Key summary points
We investigated the effectiveness of a self-monitoring intervention to promote step count and reduce sedentary behavior in older people covered by the long-term care insurance system (LTCI) in Japan.
AbstractSection FindingsResults from a randomized controlled trial of a self-monitoring intervention using accelerometers with a 5-week follow-up: improvement in a number of steps, light physical activity, and sedentary behavior in the intervention group compared to the control group.
AbstractSection MessageSelf-monitoring with an accelerometer may be effective in increasing the number of steps taken and amount of light physical activity per day and in reducing sedentary behavior in older people with LTCI.
Abstract
Purpose
This study aimed to investigate the effects of a self-monitoring intervention to promote an increase in physical activity, as measured by step count, and reduce sedentary behavior in older people covered by the long-term care insurance system (LTCI) in Japan.
Methods
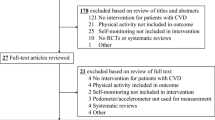
This was a randomized controlled trial conducted at a daycare center from October 2022 to January 2023. Fifty-two older adults with LTCI who were able to walk with or without aids were assigned to an intervention (n = 26) group and control (n = 26) group. During the 5-week follow-up period, the intervention group received education on physical activity and self-monitoring such as goal setting, self-management and feedback. The primary outcome was step count, and the secondary outcome was sedentary behavior.
Results
Participants who completed the study to the end of the 5-week follow-up and drop-out participants for whom outcome data were available were included in the final analysis of 57 participants, n = 24 (79.8 ± 8.8 years, male 25.5%) in the intervention group and n = 23 (82.5 ± 8.5 years, male 39.1%) in the control group. Comparisons between the two groups at baseline showed no significant differences. In the results of a two-way mixed analysis of variance (ANOVA) including 2 (group: control, intervention) × 2 (term: baseline, 5-week follow-up) factors, an interaction was observed in the number of steps, sedentary behavior, and light physical activity (p < 0.05).
Conclusion
Self-monitoring of physical activity using an accelerometer may be effective in increasing the number of steps and light physical activity and in reducing sedentary behavior in older people with LTCI.
Clinical trial registration: UMIN000052044, registered on 2023/08/29.


Similar content being viewed by others
Data availability
The data used in the research is highly confidential, so it is difficult to make it public.
References
Ministry of Health, Labour and Welfare. Long-term care insurance system of Japan (2016) https://www.mhlw.go.jp/english/policy/care-welfare/care-welfare-elderly/dl/ltcisj_e.pdf. Accessed 8 Sep 2023
Yamada M, Arai H (2020) Long-term care system in Japan. Ann Geriatr Med Res 24:174–180. https://doi.org/10.4235/agmr.20.0037
Sato J, Mitsutake N, Kitsuregawa M, Ishikawa T, Goda K (2022) Predicting demand for long-term care using Japanese healthcare insurance claims data. Environ Health Prev Med 27:42. https://doi.org/10.1265/ehpm.22-00084
Patel AV, Hildebrand JS, Leach CR, Campbell PT, Doyle C, Shuval K et al (2018) Walking in relation to mortality in a large prospective cohort of older US adults. Am J Prev Med 54(1):10–19
Xu C, Furuya-Kanamori L, Liu Y, Færch K, Aadahl M, Seguin RA et al (2019) Sedentary behavior, physical activity, and all-cause mortality: dose-response and intensity weighted time-use meta-analysis. J Am Med Dir Assoc 20:1206-1212.e3
Banach M, Lewek J, Surma S (2023) The association between daily step count and all-cause and cardiovascular mortality: a meta-analysis. Eur J Prev Cardiol 9:zwad229
Rietz M, Lehr A, Mino E, Lang A, Szczerba E, Schiemann T et al (2022) Physical activity and risk of major diabetes-related complications in individuals with diabetes: a systematic review and meta-analysis of observational studies. Diabetes Care 45:3101–3111. https://doi.org/10.2337/dc22-0886
Pescatello LS, Buchner DM, Jakicic JM, Powell KE, Kraus WE, Bloodgood B et al (2019) Physical activity to prevent and treat hypertension: a systematic review. Med Sci Sports Exerc 51(6):1314–1323. https://doi.org/10.1249/MSS.0000000000001943
