Abstract
Introduction
Previous studies in 2018 and 2022 have suggested increasing inpatient burden of pneumothorax and widespread variation in management. Local trends have never been elucidated. Northumbria Healthcare NHS Foundation Trust (NHCT) has a well-established pleural service, serving just over 600,000. Thus, we set up a local retrospective study to look at trends in pneumothorax presentation, management strategies, length of stay, and recurrence.
Methods
A coding search for ‘pneumothorax’ was performed for all patients attending NHCT between 2010 and 2020 was performed with local Caldicott approval. A total of 1840 notes were analysed to exclude iatrogenic, traumatic, and paediatric events. After excluding those cases, 580 remained for further analysis, consisting of 183 primary pneumothoraces (PSP) and 397 secondary pneumothoraces (SSP).
Results
Median age for PSP was 26.5 years (IQR 17) with 69% male, and for SSP 68 years (IQR 11.5), 62% male; 23.5% of PSP and 8.6% of SSP were never smokers. The proportion of smokers and ex-smokers has not really changed over time: > 65% every year have been smokers or ex-smokers. Yearly pneumothorax incidence shows a downward trend for PSP but upwards for SSP. Median length of stay (LoS) for PSP was 2 days (IQR 2), and SSP 5 days (IQR 8), with a clear downward trend. From 2010 to 2015 > 50% PSP were managed with drain, but in 2019–2020 at least 50% managed conservatively, with a significant reduction in aspiration. Trends of recurrence for PSP are increasing, whereas for SSP is decreasing. Seventy-six (20 PSP, 56 SSP) went for surgery at the index time with 5.3% recurrence (20% recurrence in those without surgery).
Conclusions
This is the first known analysis of pneumothorax trends in a large trust in the northeast of England. The data in this study have certain limitations, including the lack of information on the size of pneumothorax and frailty indicators that may influence the decision for conservative management. Additionally, there is a reliance on clinical coding, which can introduce potential inaccuracies, and not all patient notes were accessible for analysis. Updated larger datasets should help elucidate trends better.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
There has been no previous assessment of pneumothorax presentation and management trends in our pleural centre. Anecdotally, conservative management and length of stay have been decreasing. |
This retrospective cohort study asked if local pneumothorax patients were similar to the single previously described cohort and if there was increasing conservative management with decreasing length of stay. |
What was learned from the study? |
Local patients with pneumothorax are older than previously described cohorts in the United Kingdom and length of stay is decreasing with increasing conservative management. |
These are observational data and pave the way for formal research into conservative versus interventional research into both primary and secondary spontaneous pneumothorax. |
Introduction
Pneumothorax, defined as air in the pleural space, was first described by the French physician Jean Marc Gaspard Itard (1774–1838) in his thesis ‘Dissertation sur le pneumo-thorax ou les congestions gazeuses qui déforment dans la poitrine’ in 1803 [1]. He was a student of Rene Laennec who then described pneumothorax in greater detail in 1819 [2]. Kjaergaard in 1932 described the first cohort of primary spontaneous pneumothorax in young people [3] and since then there have been multiple studies describing various forms of pneumothorax (primary—without apparent lung disease, secondary—with lung disease, or in those over 50 years of age with significant smoking history, traumatic or iatrogenic) [4]. The most relevant study regarding the epidemiology of primary spontaneous (PSP) and secondary spontaneous pneumothorax (SSP) in the United Kingdom (UK) is from Halifax et al., where just under 171,000 hospital admissions from 1968 to 2016 were investigated [5]. The median age of patients was 44 years [interquartile range (IQR) 26–88] and 73% of the patients were male. There was a bimodal age distribution, initially at 15–34 years and then after 60 years of age. The chance of recurrence within 5 years was similar between males and females but there was variation by age group and presence of chronic lung disease. As expected, the presence of chronic lung disease increased the chance of recurrence. There have also been multiple, very heterogenous studies looking at the management strategies relating to the various types of pneumothorax, with a recent focus on more conservative approaches [6, 7].
