Key summary points
We propose a scoping review on psychomotor disadaptation syndrome. We performed a search for epidemiological studies on this subject.
AbstractSection FindingsPsychomotor disadaptation syndrome has not yet been the focus of an epidemiological study and is poorly known, especially outside of France. Post-fall syndrome is the best known and most studied aspect of psychomotor disadaptation syndrome.
AbstractSection MessageRaising awareness among medical or paramedical geriatrics professionals about psychomotor disadaptation syndrome is necessary, especially because the number of frail older adults who exhibit this syndrome will continue to increase.
Abstract
Background
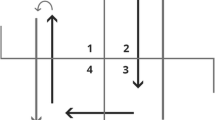
Clinical features of psychomotor disadaptation syndrome (PDS) include posture, gait, psycho-behavioral, and neurological disorders, which increase the risk of falling. Psychomotor regression syndrome, described in 1986, was renamed PDS following improvements in its pathophysiological understanding, including the preeminent role of subcortical-frontal lesions. Because frailty in aging contributes to the appearance of PDS, the geriatric professionals need to be aware of its existence.
Purpose
This article aims to provide a scoping review on PDS. Moreover, we searched for epidemiological studies and assessed whether or not all the aspects of PDS are recognized.
Methods
The studies were retrieved from three electronic databases (PubMed, Science Direct, and Google Scholar) using these terms: psychomotor disadaptation syndrome, psychomotor regression syndrome, frontal-sub-cortical dysfunction syndrome, backward disequilibrium, retropulsion, post-fall syndrome, reactional hypertonia, axial akinesia, and older adults.
Results
Out of 456 shortlisted articles, 45 met the inclusion criteria. Our results show that PDS is poorly known, especially outside of France, which had the largest number of published studies on this syndrome. Abroad, only three aspects have been described (post-fall syndrome, retropulsion, and fear of falling). Often, they are not recognized as belonging to a real syndrome, but rather an association of signs. Post-fall syndrome, found in 14 studies, is the best known and most studied aspect of PDS. There were no epidemiological studies.
Conclusion
With the increasing number of frail older adults, there will be an inevitable growth in the incidence of PDS. Raising awareness about PDS among medical and paramedical geriatrics professionals is essential.


Similar content being viewed by others
Data availability
The datasets reported in this review are publicly available.
References
Lepage S, Gillain S, Petermans J (2012) Le syndrome de désadaptation psychomotrice (SDPM): une entité clinique encore méconnue. Rev Med Liege 67:75–80
Mourey F, Manckoundia P, Martin-Arveux I, Tavernier-Vidal B, Pfitzenmeyer P (2004) Psychomotor disadaptation syndrome A new clinical entity in geriatric patients. Geriatrics 59:20–24
Manckoundia P, Mourey F (2020) Syndrome de désadaptation psychomotrice. Rev Med Liege 75:180–184
Manckoundia P, Mourey F (2021) Description du syndrome de désadaptation psychomotrice. Soins Gerontol 26:34–36
Pfitzenmeyer P, Martin-Hunyadi C, Mourey F, d’Athis P, Baudouin N, Mischis-Troussard C (2002) Cardiovascular characteristics and cerebral CT findings in elderly subjects with psychomotor disadaptation syndrome. Aging Clin Exp Res 14:100–107
Manckoundia P, Mourey F (2019) Psychomotor disadaptation syndrome. Neurol Rehabil 25:33–36
Bouchon J-P (1984) 1 + 2 + 3 ou comment tenter d’être efficace en gériatrie ? Rev Prat 34:888–892
Murphy J, Isaacs B (1982) The post-fall syndrome. Gerontology 28:265–270
Manckoundia P, Mourey F, Tavernier-Vidal B, Pfitzenmeyer P (2007) Syndrome de désadaptation psychomotrice. Rev Med Interne 28:79–85
Mourey F, Camus A, d’Athis P, Blanchon MA, Martin-Hunyadi C, de Rekeneire N et al (2005) Mini motor test: a clinical test for rehabilitation of patients showing psychomotor disadaptation syndrome (PDS). Arch Gerontol Geriatr 40:201–211
Berlot R, Pavlović A, Kojović M (2024) Secondary parkinsonism associated with focal brain lesions. Front Neurol 15:1438885
Verghese J, Wang C, Lipton R, Holtzer R (2013) Motoric cognitive risk syndrome and the risk of dementia. J Gerontol A Biol Sci Med Sci 68:412–418
Tournier-Lasserve E, Iba-Zizen MT, Romero N, Bousser MG (1991) Autosomal dominant syndrome with strokelike episodes and leukoencephalopathy. Stroke 22:1297–1302
Mourad A, Levasseur M, Bousser MG, Chabriat H (2006) Formes pauci symptomatiques de CADASIL après 60 ans. Rev Neurol (Paris) 162:827–831
Chabriat H, Vahedi K, Iba-Zizen MT, Joutel A, Nibbio A, Nagy TG et al (1995) Clinical spectrum of CADASIL: a study of 7 families. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Lancet 346:934–939
Manckoundia P, Gerbault N, Mourey F, d’Athis P, Nourdin C, Monin MP et al (2007) Multidisciplinary management in geriatric day-hospital is beneficial for elderly fallers: a prospective study of 28 cases. Arch Gerontol Geriatr 44:61–70
Ageing Europe-statistics on population developments. Eurostat statistics explained. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Ageing_Europe_-_statistics_on_population_developments. Accessed 20 Nov 2024.