White DK, Jakiela J, Bye T, Aily J, Voinier D (2023) Stepping forward: a scoping review of physical activity in osteoarthritis. J Rheumatol 50(5):611–616
Saunders DH, Mead GE, Fitzsimons C, Kelly P, van Wijck F, Verschuren O (2021) Interventions for reducing sedentary behaviour in people with stroke. Cochrane Database Syst Rev 6:CD012996
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G et al (2020) World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 54(24):1451–1462. https://doi.org/10.1136/bjsports-2020-102955
Fiorilli G, Buonsenso A, Centorbi M, Calcagno G, Iuliano E, Angiolillo A et al (2022) Long term physical activity improves quality of life perception, healthy nutrition, and daily life management in elderly: a randomized controlled trial. Nutrients 14(12):2527. https://doi.org/10.3390/nu14122527
Kitamura M, Izawa KP, Ishihara K, Matsuda H, Okamura S, Fujioka K (2021) Physical activity and sarcopenia in community-dwelling older adults with long-term care insurance. Eur J Investig Health Psychol Educ 11(4):1610–1618. https://doi.org/10.3390/ejihpe11040114
Watanabe Y, Yamada Y, Yoshida T, Yokoyama K, Miyake M, Yamagata E et al (2020) Comprehensive geriatric intervention in community-dwelling older adults: a cluster-randomized controlled trial. J Cachexia Sarcopenia Muscle 11(1):26–37. https://doi.org/10.1002/jcsm.12504
Fletcher JS, Banasik JL (2001) Exercise self-efficacy. Clin Excell Nurse Pract 5(3):134–143. https://doi.org/10.1054/xc.2001.24203
Bandura A (1982) Self-efficacy mechanism in human agency. Am Psychol 37:122–147
Kerr J, Rosenberg D, Millstein RA, Bolling K, Crist K, Takemoto M et al (2018) Cluster randomized controlled trial of a multilevel physical activity intervention for older adults. Int J Behav Nutr Phys Act 15(1):32. https://doi.org/10.1186/s12966-018-0658-4
Kanai M, Izawa KP, Kobayashi M, Onishi A, Kubo H, Nozoe M et al (2018) Effect of accelerometer-based feedback on physical activity in hospitalized patients with ischemic stroke: a randomized controlled trial. Clin Rehabil 32(8):1047–1056. https://doi.org/10.1177/0269215518755841
Izawa KP, Watanabe S, Omiya K, Hirano Y, Oka K, Osada N et al (2005) Effect of the self-monitoring approach on exercise maintenance during cardiac rehabilitation: a randomized, controlled trial. Am J Phys Med Rehabil 84(5):313–321. https://doi.org/10.1097/01.phm.0000156901.95289.09
Izawa KP, Watanabe S, Hiraki K, Morio Y, Kasahara Y, Takeichi N et al (2012) Determination of the effectiveness of accelerometer use in the promotion of physical activity in cardiac patients: a randomized controlled trial. Arch Phys Med Rehabil 93(11):1896–1902. https://doi.org/10.1016/j.apmr.2012.06.015
Ayabe M, Brubaker PH, Mori Y, Kumahara H, Kiyonaga A, Tanaka H et al (2010) Self-monitoring moderate-vigorous physical activity versus steps/day is more effective in chronic disease exercise programs. J Cardiopulm Rehabil Prev 30(2):111–115. https://doi.org/10.1097/HCR.0b013e3181be7c80
Bai Y, Burns R, Gell N, Byun W (2022) A randomized trial to promote physical activity in adult pre-hypertensive and hypertensive patients. J Sports Sci 40(14):1648–1657. https://doi.org/10.1080/02640414.2022.2099179
Boutron I, Altman DG, Moher D, Schulz KF, Ravaud P, CONSORT NPT Group (2017) CONSORT Statement for randomized trials of nonpharmacologic treatments: a 2017 update and a CONSORT extension for nonpharmacologic trial abstracts. Ann Intern Med 167(1):40–47
Mitchell AJ (2009) A meta-analysis of the accuracy of the Mini-Mental State Examination in the detection of dementia and mild cognitive impairment. J Psychiatr Res 43(4):411–431. https://doi.org/10.1016/j.jpsychires.2008.04.014
Ida S, Kaneko R, Murata K (2018) SARC-F for screening of sarcopenia among older adults: a meta-analysis of screening test accuracy. J Am Med Dir Assoc 19:685–689. https://doi.org/10.1016/j.jamda.2018.04.001
Nagasaki H, Itoh H, Furuna T (1995) The structure underlying physical performance measures for older adults in the community. Aging (Milano) 7(6):451–458. https://doi.org/10.1007/BF03324360
