Key summary points
External validation of the clinical frailty scale (CFS) classification tree by determining the agreement and predictive value of the CFS when attributed by a senior geriatrician, a junior geriatrician, or using the classification tree.
AbstractSection FindingsThe CFS classification tree demonstrates moderate agreement with the senior geriatrician CFS and has predictive value for 6-month mortality in patients admitted to an acute geriatric unit.
AbstractSection MessageThese findings suggest that the classification tree can help standardize CFS scoring, thereby improving reliability when used by less-experienced raters.
Abstract
Purpose
Our objective was to perform an external validity study of the clinical frailty scale (CFS) classification tree by determining the agreement of the CFS when attributed by a senior geriatrician, a junior geriatrician, or using the classification tree. Additionally, we evaluated the predictive value of the CFS for 6-month mortality after admission to an acute geriatric unit.
Methods
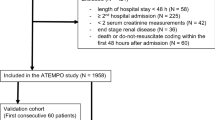
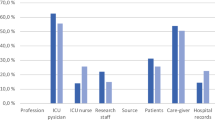
This prospective study was conducted in two acute geriatric units in Belgium. The premorbid CFS was determined by a senior and a junior geriatrician based on clinical judgment within the first 72 h of admission. Another junior geriatrician, who did not have a treatment relationship with the patient, scored the CFS using the classification tree. Intra-class correlation coefficient (ICC) was calculated to assess agreement. A ROC curve and Cox regression model determined prognostic value.
Results
In total, 97 patients were included (mean age 86 ± 5.2; 66% female). Agreement of the CFS, when determined by the senior geriatrician and the classification tree, was moderate (ICC 0.526, 95% CI [0.366–0.656]). This is similar to the agreement between the senior and junior geriatricians’ CFS (ICC 0.643, 95% CI [0.510–0.746]). The AUC for 6-month mortality based on the CFS by respectively the classification tree, the senior and junior geriatrician was 0.719, 95% CI [0.592–0.846]; 0.774, 95% CI [0.673–0.875]; 0.774, 95% CI [0.665–0.882]. Cox regression analysis indicated that severe or very severe frailty was associated with a higher risk of mortality compared to mild or moderate frailty (hazard ratio respectively 6.274, 95% CI [2.613–15.062] by the classification tree; 3.476, 95% CI [1.531–7.888] by the senior geriatrician; 4.851, 95% CI [1.891–12.442] by the junior geriatrician).
Conclusion
Interrater agreement in CFS scoring on clinical judgment without Comprehensive Geriatric Assessment is moderate. The CFS classification tree can help standardize CFS scoring.


Similar content being viewed by others
Data availability
All data relevant to the study can be attained through reasonable request from the corresponding author (Ruth.Piers@uzgent.be).
References
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381(9868):752–762
Falk Erhag H, Guðnadóttir G, Alfredsson J, Cederholm T, Ekerstad N, Religa D et al (2023) The association between the Clinical Frailty Scale and adverse health outcomes in older adults in acute clinical settings—a systematic review of the literature. Clin Interv Aging 18:249–261
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP (2019) Frailty: implications for clinical practice and public health. Lancet 394(10206):1365–1375
Church S, Rogers E, Rockwood K, Theou O (2020) A scoping review of the Clinical Frailty Scale. BMC Geriatr 20(1):393
Bruno RR, Wernly B, Bagshaw SM, van den Boogaard M, Darvall JN, De Geer L et al (2023) The Clinical Frailty Scale for mortality prediction of old acutely admitted intensive care patients: a meta-analysis of individual patient-level data. Ann Intensive Care 13(1):37
Gordon EH, Hubbard RE (2022) Frailty: understanding the difference between age and ageing. Age Ageing 51(8):afac185
Shrier W, Dewar C, Parrella P, Hunt D, Hodgson LE (2021) Agreement and predictive value of the Rockwood Clinical Frailty Scale at emergency department triage. Emerg Med J 38(12):868–873
