Abstract
Purpose
This study aimed to measure the effects of the upper or lower limit of the carbon dioxide (CO2) insufflation pressure applied in children who underwent laparoscopic and thoracoscopic interventions, on the changes in the brain and kidney Near Infrared Spectrometry (NIRS) values.
Patients and Methods
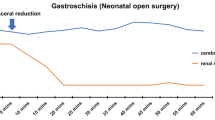
Demographic information, carbon dioxide insufflation pressure and the operation time data were recorded. During the procedure the NIRS probes monitored the brain and left kidney during laparoscopic procedures and the brain only during thoracoscopic procedures. Basal NIRS values were recorded after anesthesia induction, after CO2 insufflation-beginning of insufflation, near the end of the procedure-end of insufflation, and after carbon dioxide desufflation. During the procedure, when ≥20% decrease was observed in the basal value during carbon dioxide insufflation, the carbon dioxide pressure was decreased and the procedure was continued. In case of a decrease of ≥50% in either brain or kidney NIRS it was planned to be recorded as an absolute decrease, and to terminate laparoscopy or thoracoscopy.
Results
Two hundred four laparoscopic and 19 thoracoscopic cases were included in the study. The mean age of the patients undergoing laparoscopic procedures was 120 months, the mean body weight was 33 kg, and the mean operative time was 43 minutes; whereas the mean age of the patients undergoing thoracoscopic procedures was 62 months, the mean body weight was 17 kg, and the mean operative time was 80 minutes. No statistically significant difference was found in NIRS values between upper or lower insufflation pressures (p>0.05).
Conclusion
The pressures provided at the upper limit of the safe range may expand the surgical area and can help prevent problems that may be encountered due to the limited space during the surgery. In this study, it has been shown that pressures at the upper limit of the safe range do not impair patient brain and kidney oxygenation.
Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Aziz O, Athanasiou T, Tekkis PP, Purkayastha S, Haddow J, Malinovski V, Paraskeva P, Darzi A (2006) Laparoscopic versus open appendectomy in children: a meta-analysis. Ann Surg 243:17–27. https://doi.org/10.1097/01.sla.0000193602.74417.14
Esposito C, Calvo AI, Castagnetti M, Alicchio F, Suarez C, Giurin I, Settimi A (2012) Open versus laparoscopic appendectomy in the pediatric population: a literature review and analysis of complications. J Laparoendosc Adv Surg Tech A 22:834–839. https://doi.org/10.1089/lap.2011.0492.
Sauerland S, Lefering R, Neugebauer EA (2002) Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev CD001546. https://doi.org/10.1002/14651858.CD001546
Laberge JM, Blair GK (2013) Thoracotomy for repair of esophageal atresia: not as bad as they want you to think! Dis Esophagus 26:365–371. https://doi.org/10.1111/dote.12053.
Wiesenthal JD, Fazio LM, Perks AE, Blew BD, Mazer D, Hare G, Honey RJ, Pace KT (2011) Effect of pneumoperitoneum on renal tissue oxygenation and blood flow in a rat model. Urology 77:1508.e9–15. https://doi.org/10.1016/j.urology.2011.02.022.
Bliss D, Matar M, Krishnaswami S (2009) Should intraoperative hypercapnea or hypercarbia raise concern in neonates undergoing thoracoscopic repair of diaphragmatic hernia of Bochdalek? J Laparo Endosc Adv Surg Tech A 19(Suppl 1):S55–S58. https://doi.org/10.1089/lap.2008.0141.supp
Wahr JA, Tremper KK, Samra S, Delpy DT (1996) Near-infrared spectroscopy: theory and applications. J Cardiothorac Vasc Anesth 10(3):406–418. https://doi.org/10.1016/s1053-0770(96)80107-8.
Tuna AT, Akkoyun I, Darcin S, Palabiyik O (2016) Effects of carbon dioxide insufflation on regional cerebral oxygenation during laparoscopic surgery in children: a prospective study. Braz J Anesthesiol 66(3):249–253. https://doi.org/10.1016/j.bjane.2014.10.004
Demyttenaere S, Feldman LS, Fried GM (2007) Effect of pneumoperitoneum on renal perfusion and function: a systematic review. Surg Endosc 21(2):152–160. https://doi.org/10.1007/s00464-006-0250-x.
Gipson CL, Johnson GA, Fisher R, Stewart A, Giles G, Johnson JO, Tobias JD (2006) Changes in cerebral oximetry during peritoneal insufflation for laparoscopic procedures. J Minim Access Surg 2(2):67–72. https://doi.org/10.4103/0972-9941.26651
Bishay M, Giacomello L, Retrosi G, Thyoka M, Nah SA, McHoney M, De Coppi P, Brierley J, Scuplak S, Kiely EM, Curry JI, Drake DP, Cross KM, Eaton S, Pierro A (2011) Decreased cerebral oxygen saturation during thoracoscopic repair of congenital diaphragmatic hernia and esophageal atresia in infants. J Pediatr Surg 46(1):47–51. https://doi.org/10.1016/j.jpedsurg.2010.09.062.
Krosnar S, Baxter A (2005) Thoracoscopic repair of esophageal atresia with tracheoesophageal fistula: anesthetic and intensive care management of a series of eight neonates. Paediatr Anaesth 15(7):541–546. https://doi.org/10.1111/j.1460-9592.2005.01594.x.