Tanaka M, Ikezoe T, Ichihashi N, Tabara Y, Nakayama T, Takahashi Y et al (2020) Relationship of low muscle mass and obesity with physical function in community dwelling older adults: Results from the Nagahama study. Arch Gerontol Geriatr 88:103987. https://doi.org/10.1016/j.archger.2019.103987
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG et al (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85–M94
Yano S, Koohsari MJ, Shibata A, Ishii K, Frehlich L, McCormack GR et al (2019) Comparison of older and newer generation active style pro accelerometers in physical activity and sedentary behavior surveillance under a free-living environment. Int J Environ Res Public Health 16(9):1597. https://doi.org/10.3390/ijerph16091597
Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE et al (2017) Sedentary behavior research network (SBRN)-terminology consensus project process and outcome. Int J Behav Nutr Phys Act 14(1):75. https://doi.org/10.1186/s12966-017-0525-8
Owen N, Healy GN, Matthews CE, Dunstan DW (2010) Too much sitting: the population-health science of sedentary behavior. Exerc Sport Sci Rev 38:105. https://doi.org/10.1097/JES.0b013e3181e373a2
Ikeda S, Shiroiwa T, Igarashi A, Noto S, Fukuda T, Saito S et al (2015) Developing a Japanese version of the EQ-5D-5L value set. J Natl Inst Public Health 64(1):47–55
Japan Physical Activity Research Platform (2020). http://paplatform.umin.jp (in Japanese). Accessed 8 Sep 2023
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D et al (2011) Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 20(10):1727–1736. https://doi.org/10.1007/s11136-011-9903-x
Kline PW, Melanson EL, Sullivan WJ, Blatchford PJ, Miller MJ, Stevens-Lapsley JE et al (2019) Improving physical activity through adjunct telerehabilitation following total knee arthroplasty: randomized controlled trial protocol. Phys Ther 99(1):37–45. https://doi.org/10.1093/ptj/pzy119
Nolan CM, Maddocks M, Canavan JL, Jones SE, Delogu V, Kaliaraju D et al (2017) Pedometer step count targets during pulmonary rehabilitation in chronic obstructive pulmonary disease. A randomized controlled trial. Am J Respir Crit Care Med 195(10):1344–1352
Bakker EA, van Bakel BMA, Aengevaeren WRM, Meindersma EP, Snoek JA, Waskowsky WM et al (2021) Sedentary behaviour in cardiovascular disease patients: Risk group identification and the impact of cardiac rehabilitation. Int J Cardiol 326:194–201. https://doi.org/10.1016/j.ijcard.2020.11.014
Shinohara H, Mikami Y, Kuroda R, Asaeda M, Kawasaki T, Kouda K et al (2022) Rehabilitation in the long-term care insurance domain: a scoping review. Health Econ Rev 12(1):59. https://doi.org/10.1186/s13561-022-00407-6
Scherr J, Wolfarth B, Christle JW, Pressler A, Wagenpfeil S, Halle M (2013) Associations between Borg’s rating of perceived exertion and physiological measures of exercise intensity. Eur J Appl Physiol 113(1):147–155. https://doi.org/10.1007/s00421-012-2421-x
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum Associates Inc., Hillsdale, NJ, p 13
Goto K, Yamamoto T, Kashiwazaki M, Miura K (2018) Longitudinal changes and characteristics of the number of steps of subjects with different levels of care needs. Rigakuryouhou Kagaku 33(4):623–629. https://doi.org/10.1589/rika.33.623.(inJapanese)
Araki K, Yasunaga A, Shibata A, Hattori K, Honma R, Sato N et al (2022) Cross-sectional associations between replacing sedentary behavior with physical activity by accelerometer-measured and depression in frail older adults: an isotemporal substitution approach. Tairyokukagaku 71(2):185–192. https://doi.org/10.7600/jspfsm.71.185.(inJapanese)
Ishigaki T, Takahama Y, Nakamoto T, Ogawa T (2023) Clustering the sedentary behavior of elderly requiring care at home and the characteristics of functioning: an attempt by using sedentary behavior bout. Tiikirigakuryouhougaku 1:7–17. https://doi.org/10.57351/jjccpt.1.0_7.(inJapanese)
Chastin S, Gardiner PA, Harvey JA, Leask CF, Jerez-Roig J, Rosenberg D et al (2021) Interventions for reducing sedentary behaviour in community-dwelling older adults. Cochrane Database Syst Rev 25:CD012784
Ashizawa R, Honda H, Take K, Yoshizawa K, Kameyama Y, Yoshimoto Y (2023) Effects on sedentary behaviour of an approach to reduce sedentary behaviour in patients with minor ischaemic stroke: a randomised controlled trial. Clin Rehabil 37(4):545–556. https://doi.org/10.1177/02692155221135412