As far as we know, no further studies looking at pneumothorax epidemiology in the UK have been performed. We work in a well-established pleural disease centre catering to a population of just over 600,000 [8]. Acute care is concentrated in a new purpose-built unit that receives all admissions and was opened in 2015. This has 24/7 respiratory consultant (and pleural) cover [9]. Anecdotally, we observed a decrease in the number of pneumothoraces among our inpatient service, an increased utilisation of conservative management approaches, and a reduction in the length of hospital stay for these cases. Thus, we set up a local retrospective study to examine trends in pneumothorax presentation, management strategies, length of stay, as well as recurrence.
Methods
The study was registered as a service audit with the Audit department of Northumbria Healthcare NHS Foundation Trust (NHCT) (Reference 8276) and local ethical (Caldicott) approval was granted by the Information Governance department (Reference C3737). Informed consent was not required due to the retrospective nature of this study. A case record form was developed, and the authors tried to collect multiple data points such as age, sex, length of stay, height, weight, body mass index, type of pneumothorax, smoking (cigarette and cannabis) status, family history of pneumothorax, final causative diagnosis, management strategy, and recurrence. All inpatient care records between 1 January 2010 and 31 December 2020 coded for pneumothorax were retrieved using electronic searches by the NHCT coding department and then manually searched to exclude traumatic, iatrogenic, and paediatric cases.
All analyses were performed using Microsoft Excel 365 within Office 365. Continuous variables are presented as mean (± standard deviation) if normally distributed, or with median and IQRs, and categorical variables as percentages where appropriate. Descriptive methods are used.
This study was performed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement and abides by the principles of the Declaration of Helsinki [10, 11].
Results
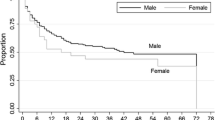
A total of 1840 records were initially obtained from the search and manually screened to apply the above exclusion criteria. Then, 580 records with PSP or SSP were analysed. There were 183 PSP and 397 SSP. Due to missing data in over 90% of the records related to cannabis smoking status, height, weight, body mass index, and family history of pneumothorax, we are unable to report any findings for these variables. The median age for the whole cohort was 56.5 years (IQR 44.5, range, 17–90), for PSP was 27 years (IQR 17) and 70 years (IQR 11.5) for SSP. Figure 1 shows the trends in average age of presentation of SSP and PSP. There was a male preponderance in each group (127, 69% males in PSP and 247, 62% in SSP—these lower numbers reflecting the fact that some recurred and were only counted once.
In the PSP group, cigarette smoking status was unknown in 42 patients (23%). Forty-three patients (23.5%) were never smokers, 79 (43.2%) were current cigarette smokers, and 19 (10.3%) were smokers. In the SSP group, there were no data for 48 (12%) patients. One hundred and five (26.5%) were current smokers, 210 (53%) were ex-smokers, and 34 (8.5%) were non-smokers.
The pneumothorax incidence per year shows an upward trend for SSP, but a downward trend for PSP, except for rises in the year 2017 and 2015, respectively. Of note, three people recurred in the 2015 PSPs (accounting for seven out of 34 events in total, i.e., four excess) and nine recurred in the 2017 SSPs (accounting for 17 of 52 events in total, i.e., eight excess). This is depicted in Fig. 2.
There is a clear downward trend in the number of inpatient days for both SSP and PSP from 2010 to 2020. This is depicted in Fig. 3.
With regards to management, there was an increasing trend towards conservative management for both PSP and SSP. Figures 4 and 5 in the supplementary material show length of stay by management strategy, showing a trend that an insertion of a chest drain is associated with longer length of stay for PSP. Table 1 shows that overall, 43 out of 183 PSP were managed conservatively (23.5%), 34 had a needle aspirate (18.6%), and 106 patients had an intercostal drain insertion (65%) as initial management.
Twenty-one had surgery at the time of their PSP for prolonged air leaks. Of the 43 initially managed conservatively, one went on to have a drain insertion (2.3%). Of the 34 managed with needle aspiration, 12 went on to have an intercostal drain insertion (35.3%). Of the SSPs, 94 were managed conservatively (five went on to have an intercostal drain insertion [5.4%]), ten had a needle aspirate (six of which went on to have a drain insertion [60%]) and 293 had an intercostal drain as first line treatment. Figures 6 and 7 (supplementary material) show the trends of type of management over time, showing a clear increase in conservative management of PSP over the years, with a near total reduction in the use of needle aspiration and less use of intercostal drains. In the SSP group, there is a similar trend towards conservative management, but intercostal drain use has remained quite high.
