Abstract
Purpose of Review
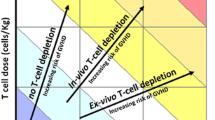
The outcome of allogeneic stem cell transplantation (allo-HCT) is still compromised by relapse and complications. NK cells and γδT cells, effectors that both function through MHC-unrestricted mechanisms, can target transformed and infected cells without inducing graft-versus-host disease (GVHD). Allo-HCT platforms based on CD34+ selection or αβ-TCR depletion result in low grades of GVHD, early immune reconstitution (IR) of NK and γδT cells and minimal usage of GVHD prophylaxis. In this review we will discuss strategies to retain and expand the quantity, diversity, and functionality of these reconstituting innate cell types.
Recent Findings
Bisphosphonates, IL-15 cytokine administration, specific antibodies, checkpoint inhibitors, and (CMV based) vaccination are currently being evaluated to enhance IR. All these approaches have shown to potentially enhance both NK and γδT cell immuno-repertoires.
Summary
Rapidly accumulating data linking innate biology to proposed clinical immune interventions will give unique opportunities to unravel shared pathways which determine the graft-versus-tumor effects of NK and γδT cells.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Baron F, Labopin M, Blaise D, Lopez-Corral L, Vigouroux S, Craddock C, et al. Impact of in vivo T-cell depletion on outcome of AML patients in first CR given peripheral blood stem cells and reduced-intensity conditioning allo-SCT from a HLA-identical sibling donor: a report from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Bone Marrow Transplant. 2014;49(3):389–96. https://doi.org/10.1038/bmt.2013.204.
Zaia J, Baden L, Boeckh MJ, Chakrabarti S, Einsele H, Ljungman P, et al. Viral disease prevention after hematopoietic cell transplantation. Bone Marrow Transplant. 2009;44(8):471–82. https://doi.org/10.1038/bmt.2009.258.
• Luznik L, Bolanos-Meade J, Zahurak M, Chen AR, Smith BD, Brodsky R, et al. High-dose cyclophosphamide as single-agent, short-course prophylaxis of graft-versus-host disease. Blood. 2010;115(16):3224–30. https://doi.org/10.1182/blood-2009-11-251595. First large report of the effectiveness of post transplant cycloplosphamide as GVHD prophylaxis.
• Fuchs EJ. HLA-haploidentical blood or marrow transplantation with high-dose, post-transplantation cyclophosphamide. Bone Marrow Transplant. 2015;50(Suppl 2):S31–6. https://doi.org/10.1038/bmt.2015.92. Large clinical cohorts who received post transplant cyclophosphamide.
Pasquini MC, Devine S, Mendizabal A, Baden LR, Wingard JR, Lazarus HM, et al. Comparative outcomes of donor graft CD34+ selection and immune suppressive therapy as graft-versus-host disease prophylaxis for patients with acute myeloid leukemia in complete remission undergoing HLA-matched sibling allogeneic hematopoietic cell transplantation. J Clin Oncol Off J Am Soc Clin Oncol. 2012;30(26):3194–201. https://doi.org/10.1200/JCO.2012.41.7071.
Maschan M, Shelikhova L, Ilushina M, Kurnikova E, Boyakova E, Balashov D, et al. TCR-alpha/beta and CD19 depletion and treosulfan-based conditioning regimen in unrelated and haploidentical transplantation in children with acute myeloid leukemia. Bone Marrow Transplant. 2016;51(5):668–74. https://doi.org/10.1038/bmt.2015.343.
Bertaina A, Merli P, Rutella S, Pagliara D, Bernardo ME, Masetti R, et al. HLA-haploidentical stem cell transplantation after removal of alphabeta+ T and B cells in children with nonmalignant disorders. Blood. 2014;124(5):822–6. https://doi.org/10.1182/blood-2014-03-563817.
Airoldi I, Bertaina A, Prigione I, Zorzoli A, Pagliara D, Cocco C, et al. gammadelta T-cell reconstitution after HLA-haploidentical hematopoietic transplantation depleted of TCR-alphabeta+/CD19+ lymphocytes. Blood. 2015;125(15):2349–58. https://doi.org/10.1182/blood-2014-09-599423.
Bosch M, Khan FM, Storek J. Immune reconstitution after hematopoietic cell transplantation. Curr Opin Hematol. 2012;19(4):324–35. https://doi.org/10.1097/MOH.0b013e328353bc7d.