Pfitzenmeyer P, Mourey F, Tavernier B, Camus A (1999) Psychomotor desadaptation syndrome. Arch Gerontol Geriatr 28:217–225
Pfitzenmeyer P, Mourey F, Manckoundia P, Tavernier-Vidal B (2003) La désadaptation psychomotrice. Rev Geriatr 28:597–600
Manckoundia P, Ntari Soungui E, Tavernier-Vidal B, Mourey F (2014) Syndrome de désadaptation psychomotrice. Geriatr Psychol Neuropsychiatr Vieil 12:94–100
Pfitzenmeyer P, Mourey F, Manckoundia P, d’Athis P (2005) A 4-year follow-up of very old patients presenting with frontal-subcortical dysfunction compared with Alzheimer’s disease patients. Gerontology 51:62–65
Rapp K, Becker C, Cameron ID, Konig HH, Buchele G (2012) Epidemiology of falls in residential aged care: analysis of more than 70,000 falls from residents of Bavarian nursing homes. J Am Med Dir Assoc 13:187.e1–6
Kramer D, Allgaier AK, Fejtkova S, Mergl R, Hegerl U (2009) Depression in nursing homes: prevalence, recognition, and treatment. Int J Psychiatry Med 39:345–358
Komici K, Guerra G, Addona F, Fantini C (2022) Delirium in nursing home residents: a narrative review. Healthcare (Basel) 10:1544
Jerez-Roig J, Farrés-Godayol P, Yildirim M, Escribà-Salvans A, Moreno-Martin P, Goutan-Roura E et al (2024) Prevalence of urinary incontinence and associated factors in nursing homes: a multicentre cross-sectional study. BMC Geriatr 24:169
Vanderwee K, Clays E, Bocquaert I, Gobert M, Folens B, Defloor T (2010) Malnutrition and associated factors in elderly hospital patients: a Belgian cross-sectional, multi-centre study. Clin Nutr 29:469–476
Williams AT, Bates-Jensen BM, Hodge F, Lee E, Levy-Storms L (2024) Pressure injury pain over time among nursing home residents. Geriatr Nurs 59:362–371
Bouchmal S, Goërtz YMJ, Hacking C, Winkens B, Aarts S (2024) The relation between resident-related factors and care problems in nursing homes: a multi-level analysis. BMC Health Serv Res 24:1435
Reilev M, Lundby C, Jensen J, Larsen SP, Hoffmann H, Pottegård A (2019) Morbidity and mortality among older people admitted to nursing home. Age Ageing 49:67–73
Atramont A, Rigault A, Chevalier S, Leblanc G, Fagot-Campagna A, Tuppin P (2017) Caractéristiques, pathologies et mortalité des résidents en établissements d’hébergement pour personnes âgées dépendantes (Ehpad) admis au cours du premier trimestre 2013 en France. Rev Epidemiol Sante Publique 65:221–230
Morisod J, Coutaz M (2007) Le syndrome post-chute : comment le reconnaitre et le traiter. Rev Med Suisse 3:2531–2536
Debette S, Schilling S, Duperron MG, Larsson SC, Markus HS (2019) Clinical significance of magnetic resonance imaging markers of vascular brain injury: a systematic review and Meta -analysis. JAMA Neurol 76:81–94
Zheng JJ, Delbaere K, Close JC, Sachdev PS, Lord SR (2011) Impact of white matter lesions on physical functioning and fall risk in older people: a systematic review. Stroke 42:2086–2090
Su C, Yang X, Wei S, Zhao R (2022) Association of cerebral small vessel disease with gait and balance disorders. Front Aging Neurosci 14:834496
Mourey F, Brondel L, Van Wymelbeke V, Buchheit M, Moreau D, Pfitzenmeyer P (2009) Assessment of cardiac autonomic nervous activity in frail elderly people with postural abnormalities and in control subjects. Arch Gerontol Geriatr 48:121–124
Manckoundia P, Pérennou D, Pfitzenmeyer P, Mourey F (2007) La rétropulsion du sujet âgé : mise au point sur un symptôme grave et proposition d’une échelle pour une évaluation quantifiée. Rev Med Interne 28:242–249