Figure 8 (supplementary material) shows the trends of recurrence of PSP by year and management trends juxtaposed, and the linear trend would suggest a general increasing signal of recurrence, although some years such as 2018 had none. The recurrence rate was highest in the last 2 years and in those managed with an intercostal drain, but the numbers are small. Figure 9 (supplementary material) shows the trend of recurrence of SSP by year with management trends juxtaposed as well, and the linear trend would suggest reducing recurrence rates. Overall, 106 (18.3%) out of 580 episodes were determined as recurring—31 primary and 75 secondaries; 12/31 (38.7%) of PSP and 54/75 SSP (72%) recurring within the first 3 months (Fig. 10—supplementary material). Of those that recurred, 84 (79.2%) were in current or ex-smokers and 12 (11.3%) non-smokers. We only recorded those who went for surgery at the time of their inpatient episode, and those were 21 PSP (11.5% total PSPs) and 49 SSP (12.3% total SSPs); 12/21 (57.1%) of the PSP were their first episodes and this compared to 31/49 (63.3%) for SSP. Of those who needed surgery with primary spontaneous pneumothorax, six of 21 (28.6%) had a known current or ex smoking label; with secondary spontaneous pneumothorax this was 44 of 49 (89.8%). There was 5.3% recurrence in those who went for surgery compared to a 20% recurrence in those who did not have surgery.
Discussion
This is the first retrospective cohort study in pneumothorax performed from a local hospital in the UK and has some interesting trends that we will now discuss.
The median age of our population is much older than the data presented by Hallifax et al. (56 years versus 44 years), and the male preponderance is still there at 74% in our cohort [12]. This is reflected in the subnational population projections for England: 2018-based statistics, where the northern regions have a greater burden of ageing than other regions in the UK [13]. The tobacco smoking rates in the northeast of England are also much higher than the rest of the UK, which would explain our much higher rates of SSP.
Smoking is the main risk factor for the development of pneumothorax and this evidence has been known for many decades [14]. A very large proportion of the PSP in this cohort were current or ex-smokers. By definition, a PSP is the presence of pneumothorax in someone without known lung disease, but that definition has been challenged over time as there are clear pathological changes in smokers’ lung which might not be totally clinically apparent [15]. As such, it is worth wondering if PSP is truly without lung disease in those smokers and whether the definition should be changed. The upcoming British Thoracic Society Pleural Disease guidelines make a note that ‘This distinction does not imply that patients with PSP have normal underlying lung parenchyma, with the majority demonstrating emphysema-like pulmonary changes on CT imaging, but instead reflects that current management and outcomes differ between the two patient groups.’
There has been some evidence published recently that conservative management might be an option for management of PSP and SSP, although this is not a new concept altogether. Stradling et al. in 1966 described the observational approach to 119 pneumothoraces and 80% of those did not require an intervention and did not require admission [16]. More recently, Brown et al. randomised 316 patients with unilateral significant PSPs to conservative versus interventional management and found that conservative management was probably non-inferior to interventional management at 8 weeks. Those patients also had a shorter length of stay and the patients had less complications. Limitations to the data are the prespecified non-inferiority margins, the missing data at follow-ups, and the very large number of patients screened. Conservative management also showed improvements in 12-month recurrence rates with a small (15%) reintervention rate. Conservative management might also play a role in the management of SSP, but data are from non-randomised, observational studies [17,18,19]. The draft BTS guidance suggests that all modalities (conservative care, needle aspiration, chest drain insertion as well as ambulatory care) have a role to play, according to the patient’s choice and resource availability, that conservative management is likely associated with reduced length of stay and recurrence [4].
The management trends in our cohort of both PSP and SSP are towards increasing conservative management for both with less use of intercostal drains in PSP and much reduced use of needle aspiration. This mirrors the trends in length of stay for both PSP and SSP and is in line with the known literature. Needle aspiration, despite the evidence regarding efficacy, both in PSP and SSP, has anecdotally fallen out in favour locally due to the requirement for further procedures when performed, and the preference to go for an intercostal drain for initial management. This is reflected in the recent survey by Hallifax et al. where for those with minimal symptoms in PSP or SSP, over 50% of responders would opt for conservative management, 35% would then go for an intercostal drain with ongoing symptoms and that for large or symptomatic SSP, an intercostal drain would be the first management strategy [20]. The recurrence rate is more difficult to explain and limited by small numbers preventing meaningful statistical analyses, but observational evidence would suggest that conservative management allows the air leak to heal on its own. This is the trend seen over the last few years with PSP managed by intercostal drainage.