Admiraal R, Nierkens S, de Witte MA, Petersen EJ, Fleurke GJ, Verrest L, et al. Association between anti-thymocyte globulin exposure and survival outcomes in adult unrelated haemopoietic cell transplantation: a multicentre, retrospective, pharmacodynamic cohort analysis. Lancet Haematol. 2017;4(4):e183–e91. https://doi.org/10.1016/S2352-3026(17)30029-7.
Hirokawa M, Horiuchi T, Kawabata Y, Kitabayashi A, Miura AB. Reconstitution of gammadelta T cell repertoire diversity after human allogeneic hematopoietic cell transplantation and the role of peripheral expansion of mature T cell population in the graft. Bone Marrow Transplant. 2000;26(2):177–85. https://doi.org/10.1038/sj.bmt.1702478.
Scheper W, Grunder C, Straetemans T, Sebestyen Z, Kuball J. Hunting for clinical translation with innate-like immune cells and their receptors. Leukemia. 2014;28(6):1181–90. https://doi.org/10.1038/leu.2013.378.
Handgretinger R. Negative depletion of CD3(+) and TcRalphabeta(+) T cells. Curr Opin Hematol. 2012;19(6):434–9. https://doi.org/10.1097/MOH.0b013e3283582340.
Lang P, Feuchtinger T, Teltschik HM, Schwinger W, Schlegel P, Pfeiffer M, et al. Improved immune recovery after transplantation of TCRalphabeta/CD19-depleted allografts from haploidentical donors in pediatric patients. Bone Marrow Transplant. 2015;50(Suppl 2):S6–10. https://doi.org/10.1038/bmt.2015.87.
Deniger DC, Moyes JS, Cooper LJ. Clinical applications of gamma delta T cells with multivalent immunity. Front Immunol. 2014;5:636. https://doi.org/10.3389/fimmu.2014.00636.
Childs RW, Carlsten M. Therapeutic approaches to enhance natural killer cell cytotoxicity against cancer: the force awakens. Nat Rev Drug Discov. 2015;14(7):487–98. https://doi.org/10.1038/nrd4506.
Scheper W, Sebestyen Z, Kuball J. Cancer Immunotherapy Using gammadeltaT Cells: Dealing with Diversity. Front Immunol. 2014;5:601. https://doi.org/10.3389/fimmu.2014.00601.
Silva-Santos B, Serre K, Norell H. gammadelta T cells in cancer. Nat Rev Immunol. 2015;15(11):683–91. https://doi.org/10.1038/nri3904.
Morvan MG, Lanier LL. NK cells and cancer: you can teach innate cells new tricks. Nat Rev Cancer. 2016;16(1):7–19. https://doi.org/10.1038/nrc.2015.5.
Vivier E, Tomasello E, Baratin M, Walzer T, Ugolini S. Functions of natural killer cells. Nat Immunol. 2008;9(5):503–10. https://doi.org/10.1038/ni1582.
Orr MT, Lanier LL. Natural killer cell education and tolerance. Cell. 2010;142(6):847–56. https://doi.org/10.1016/j.cell.2010.08.031.
Bottino C, Castriconi R, Pende D, Rivera P, Nanni M, Carnemolla B, et al. Identification of PVR (CD155) and Nectin-2 (CD112) as cell surface ligands for the human DNAM-1 (CD226) activating molecule. J Exp Med. 2003;198(4):557–67. https://doi.org/10.1084/jem.20030788.
Lanier LL. Up on the tightrope: natural killer cell activation and inhibition. Nat Immunol. 2008;9(5):495–502. https://doi.org/10.1038/ni1581.
Thielens A, Vivier E, Romagne F. NK cell MHC class I specific receptors (KIR): from biology to clinical intervention. Curr Opin Immunol. 2012;24(2):239–45. https://doi.org/10.1016/j.coi.2012.01.001.
Ruggeri L, Mancusi A, Capanni M, Martelli MF, Velardi A. Exploitation of alloreactive NK cells in adoptive immunotherapy of cancer. Curr Opin Immunol. 2005;17(2):211–7. https://doi.org/10.1016/j.coi.2005.01.007.
Bjorkstrom NK, Ljunggren HG, Sandberg JK. CD56 negative NK cells: origin, function, and role in chronic viral disease. Trends Immunol. 2010;31(11):401–6. https://doi.org/10.1016/j.it.2010.08.003.