McHoney M, Giacomello L, Nah SA, De Coppi P, Kiely EM, Curry JI, Drake DP, Eaton S, Pierro A (2010) Thoracoscopic repair of congenital diaphragmatic hernia: intraoperative ventilation and recurrence. J Pediatr Surg 45(2):355–359. https://doi.org/10.1016/j.jpedsurg.2009.10.072.
Armaly Z, Abassi Z (2014) Deleteriousefects of increased intraabdominal pressure on kidney function. Adv Nephrol 2014:1–15 https://doi.org/10.1155/2014/731657
Çalışkan E, ŞanalBaş S, Onay M, Kılıç Y, KayhanErdoğan G, Tokar B (2020) Evaluation of renal oxygenization in laparoscopic pediatric surgery by near infrared spectroscopy. Pediatr Surg Int 36(9):1077–1086. https://doi.org/10.1007/s00383-020-04709-w.
Ruf B, Bonelli V, Balling G, Hörer J, Nagdyman N, Braun SL, Ewert P, Reiter K (2015) Intraoperative renal near-infrared spectroscopy indicates developing acute kidney injury in infants undergoing cardiac surgery with cardiopulmonary bypass: a case-control study. Crit Care 19(1):27. https://doi.org/10.1186/s13054-015-0760-9
Joffe R, Al Aklabi M, Bhattacharya S, Cave D, Calleja T, Garros D, Majesic N, Ryerson L, Morgan C (2018) Cardiac surgery-associated kidney injury in children and renal oximetry. Pediatr Crit Care Med 19(9):839–845. https://doi.org/10.1097/PCC.0000000000001656.
Westgarth-Taylor C, de Lijster L, van Bogerijen G, Millar AJ, Karpelowsky J (2013) A prospective assessment of renal oxygenation in children undergoing laparoscopy using near-infrared spectroscopy. Surg Endosc 27(10):3696–3704. https://doi.org/10.1007/s00464-013-2950-3.
Beck J, Loron G, Masson C, Poli-Merol ML, Guyot E, Guillot C, Bednarek N, François C (2017) Monitoring cerebral and renal oxygenation status during neonatal digestive surgeries using near infrared spectroscopy. Front Pediatr 14(5):140. https://doi.org/10.1186/s13054-015-0760-9
Franzini S, Morandi A, Palmisani F, Consonni D, Macchini F, Calderini E, Leva E (2021) Cerebral oxygenation by near-infrared spectroscopy in infants undergoing Thoracoscopic lung resection. J Laparoendosc Adv Surg Tech A 31(9):1084–1091. https://doi.org/10.1089/lap.2021.0177.
Costerus S, Vlot J, van Rosmalen J, Wijnen R, Weber F (2019) Effects of neonatal thoracoscopic surgery on tissue oxygenation: a pilot study on (neuro-) monitoring and outcomes. Eur J Pediatr Surg 29(2):166–172. https://doi.org/10.1055/s-0037-1615277.
Velde EAT, Bax NMA, Tytgat SHAJ, de Jong JR, Travassos DV, Kramer WLM, van der Zee DC (2008) Minimally invasive pediatric surgery: Increasing implementation in daily practice and resident’s training. Surg Endosc 22(1):163–166. https://doi.org/10.1007/s00464-007-9395-5
Allal H, Pérez-Bertólez S, Maillet O, Forgues D, Doan Q, Chiapinelli A, Kong V (2009) Estudio comparativo de toracoscopia versus toracotomía en atresia esofágica [Comparative study of thoracoscopy versus thoracotomy in esophageal atresia]. Cir Pediatr 22(4):177–180
Szavay PO, Zundel S, Blumenstock G, Kirschner HJ, Luithle T, Girisch M, Luenig H, Fuchs J (2011) Perioperative outcome of patients with esophageal atresia and tracheo-esophageal fistula undergoing open versus thoracoscopic surgery. J Laparoendosc Adv Surg Tech A 21(5):439–443. https://doi.org/10.1089/lap.2010.0349.
Rothenberg SS (2009) Experience with thoracoscopic tracheal surgery in infants and children. J Laparoendosc Adv Surg Tech A 19(5):671–674. https://doi.org/10.1089/lap.2009.0083.
Bishay M, Giacomello L, Retrosi G et al (2013) Hypercapnia and acidosis during open and thoracoscopic repair of congenital diaphragmatic hernia and esophageal atresia: results of a pilot randomized controlled trial. Ann Surg 258(6):895–900. https://doi.org/10.1097/sla.0b013e31828fab55.
Stolwijk LJ, Tytgat SH, Keunen K, Suksamanapan N, vanHerwaarden MY, Groenendaal F, Lemmers PM, van der Zee DC (2015) The effects of CO2-insufflation with 5 and 10 mmHg during thoracoscopy on cerebral oxygenation and hemodynamics in piglets: an animal experimental study. Surg Endosc 29(9):2781–2788. https://doi.org/10.1007/s00464-014-4009-5.
Funding
No financial assistance was received to support this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical permission
Ethical committee of the University granted permission for this study No:17B0230005.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ergun, E., Gollu, G., Gurbanov, A. et al. Evaluation of oxygenation of brain and kidneys with NIRS (near infrared spectrometry) technique in laparoscopic and thoracoscopic operations in children and determination of safe limits of carbon dioxide insufflation. J Ped Endosc Surg 5, 55–61 (2023). https://doi.org/10.1007/s42804-023-00171-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42804-023-00171-2