As a single-centre study with a significant amount of missing data points, there are several limitations to the above. Numbers are small overall compared to the study by Hallifax et al., and thus can only inform decisions locally. We are limited by only having data from our centre, and none from the regional centres where patients are referred to for potential surgery, or from anywhere else that patients might have migrated to. We were also reliant on hospital coding to get our original data set and some cases might have been incorrectly coded, thereby also reducing the numbers for final analyses. We also did not collect data on symptoms of the patients, which might have influenced management or on size of the pneumothorax. Interestingly, the latest guideline from the BTS has removed size as a criterion for intervention, as it is known that even large asymptomatic pneumothoraces can be safely observed and resolve over time. We also did not collect data on frailty of the patients, which might also have influenced conservative management and the patients in the more recent years have had shorter follow-up times, which may underestimate recurrence rates.
Another point worth mentioning is that when the acute care centre opened in June 2015, respiratory consultant cover was provided every day of the week, and there is a marked difference between length of stay for patients before 2015 and after 2015, most notably for PSP. Prior to 2015, the median length of inpatient stay for PSP was 3.2 days. From 2015 to end of data this has reduced to 1.1 day. In SSP, a similar effect is seen decreasing from 6.2 days pre-2015 to 4.3 days since. This is perhaps attributable to daily consultant review, thus enabling a faster discharge.
All of the above is purely observational. Future research into pneumothorax is warranted, and the NHCT is participating or considering participation in the Longitudinal Investigation of Secondary Pneumothorax (LISP), Randomised trial of suction for primary pneumothorax early resolution (RASPER), CONservative versus Standard carE for primary spontaneous PneumoThorax (CONSEPT), and Pragmatic non-inferiority Randomised trial Investigating Needle aspiration versus ChEst drain for Secondary Spontaneous Pneumothorax (PRINCE) [21,22,23,24].
Conclusions
Trends for pneumothorax management over a decade in a large pleural centre show a decreasing length of stay and increasing conservative management. This mirrors previously known literature. Future randomised trials, that are all in set up or recruiting, should help understand the presentation and management of pneumothorax further.
References
Itard JM. Dissertation sur le pneumo-thorax ou les congestions gazeuses qui déforment dans la poitrine. Paris: Thesis, 1803 [Google Scholar].
Laennec RT, editor. De l’Auscultation Médiate ou Traité du Diagnostic des Maladies des Poumons et du Coeur. Paris: Brosson & Chaudé, 1819 [Google Scholar].
Kjaergaard H. Spontaneous pneumothorax in the apparently healthy. Acta Med Scand Suppl. 1932;43:1–159 (Google Scholar).
Pleural disease guidelines British Thoracic Society (in draft). https://www.brit-thoracic.org.uk/quality-improvement/guidelines/pleural-disease/. Accessed 29 Mar 2022
Hallifax RJ, Goldacre R, Landray MJ, Rahman NM, Goldacre MJ. Trends in the incidence and recurrence of inpatient-treated spontaneous pneumothorax, 1968–2016. JAMA. 2018;320(14):1471–80. https://doi.org/10.1001/jama.2018.14299.
Nava GW, Walker SP. Management of the secondary spontaneous pneumothorax: current guidance, controversies, and recent advances. J Clin Med. 2022;11:1173. https://doi.org/10.3390/jcm11051173.
Aujayeb A. Spontaneous pneumothorax: new horizons. J Respir. 2021;1:80–3. https://doi.org/10.3390/jor1010008.
Aujayeb A, Parker S, Bourke S, Miller J, Cooper D. A review of a pleural service. J R Coll Physicians Edinb. 2016;46(1):26–31. https://doi.org/10.4997/jrcpe.2016.108.
