Abstract
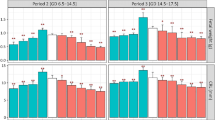
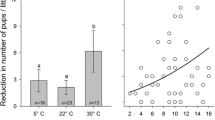
Physiological adaptations during heat exposure are critical in pregnancy. Maternal thermoregulation has to accommodate the increased metabolic load of the developing fetus. Here, we assess the consequences of intermittent heat exposure, as occurs in heat waves, for maternal adaptations during pregnancy, and chronic feto-placental outcomes. Following timed mating, C57BL/6J mice were allocated to either standard animal housing temperature conditions (SH) or housing at a temperature within the thermoneutral zone (TNZ). A subset of the TNZ group was exposed to 37 °C for 8 h a day from E15.5 to E17.5 to simulate a heat wave (HW). Maternal weight gain, food intake, rectal temperature, and nesting behaviors were measured across gestation. Fetal and placental tissues were collected at E18.5. With heat exposure, maternal rectal temperature increased while food intake and nest complexity decreased. Maternal daily weight gain initially decreased due to heat exposure, but on the last day of exposure, it was comparable to the other experimental groups. These maternal responses during heat exposure impacted on the fetus, with restrictions in placental and fetal development evident just before birth. Thus, the vascular portion of the placenta, and the relative fetal head size, was smaller. Furthermore, SH and TNZ animals demonstrated distinct differences in food intake and nesting behavior during pregnancy, reinforcing the need for caution in extrapolating from animal models to humans when housing occurs outside of thermoneutral zone conditions. This study highlights the direct effects of temperature conditions on health in pregnancy and provides a foundation for future studies to investigate fetal health consequences that are associated with intermittent heat exposure.



Similar content being viewed by others
References
Watts N, Amann M, Ayeb-Karlsson S, Belesova K, Bouley T, Boykoff M, et al. The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet. 2018;391(10120):581–630. https://doi.org/10.1016/S0140-6736(17)32464-9.
Xu C, Kohler TA, Lenton TM, Svenning JC, Scheffer M. Future of the human climate niche. Proc Natl Acad Sci U S A. 2020;117:11350–5. https://doi.org/10.1073/pnas.1910114117.
Steffen W, Hughes L, Perkins S. Heatwaves: hotter, longer, more often. Climate Council of Australia 2014.
Schroder HJ, Power GG. Engine and radiator: fetal and placental interactions for heat dissipation. Exp Physiol. 1997;82(2):403–14.
Laburn HP, Faurie A, Goelst K, Mitchell D. Effects on fetal and maternal body temperatures of exposure of pregnant ewes to heat, cold, and exercise. J Appl Physiol (1985). 2002;92(2):802–8. https://doi.org/10.1152/japplphysiol.00109.2001.
Laburn HP, Mitchell D, Goelst K. Fetal and maternal body temperatures measured by radiotelemetry in near-term sheep during thermal stress. J Appl Physiol (1985). 1992;72(3):894–900. https://doi.org/10.1152/jappl.1992.72.3.894.
Cil G, Cameron TA. Potential climate change health risks from increases in heat waves: abnormal birth outcomes and adverse maternal health conditions. Risk Anal. 2017;37(11):2066–79. https://doi.org/10.1111/risa.12767.
Basu R, Rau R, Pearson D, Malig B. Temperature and term low birth weight in California. Am J Epidemiol. 2018;187:2306–14. https://doi.org/10.1093/aje/kwy116.
Zheng X, Zhang W, Lu C, Norback D, Deng Q. An epidemiological assessment of the effect of ambient temperature on the incidence of preterm births: identifying windows of susceptibility during pregnancy. J Therm Biol. 2018;74:201–7. https://doi.org/10.1016/j.jtherbio.2018.04.001.
Kuehn L, McCormick S. Heat exposure and maternal health in the face of climate change. Int J Environ Res Public Health. 2017;14(8). doi:https://doi.org/10.3390/ijerph14080853.