Kirk AF, Barnett J, Mutrie N (2007) Physical activity consultation for people with type 2 diabetes: evidence and guidelines. Diabet Med 24:809–816
Saunders DH, Mead GE, Fitzsimons C, Kelly P, van Wijck F, Verschuren O et al (2021) Interventions for reducing sedentary behaviour in people with stroke. Cochrane Database Syst Rev 6:CD012996
Swartz AM, Cho CC, Welch WA, Widlansky ME, Maeda H, Strath SJ (2018) Pattern analysis of sedentary behavior change after a walking intervention. Am J Health Behav 42(3):90–101. https://doi.org/10.5993/AJHB.42.3.9
Giné-Garriga M, Sansano-Nadal O, Tully MA, Caserotti P, Coll-Planas L, Rothenbacher D et al (2020) Accelerometer-measured sedentary and physical activity time and their correlates in European older adults: the SITLESS study. J Gerontol A Biol Sci Med Sci 75(9):1754–1762. https://doi.org/10.1093/gerona/glaa016. (PMID: 31943000)
Awick EA, Ehlers DK, Aguiñaga S, Daugherty AM, Kramer AF, McAuley E (2017) Effects of a randomized exercise trial on physical activity, psychological distress and quality of life in older adults. Gen Hosp Psychiatry 49:44–50. https://doi.org/10.1016/j.genhosppsych.2017.06.005
Nagai K, Miyamato T, Okamae A, Tamaki A, Fujioka H, Wada Y et al (2018) Physical activity combined with resistance training reduces symptoms of frailty in older adults: a randomized controlled trial. Arch Gerontol Geriatr 76:41–47. https://doi.org/10.1016/j.archger.2018.02.005
Pedersen MT, Vorup J, Nistrup A, Wikman JM, Alstrøm JM, Melcher PS et al (2017) Effect of team sports and resistance training on physical function, quality of life, and motivation in older adults. Scand J Med Sci Sports 27(8):852–864. https://doi.org/10.1111/sms.12823
Nicholas SO, Giang AT, Yap PLK (2019) The effectiveness of horticultural therapy on older adults: a systematic review. J Am Med Dir Assoc 20(10):1351.e1-1351.e11. https://doi.org/10.1016/j.jamda.2019.06.021
Rowiński R, Morgulec-Adamowicz N, Ogonowska-Slodownik A, Dąbrowski A, Geigle PR (2017) Participation in leisure activities and tourism among older people with and without disabilities in Poland. Arch Gerontol Geriatr 73:82–88. https://doi.org/10.1016/j.archger.2017.07.025
Acknowledgements
This study was benefitted by the support and encouragement of Masashi Kanai, Masato Ogawa, Asami Ogura, Ikkou Kubo, Kodai Ishihara, Yuji Kanejima, Ryo Yoshihara, and Ayami Osumi, all of Kobe University Graduate School of Health Sciences, and Shinichi Noto of Niigata University of Health and Welfare. We would also like to thank the participants and staff at Rifuru Yukuhashi Daycare Center for their cooperation in this study.
Funding
This work was supported by JSPS KAKENHI Grant Numbers JP22K11392 and JP23K16629 and Reiwa Health Sciences University, University Support Research Fund 2022.
Author information
Authors and Affiliations
Contributions
Conceptualization, MK, KPI, TN, TY, SO, KF, WY, and HM; methodology, MK and KPI; protocol development, obtaining ethical approval and formal analysis. MK; participant recruitment and investigation, KF and WY; writing—original draft preparation, MK; writing—review and editing, MK, KPI, TN, TY, SO, KF, WY, and HM; resources and funding acquisition, MK and KPI; supervision, KPI All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The Authors declare that there is no conflict of interest.
Ethics approval
The study protocol was approved by the Reiwa Health Sciences University Research Ethics Committee (approval number: 22–008). The study complied with the guidelines of the Declaration of Helsinki, and written informed consent was obtained from all participants.
Informed consent
Written informed consent was obtained from each participant in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kitamura, M., Izawa, K.P., Nagasaki, T. et al. Effects of self-monitoring using an accelerometer on physical activity of older people with long-term care insurance in Japan: a randomized controlled trial. Eur Geriatr Med 15, 371–380 (2024). https://doi.org/10.1007/s41999-024-00935-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-024-00935-w