Aujayeb A. Consolidating malignant pleural and peritoneal services during the COVID-19 response. Future Healthc J. 2020;7(2):161–2. https://doi.org/10.7861/fhj.2020-0016.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;6:344–9. https://doi.org/10.1016/j.jclinepi.2007.11.008.
Carlson RV, Boyd KM, Webb DJ. The revision of the Declaration of Helsinki: past, present and future. Br J Clin Pharmacol. 2004;57:695–713. https://doi.org/10.1111/j.1365-2125.2004.02103.x.
Subnational population projections for England: 2018-based. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/bulletins/subnationalpopulationprojectionsforengland/2018based. Accessed 29 Mar 2022.
Local tobacco control profiles for England: statistical commentary, December 2022 update. https://www.gov.uk/government/statistics/local-tobacco-control-profiles-december-2022-update/local-tobacco-control-profiles-for-england-statistical-commentary-december-2022-update.
Bense L, Eklund G, Wiman LG. Smoking and the increased risk of contracting spontaneous pneumothorax. Chest. 1987;92(6):1009–12. https://doi.org/10.1378/chest.92.6.1009.
Hallifax R. Aetiology of primary spontaneous pneumothorax. J Clin Med. 2022;11:490. https://doi.org/10.3390/jcm11030490.
Stradling P, Poole G. Conservative management of spontaneous pneumothorax. Thorax. 1966;21:145–9.
Brown SGA, Ball EL, Perrin K, Asha SE, Braithwaite I, Egerton-Warburton D, Jones PG, Keijzers G, Kinnear FB, Kwan BCH, et al. Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med. 2020;382:405–15.
Cortes-Telles A, Ortíz-Farias DL, Perez-Hernandez F, Rodriguez-Morejon D. Secondary spontaneous pneumothorax: a time to re-evaluate management. Respirol Case Rep. 2021;9: e00749.
Gerhardy BC, Simpson G. Conservative versus invasive management of secondary spontaneous pneumothorax: A retrospective cohort study. Acute Med Surg. 2021;8: e663.
Hallifax RJ, Roberts M, Russell N, et al. Pneumothorax management: current state of practice in the UK. Respir Res. 2022;23:23. https://doi.org/10.1186/s12931-022-01943-9.
Longitudinal Investigation of Secondary Pneumothorax. https://inspirerespiratory.co.uk/studies/lisp/. Accessed 29 Mar 2022.
A trial of suction for the early resolution of a collapsed lung ISRCTN18017504. https://doi.org/10.1186/ISRCTN18017504. Accessed 4 May 23.
Treating people with a lung collapse (pneumothorax) without inserting a needle into the chest. Is it safe and effective? ISRCTN75384510. https://doi.org/10.1186/ISRCTN75384510.
NIHR204137: Pragmatic non-inferiority Randomised trial Investigating Needle aspiration versus ChEst drain for Secondary Spontaneous Pneumothorax. https://www.nihr.ac.uk/documents/research-for-patient-benefit-competition-45-stage-2-and-competition-46-stage-1-minutes-east-midlands/30368. Accessed 29 Mar 2022.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Author Contributions
Avinash Aujayeb: concept and design, James Hyman, Avinash Aujayeb, Mariko Moffatt, Claire Storey, Umair Falak, Samuel Richardson: data collection, AA and JH: statistical analysis, Avinash Aujayeb and James Hyman drafting the initial manuscript, James Hyman, Avinash Aujayeb, Mariko Moffatt, Claire Storey, Umair Falak, Samuel Richardson revision and approval of final submitted version of manuscript.
Disclosures
James Hyman, Avinash Aujayeb, Mariko Moffatt, Claire Storey, Umair Falak, and Samuel Richardson have nothing to disclose.
Compliance with Ethics Guidelines
The study was registered as a service audit with the Audit department of Northumbria Healthcare NHS Foundation Trust (NHCT) (Reference 8276) and local ethical (Caldicott) approval was granted by the Information Governance department (Reference C3737). Informed consent was not required due to the retrospective nature of this study.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hyman, J., Falak, U., Storey, C. et al. Pneumothorax Trends from 2010–2020 from a Large-Volume Pleural Unit. Pulm Ther 9, 367–375 (2023). https://doi.org/10.1007/s41030-023-00232-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-023-00232-0