Cannon MJ, Schmid DS, Hyde TB. Review of cytomegalovirus seroprevalence and demographic characteristics associated with infection. Rev Med Virol. 2010;20(4):202–13. https://doi.org/10.1002/rmv.655.
Godfrey DI, Uldrich AP, McCluskey J, Rossjohn J, Moody DB. The burgeoning family of unconventional T cells. Nat Immunol. 2015;16(11):1114–23. https://doi.org/10.1038/ni.3298.
Harly C, Guillaume Y, Nedellec S, Peigne CM, Monkkonen H, Monkkonen J, et al. Key implication of CD277/butyrophilin-3 (BTN3A) in cellular stress sensing by a major human gammadelta T-cell subset. Blood. 2012;120(11):2269–79. https://doi.org/10.1182/blood-2012-05-430470.
• Sebestyen Z, Scheper W, Vyborova A, Gu S, Rychnavska Z, Schiffler M, et al. RhoB Mediates Phosphoantigen Recognition by Vgamma9Vdelta2 T Cell Receptor. Cell Rep. 2016;15(9):1973–85. https://doi.org/10.1016/j.celrep.2016.04.081. Authors provide a mechanism on how vγ9δ2+ T cells can specically target cancer cells. Altered RhoB activity and distribution in tumor cells induces membrane immobility of BTN3A1, the ligand for the vγ9δ2 TCR.
• Cichocki F, Cooley S, Davis Z, DeFor TE, Schlums H, Zhang B, et al. CD56dimCD57+NKG2C+ NK cell expansion is associated with reduced leukemia relapse after reduced intensity HCT. Leukemia. 2016;30(2):456–63. https://doi.org/10.1038/leu.2015.260. In a large clinical cohort CMV induced adaptive NK cells results in reduced relapse rates after allo-HCT.
Green ML, Leisenring WM, Xie H, Walter RB, Mielcarek M, Sandmaier BM, et al. CMV reactivation after allogeneic HCT and relapse risk: evidence for early protection in acute myeloid leukemia. Blood. 2013;122(7):1316–24. https://doi.org/10.1182/blood-2013-02-487074.
Vantourout P, Hayday A. Six-of-the-best: unique contributions of gammadelta T cells to immunology. Nat Rev Immunol. 2013;13(2):88–100. https://doi.org/10.1038/nri3384.
Correia DV, Lopes A, Silva-Santos B. Tumor cell recognition by gammadelta T lymphocytes: T-cell receptor vs. NK-cell receptors. Oncoimmunology. 2013;2(1):e22892. https://doi.org/10.4161/onci.22892.
Hayday AC. Gammadelta T cells and the lymphoid stress-surveillance response. Immunity. 2009;31(2):184–96. https://doi.org/10.1016/j.immuni.2009.08.006.
Sebestyen Z, Scheper W, Vyborova A, Gu S, Rychnavska Z, Schiffler M, et al. RhoB Mediates Phosphoantigen Recognition by Vgamma9Vdelta2 T Cell Receptor. Cell Rep. 2016; https://doi.org/10.1016/j.celrep.2016.04.081.
•• Gentles AJ, Newman AM, Liu CL, Bratman SV, Feng W, Kim D, et al. The prognostic landscape of genes and infiltrating immune cells across human cancers. Nat Med. 2015;21(8):938–45. https://doi.org/10.1038/nm.3909. Comprehensive analysis of tumor infitrating leucocytes, showing that γδT cells present at the tumor site are strongly associated with clinical benificial.
Kunzmann V, Bauer E, Wilhelm M. Gamma/delta T-cell stimulation by pamidronate. N Engl J Med. 1999;340(9):737–8. https://doi.org/10.1056/NEJM199903043400914.
Gober HJ, Kistowska M, Angman L, Jeno P, Mori L, De Libero G. Human T cell receptor gammadelta cells recognize endogenous mevalonate metabolites in tumor cells. J Exp Med. 2003;197(2):163–8.
Mullen PJ, Yu R, Longo J, Archer MC, Penn LZ. The interplay between cell signalling and the mevalonate pathway in cancer. Nat Rev Cancer. 2016;16(11):718–31. https://doi.org/10.1038/nrc.2016.76.