Theou O, Squires E, Mallery K, Lee JS, Fay S, Goldstein J et al (2018) What do we know about frailty in the acute care setting? A scoping review. BMC Geriatr 18(1):139
Montero-Odasso M, Hogan DB, Lam R, Madden K, MacKnight C, Molnar F et al (2020) Age alone is not adequate to determine health-care resource allocation during the COVID-19 pandemic. Can Geriatr J 23(1):152–154
Lewis EG, Breckons M, Lee RP, Dotchin C, Walker R (2021) Rationing care by frailty during the COVID-19 pandemic. Age Ageing 50(1):7–10
Piers R, Janssens W, Cobbaert K, Pattyn I, Westhovens I, Martens H et al (2021) Letter to the Editor: Premorbid frailty is a better prognostic indicator than age in oldest-old hospitalized with COVID-19. J Am Med Dir Assoc 22(3):514–516
Dou Q, Wang W, Wang H, Ma Y, Hai S, Lin X et al (2019) Prognostic value of frailty in elderly patients with acute coronary syndrome: a systematic review and meta-analysis. BMC Geriatr 19(1):222
Yan B, Sun W, Wang W, Wu J, Wang G, Dou Q (2022) Prognostic significance of frailty in older patients with hip fracture: a systematic review and meta-analysis. Int Orthop 46(12):2939–2952
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I et al (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173(5):489–495
Kaeppeli T, Rueegg M, Dreher-Hummel T, Brabrand M, Kabell-Nissen S, Carpenter CR et al (2020) Validation of the Clinical Frailty Scale for prediction of thirty-day mortality in the emergency department. Ann Emerg Med 76(3):291–300
Surkan M, Rajabali N, Bagshaw SM, Wang X, Rolfson D (2020) Interrater reliability of the Clinical Frailty Scale by geriatrician and intensivist in patients admitted to the intensive care unit. Can Geriatr J 23(3):235–241
Pugh RJ, Battle CE, Thorpe C, Lynch C, Williams JP, Campbell A et al (2019) Reliability of frailty assessment in the critically ill: a multicentre prospective observational study. Anaesthesia 74(6):758–764
Theou O, Pérez-Zepeda MU, van der Valk AM, Searle SD, Howlett SE, Rockwood K (2021) A classification tree to assist with routine scoring of the Clinical Frailty Scale. Age Ageing 50(4):1406–1411
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163
Fronczek J, Polok K, de Lange DW, Jung C, Beil M, Rhodes A et al (2021) Relationship between the Clinical Frailty Scale and short-term mortality in patients ≥ 80 years old acutely admitted to the ICU: a prospective cohort study. Crit Care 25(1):231
Darvall JN, Bellomo R, Bailey M, Paul E, Young PJ, Rockwood K et al (2020) Frailty and outcomes from pneumonia in critical illness: a population-based cohort study. Br J Anaesth 125(5):730–738
Rottler M, Ocskay K, Sipos Z, Görbe A, Virág M, Hegyi P et al (2022) Clinical Frailty Scale (CFS) indicated frailty is associated with increased in-hospital and 30-day mortality in COVID-19 patients: a systematic review and meta-analysis. Ann Intensive Care 12(1):17
Acknowledgements
We would like to acknowledge Soetkin De Raedt, Marie De Groote, Han Martens, and Raf Van Hoeyweghen for their contribution in patient recruitment and data collection.
Author information
Authors and Affiliations
Contributions
Study concept and design were developed by Olga Theou and Ruth Piers. Liese Lanckmans conducted material preparation and data collection. Data analysis and interpretation were performed by Liese Lanckmans, Ruth Piers, and Nele Van Den Noortgate. Liese Lanckmans drafted the initial manuscript, and all authors provided feedback on previous versions. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethics approval
The study protocol was approved by the Ghent University Hospital Ethical Committee (reference number THE-2023-0187). The study was performed in accordance with the Declaration of Helsinki.
Consent
Before enrollment, all included patients or their legal representative provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lanckmans, L., Theou, O., Van Den Noortgate, N. et al. Agreement and predictive value of the clinical frailty scale in hospitalized older patients. Eur Geriatr Med 15, 1339–1345 (2024). https://doi.org/10.1007/s41999-024-01026-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-024-01026-6