Manckoundia P, Mourey F, Pérennou D, Pfitzenmeyer P (2008) Backward disequilibrium in elderly subjects. Clin Interv Aging 3:667–672
Scheets PL, Sahrmann SA, Norton BJ, Stith JS, Crowner BE (2015) What is backward disequilibrium and how do I treat it? J Neurol Phys Ther 39:119–126
Bergmann J, Krewer C, Müller F, Jahn K (2022) The scale for retropulsion: internal consistency, reliability and construct validity. Ann Phys Rehabil Med 65:101537
Matheron E, Dubost V, Mourey F, Pfitzenmeyer P, Manckoundia P (2010) Analysis of postural control in elderly subjects suffering from Psychomotor disadaptation syndrome (PDS). Arch Gerontol Geriatr 51:19–23
Brondel L, Mourey F, Mischis-Troussard C, d’Athis P, Pfitzenmeyer P (2005) Energy cost and cardiorespiratory adaptation in the “get-up-and-go” test in frail elderly women with postural abnormalities and in controls. J Gerontol A Biol Sci Med Sci 60:98–103
Alarcón T, González-Montalvo JI, Otero Puime Á (2009) Evaluación de los pacientes con miedo a caídas? El método empleado modifica los resultados? Una revisión sistemática. Aten Primaria 41:262–268
Wu SYF, Brown T, Yu M (2020) Older adults’ psychosocial responses to a fear of falling: a scoping review to inform occupational therapy practice. Occup Ther Ment Health 36:207–243
Jung D (2008) Fear of falling in older adults: comprehensive review. Asian Nurs Res 2:214–222
Uemura K, Yamada M, Nagai K, Tanaka B, Mori S, Ichihashi N (2012) Fear of falling is associated with prolonged anticipatory postural adjustment during gait initiation under dual-task conditions in older adults. Gait Posture 35:282–286
Legters K (2002) Fear of falling. Phys Ther 82:264–272
Mourey F, Manckoundia P, Pfitzenmeyer P (2009) La peur de tomber et ses conséquences : mise au point. Cah Annee Gerontol 1:102–108
Gaxatte C, Nguyen T, Chourabi F, Salleron J, Pardessus V, Delabrière I et al (2011) Fear of falling as seen in the multidisciplinary falls consultation. Ann Phys Rehabil Med 54:248–258
Benhamou J, Espejo T, Riedel HB, Dreher-Hummel T, García-Martínez A, Gubler-Gut B et al (2024) On-site physiotherapy in older emergency department patients following a fall: a randomized controlled trial. Eur Geriatr Med (in press)
Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C (2005) Development and initial validation of the falls efficacy scale-international (FES-I). Age Ageing 34:614–619
Kempen G, Yardley L, van Haastregt JCM, Zijlstra GA, Beyer N, Hauer K et al (2008) The Short FES-I: a shortened version of the falls efficacy scale-International to assess fear of falling. Age Ageing 37:45–50
Suzuki T, Kim H, Yoshida H, Ishizaki T (2004) Randomized controlled trial of exercise intervention for the prevention of falls in community-dwelling elderly Japanese women. J Bone Miner Metab 22:602–611
Kechaou I, Cherif E, Sana BS, Boukhris I, Hassine LB (2019) Complications traumatiques et psychosociales des chutes chez le sujet âgé tunisien. Pan Afr Med J 32:92
Fromage B (2005) Représentation de soi chez des sujets âgés chuteurs et non chuteurs. Encephale 31:601–608
Bloch F (2015) Les complications non traumatiques des chutes : des conséquences trop souvent négligées chez la personne âgée. Neurol Psychiatr Geriatr 15:188–190
Gonthier R (2014) Epidémiologie, morbidité, mortalité, coût pour la société et pour l’individu, principales causes de la chute. Bull Acad Natle Med 198:1025–1039