Fisher JP, Heuijerjans J, Yan M, Gustafsson K, Anderson J. gammadelta T cells for cancer immunotherapy: A systematic review of clinical trials. Oncoimmunology. 2014;3(1):e27572. https://doi.org/10.4161/onci.27572.
Xiang Z, Liu Y, Zheng J, Liu M, Lv A, Gao Y, et al. Targeted activation of human Vgamma9Vdelta2-T cells controls epstein-barr virus-induced B cell lymphoproliferative disease. Cancer Cell. 2014;26(4):565–76. https://doi.org/10.1016/j.ccr.2014.07.026.
Dharnidharka VR, Mohanakumar T. New approaches to treating B-cell cancers induced by Epstein-Barr virus. N Engl J Med. 2015;372(6):569–71. https://doi.org/10.1056/NEJMcibr1415117.
McClune BL, Polgreen LE, Burmeister LA, Blaes AH, Mulrooney DA, Burns LJ, et al. Screening, prevention and management of osteoporosis and bone loss in adult and pediatric hematopoietic cell transplant recipients. Bone Marrow Transplant. 2011;46(1):1–9. https://doi.org/10.1038/bmt.2010.198.
Pundole X, Cheema HI, Petitto GS, Lopez-Olivo MA, Suarez-Almazor ME, Lu H. Prevention and treatment of bone loss and fractures in patients undergoing a hematopoietic stem cell transplant: a systematic review and meta-analysis. Bone Marrow Transplant. 2017; https://doi.org/10.1038/bmt.2016.312.
•• Bertaina A, Zorzoli A, Petretto A, Barbarito G, Inglese E, Merli P, et al. Zoledronic acid boosts gammadelta T-cell activity in children receiving alphabeta+ T and CD19+ cell-depleted grafts from an HLA-haplo-identical donor. Oncoimmunology. 2017;6(2):e1216291. https://doi.org/10.1080/2162402X.2016.1216291. This trial shows that ZOL stimulates vδ2+ T cells and to a lesser extend vδ1+ T cells. ZOL treatment may associate with an improved outcome.
Nussbaumer O, Gruenbacher G, Gander H, Thurnher M. DC-like cell-dependent activation of human natural killer cells by the bisphosphonate zoledronic acid is regulated by gammadelta T lymphocytes. Blood. 2011;118(10):2743–51. https://doi.org/10.1182/blood-2011-01-328526.
Maniar A, Zhang X, Lin W, Gastman BR, Pauza CD, Strome SE, et al. Human gammadelta T lymphocytes induce robust NK cell-mediated antitumor cytotoxicity through CD137 engagement. Blood. 2010;116(10):1726–33. https://doi.org/10.1182/blood-2009-07-234211.
• An G, Acharya C, Feng X, Wen K, Zhong M, Zhang L, et al. Osteoclasts promote immune suppressive microenvironment in multiple myeloma: therapeutic implication. Blood. 2016;128(12):1590–603. https://doi.org/10.1182/blood-2016-03-707547. In this report the authors show that osteoclasts in MM contribute to the immunosuppressive microenvironment. Treatment with an anti-CD38 antibody shows hat osteoclastogenesis is impaired and T cell immunity is restored.
Charles JF, Aliprantis AO. Osteoclasts: more than ‘bone eaters’. Trends Mol Med. 2014;20(8):449–59. https://doi.org/10.1016/j.molmed.2014.06.001.
Rosenberg SA, Yang JC, Topalian SL, Schwartzentruber DJ, Weber JS, Parkinson DR, et al. Treatment of 283 consecutive patients with metastatic melanoma or renal cell cancer using high-dose bolus interleukin 2. JAMA. 1994;271(12):907–13.
•• Rosenberg SA. IL-2: the first effective immunotherapy for human cancer. J Immunol. 2014;192(12):5451–8. https://doi.org/10.4049/jimmunol.1490019. Reviews IL-2 as first lymphocyte stimulator.
•• Bachanova V, Cooley S, Defor TE, Verneris MR, Zhang B, McKenna DH, et al. Clearance of acute myeloid leukemia by haploidentical natural killer cells is improved using IL-2 diphtheria toxin fusion protein. Blood. 2014;123(25):3855–63. https://doi.org/10.1182/blood-2013-10-532531. Large cumulative report showing 30-50% remission in advanced AML using lymphodepleting chemotherapy, haploidentical NK cells and IL-2 with or with Treg depletion.