Wang J, Williams G, Guo Y, Pan X, Tong S. Maternal exposure to heatwave and preterm birth in Brisbane, Australia. BJOG. 2013;120(13):1631–41. https://doi.org/10.1111/1471-0528.12397.
Beltran AJ, Wu J, Laurent O. Associations of meteorology with adverse pregnancy outcomes: a systematic review of preeclampsia, preterm birth and birth weight. Int J Environ Res Public Health. 2013;11(1):91–172. https://doi.org/10.3390/ijerph110100091.
Vicedo-Cabrera AM, Iniguez C, Barona C, Ballester F. Exposure to elevated temperatures and risk of preterm birth in Valencia, Spain. Environ Res. 2014;134:210–7. https://doi.org/10.1016/j.envres.2014.07.021.
Hansen PJ. Effects of heat stress on mammalian reproduction. Philos Trans R Soc Lond Ser B Biol Sci. 2009;364(1534):3341–50. https://doi.org/10.1098/rstb.2009.0131.
Koyama H, Ikeda S, Sugimoto M, Kume S. Effects of folic acid on the development and oxidative stress of mouse embryos exposed to heat stress. Reprod Domest Anim. 2012;47(6):921–7. https://doi.org/10.1111/j.1439-0531.2012.01992.x.
Ziskin MC, Morrissey J. Thermal thresholds for teratogenicity, reproduction, and development. Int J Hyperth. 2011;27(4):374–87. https://doi.org/10.3109/02656736.2011.553769.
Thureen PJ, Trembler KA, Meschia G, Makowski EL, Wilkening RB. Placental glucose transport in heat-induced fetal growth retardation. Am J Phys. 1992;263(3 Pt 2):R578–85. https://doi.org/10.1152/ajpregu.1992.263.3.R578.
Dreiling CE, Carman FS 3rd, Brown DE. Maternal endocrine and fetal metabolic responses to heat stress. J Dairy Sci. 1991;74(1):312–27. https://doi.org/10.3168/jds.S0022-0302(91)78175-7.
Regnault TR, Orbus RJ, de Vrijer B, Davidsen ML, Galan HL, Wilkening RB, et al. Placental expression of VEGF, PlGF and their receptors in a model of placental insufficiency-intrauterine growth restriction (PI-IUGR). Placenta. 2002;23(2–3):132–44. https://doi.org/10.1053/plac.2001.0757.
Fischer AW, Cannon B, Nedergaard J. Optimal housing temperatures for mice to mimic the thermal environment of humans: an experimental study. Mol Metab. 2018;7:161–70. https://doi.org/10.1016/j.molmet.2017.10.009.
Ganeshan K, Chawla A. Warming the mouse to model human diseases. Nat Rev Endocrinol. 2017;13(8):458–65. https://doi.org/10.1038/nrendo.2017.48.
Maloney SK, Fuller A, Mitchell D, Gordon C, Overton JM. Translating animal model research: does it matter that our rodents are cold? Physiology (Bethesda). 2014;29(6):413–20. https://doi.org/10.1152/physiol.00029.2014.
Hess SE, Rohr S, Dufour BD, Gaskill BN, Pajor EA, Garner JP. Home improvement: C57BL/6J mice given more naturalistic nesting materials build better nests. J Am Assoc Lab Anim Sci. 2008;47(6):25–31.
Clarke MW, Tuckey RC, Gorman S, Holt B, Hart PH. Optimized 25-hydroxyvitamin D analysis using liquid–liquid extraction with 2D separation with LC/MS/MS detection, provides superior precision compared to conventional assays. Metabolomics. 2013;9(5):1031–40. https://doi.org/10.1007/s11306-013-0518-9.
Wharfe MD, Mark PJ, Wyrwoll CS, Smith JT, Yap C, Clarke MW, et al. Pregnancy-induced adaptations of the central circadian clock and maternal glucocorticoids. J Endocrinol. 2016;228(3):135–47. https://doi.org/10.1530/JOE-15-0405.