Sellier C (2017) Bilan à réaliser devant un patient chuteur. Soins Gerontol 22:12–15
Gaudin AC, Moumneh T, Rivière H, Roy PM, Annweiler C, Brangier A (2019) Prise en charge et orientation des patients gériatriques consultant aux urgences pour une chute : résultats de l’étude de cohorte OREGoN. Geriatr Psychol Neuropsychiatr Vieil 17:254–260
Meyer M, Constancias F, Vogel T, Kaltenbach G, Schmitt E (2020) Gait disorder among elderly people, psychomotor disadaptation syndrome: post-fall syndrome, risk factors and follow-up—a cohort study of 70 patients. Gerontology 67:17–24
Miró Ò, Brizzi BN, Aguiló S, Alemany X, Jacob J, Llorens P et al (2019) 180-Day functional decline among older patients attending an emergency department after a fall. Maturitas 129:50–56
Pfitzenmeyer P, Mourey F, Mischis-Troussard C, Bonneval P (2001) Rehabilitation of serious postural insufficiency after falling in very elderly subjects. Arch Gerontol Geriatr 33:211–218
Bloch F, Rigaud AS, Kemoun G (2013) Virtual Reality Exposure Therapy in posttraumatic stress disorder: a brief review to open new opportunities for post-fall syndrome in elderly subjects. Eur Geriatr Med 4:427–430
Marivan K, Boully C, Benveniste S, Reingewirtz S, Rigaud AS, Kemoun G et al (2016) Rehabilitation of the psychomotor consequences of falling in an elderly population: a pilot study to evaluate feasibility and tolerability of virtual reality training. J Health Care Technol 24:169–175
Rmadi H, Mary M, Duron E, Pujol T, Gasmi Y, Maillot P et al (2020) Acceptabilité et tolérance de la thérapie d’exposition à la réalité virtuelle dans la prise en charge du syndrome de désadaptation psychomotrice du sujet âgé. Neurol Psychiatr Geriatr 20:38–46
Piau A, Krams T, Voisin T, Lepage B, Nourhashemi F (2019) Use of a robotic walking aid in rehabilitation to reduce fear of falling is feasible and acceptable from the end user’s perspective: a randomised comparative study. Maturitas 120:40–46
Cremer G, Schoevaerdts D, de Saint-Hubert M, Jamart J, Poulain G, Toussaint É et al (2012) Élaboration d’un test de dépistage du syndrome de désadaptation psychomotrice : le Get-up early test. Geriatr Psychol Neuropsychiatr Vieil 10:165–173
Santos-Pontelli TEG, Pontes-Neto OM, Leite JP (2011) ‘Posterior pusher syndrome’ or ‘psychomotor disadaptation syndrome’? Clin Neurol Neurosurg 113:520–521
Acknowledgements
The authors are grateful to Mrs. Suzanne Rankin, a native English speaker, for editing and proofreading this article.
Funding
This research did not receive any funding.
Author information
Authors and Affiliations
Contributions
AM and PM performed article selection based on title and abstract against predefined inclusion criteria, and if an article was deemed potentially relevant, they assessed the full text on study eligibility. AM and PM wrote the manuscript. All authors made critical revisions and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors report no conflict of interests as concerns this article.
Ethical approval
For this review, no ethical approval is required.
Informed consent
For this study, no informed consent is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Merendino, A., Mourey, F., Renoncourt, T. et al. Psychomotor disadaptation syndrome: a scoping review. Eur Geriatr Med (2025). https://doi.org/10.1007/s41999-025-01176-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41999-025-01176-1