysis: a randomized, controlled trial of the EmbryoScope. Fertil Steril. 2014;102(5):1287-94e5.
Pribenszky C, Nilselid AM, Montag M. Time-lapse culture with morphokinetic embryo selection improves pregnancy and live birth chances and reduces early pregnancy loss: a meta-analysis. Reprod Biomed Online. 2017;35(5):511–20.
Neuber E, Rinaudo P, Trimarchi JR, Sakkas D. Sequential assessment of individually cultured human embryos as an indicator of subsequent good quality blastocyst development. Hum Reprod. 2003;18(6):1307–12.
Racowsky C, Stern JE, Gibbons WE, Behr B, Pomeroy KO, Biggers JD. National collection of embryo morphology data into Society for Assisted Reproductive Technology Clinic Outcomes Reporting System: associations among day 3 cell number, fragmentation and blastomere asymmetry, and live birth rate. Fertil Steril. 2011;95(6):1985–9.
Tain DCX, Lim MSR, Ng BL, Hammond E, Wong PS. The influence of day 2 blastomere symmetry on blastocyst grade and ploidy status. Fertility & Reproduction. 2019;01(02):115–8.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Chandra Shenoy. The first draft of the manuscript was written by Chandra Shenoy and Dean Morbeck commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
IRB approved by Mayo Clinic Institutional Review Board 15–007799. Waived by IRB due to retrospective nature. Patients who did not complete Minnesota Research Authorization were excluded.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Shenoy, C.C., Khan, Z., Coddington, C.C. et al. Symmetry at the 4-Cell Stage Is Associated with Embryo Aneuploidy. Reprod. Sci. 28, 3473–3479 (2021). https://doi.org/10.1007/s43032-021-00758-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00758-1