Tesic D, Hawes JE, Zosky GR, Wyrwoll CS. Vitamin D deficiency in BALB/c mouse pregnancy increases placental transfer of glucocorticoids. Endocrinology. 2015;156(10):3673–9. https://doi.org/10.1210/en.2015-1377.
Roberts CT, White CA, Wiemer NG, Ramsay A, Robertson SA. Altered placental development in interleukin-10 null mutant mice. Placenta. 2003;24 Suppl A:S94–9.
Groves NJ, Kesby JP, Eyles DW, McGrath JJ, Mackay-Sim A, Burne TH. Adult vitamin D deficiency leads to behavioural and brain neurochemical alterations in C57BL/6J and BALB/c mice. Behav Brain Res. 2013;241:120–31. https://doi.org/10.1016/j.bbr.2012.12.001.
Fewell JE. Body temperature regulation in rats near term of pregnancy. Can J Physiol Pharmacol. 1995;73(3):364–8.
Wharfe MD, Wyrwoll CS, Waddell BJ, Mark PJ. Pregnancy suppresses the daily rhythmicity of core body temperature and adipose metabolic gene expression in the mouse. Endocrinology. 2016;157(9):3320–31. https://doi.org/10.1210/en.2016-1177.
Crew RC, Waddell BJ, Maloney SK, Mark PJ. Diet-induced obesity reduces core body temperature across the estrous cycle and pregnancy in the rat. Chronobiol Int. 2018;35(8):1077–87. https://doi.org/10.1080/07420528.2018.1458035.
Gaskill BN, Gordon CJ, Pajor EA, Lucas JR, Davis JK, Garner JP. Impact of nesting material on mouse body temperature and physiology. Physiol Behav. 2013;110–111:87–95. doi:https://doi.org/10.1016/j.physbeh.2012.12.018.
Nagashima K, Nakai S, Konishi M, Su L, Kanosue K. Increased heat-escape/cold-seeking behavior following hypertonic saline injection in rats. Am J Phys Regul Integr Comp Phys. 2001;280(4):R1031–6. https://doi.org/10.1152/ajpregu.2001.280.4.R1031.
Westerterp KR. Diet induced thermogenesis. Nutr Metab (Lond). 2004;1(1):5. https://doi.org/10.1186/1743-7075-1-5.
Gordon CJ. The mouse thermoregulatory system: its impact on translating biomedical data to humans. Physiol Behav. 2017;179:55–66. https://doi.org/10.1016/j.physbeh.2017.05.026.
Coan PM, Ferguson-Smith AC, Burton GJ. Developmental dynamics of the definitive mouse placenta assessed by stereology. Biol Reprod. 2004;70(6):1806–13.
Wyrwoll CS, Seckl JR, Holmes MC. Altered placental function of 11beta-hydroxysteroid dehydrogenase 2 knockout mice. Endocrinology. 2009;150(3):1287–93. https://doi.org/10.1210/en.2008-1100.
Yamauchi C, Fujita S, Obara T, Ueda T. Effects of room temperature on reproduction, body and organ weights, food and water intakes, and hematology in mice. Jikken Dobutsu. 1983;32(1):1–11.
Acknowledgments
The authors give many thanks to the staff in the Cell Central and Animal Care Services at the School of Human Sciences, University of Western Australia, for their assistance with this project.
Funding
The study was funded by a Raine BrightSpark grant awarded to GP, CW, and SM.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The Animal Ethics Committee of the University of Western Australia approved all procedures associated with this study (RA/3/100/1509).
Conflict of Interest
The authors declare that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(PDF 24 kb)
Rights and permissions
About this article
Cite this article
Olivier, K., Reinders, L.A., Clarke, M.W. et al. Maternal, Placental, and Fetal Responses to Intermittent Heat Exposure During Late Gestation in Mice. Reprod. Sci. 28, 416–425 (2021). https://doi.org/10.1007/s43032-020-00291-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-020-00291-7