Waldmann TA. The shared and contrasting roles of IL2 and IL15 in the life and death of normal and neoplastic lymphocytes: implications for cancer therapy. Cancer Immunol Res. 2015;3(3):219–27. https://doi.org/10.1158/2326-6066.CIR-15-0009.
Rautela J, Huntington ND. IL-15 signaling in NK cell cancer immunotherapy. Curr Opin Immunol. 2016;44:1–6. https://doi.org/10.1016/j.coi.2016.10.004.
Burkett PR, Koka R, Chien M, Chai S, Boone DL, Ma A. Coordinate expression and trans presentation of interleukin (IL)-15Ralpha and IL-15 supports natural killer cell and memory CD8+ T cell homeostasis. J Exp Med. 2004;200(7):825–34. https://doi.org/10.1084/jem.20041389.
Bergamaschi C, Bear J, Rosati M, Beach RK, Alicea C, Sowder R, et al. Circulating IL-15 exists as heterodimeric complex with soluble IL-15Ralpha in human and mouse serum. Blood. 2012;120(1):e1–8. https://doi.org/10.1182/blood-2011-10-384362.
• Mao Y, van Hoef V, Zhang X, Wennerberg E, Lorent J, Witt K, et al. IL-15 activates mTOR and primes stress-activated gene-expression leading to prolonged anti-tumor capacity of NK cells. Blood. 2016; https://doi.org/10.1182/blood-2016-02-698027. This study shows by gene-expression analysis how IL-15 is superior towards IL-2 in stimulating NK cells and that mTOR is key in the signaling process.
Kennedy MK, Glaccum M, Brown SN, Butz EA, Viney JL, Embers M, et al. Reversible defects in natural killer and memory CD8 T cell lineages in interleukin 15-deficient mice. J Exp Med. 2000;191(5):771–80.
Cairo C, Sagnia B, Cappelli G, Colizzi V, Leke RG, Leke RJ, et al. Human cord blood gammadelta T cells expressing public Vgamma2 chains dominate the response to bisphosphonate plus interleukin-15. Immunology. 2013;138(4):346–60. https://doi.org/10.1111/imm.12039.
Ribot JC, Ribeiro ST, Correia DV, Sousa AE, Silva-Santos B. Human gammadelta thymocytes are functionally immature and differentiate into cytotoxic type 1 effector T cells upon IL-2/IL-15 signaling. J Immunol. 2014;192(5):2237–43. https://doi.org/10.4049/jimmunol.1303119.
Garcia VE, Jullien D, Song M, Uyemura K, Shuai K, Morita CT, et al. IL-15 enhances the response of human gamma delta T cells to nonpeptide [correction of nonpetide] microbial antigens. J Immunol. 1998;160(9):4322–9.
•• Dadi S, Chhangawala S, Whitlock BM, Franklin RA, Luo CT, Oh SA, et al. Cancer Immunosurveillance by Tissue-Resident Innate Lymphoid Cells and Innate-like T Cells. Cell. 2016;164(3):365–77. https://doi.org/10.1016/j.cell.2016.01.002. In a mouse models these authors show that the non circulating lymphocytes are shaped by the tumor microenvironment. IL-15 promotes anti-tumor reactivity of these innate lymphoid cells.
Almeida AR, Correia DV, Fernandes-Platzgummer A, da Silva CL, da Silva MG, Anjos DR, et al. Delta One T Cells for Immunotherapy of Chronic Lymphocytic Leukemia: Clinical-Grade Expansion/Differentiation and Preclinical Proof of Concept. Clin Cancer Res. 2016;22(23):5795–804. https://doi.org/10.1158/1078-0432.CCR-16-0597.
Van Acker HH, Anguille S, Willemen Y, Van den Bergh JM, Berneman ZN, Lion E, et al. Interleukin-15 enhances the proliferation, stimulatory phenotype, and antitumor effector functions of human gamma delta T cells. J Hematol Oncol. 2016;9(1):101. https://doi.org/10.1186/s13045-016-0329-3.
•• Conlon KC, Lugli E, Welles HC, Rosenberg SA, Fojo AT, Morris JC, et al. Redistribution, hyperproliferation, activation of natural killer cells and CD8 T cells, and cytokine production during first-in-human clinical trial of recombinant human interleukin-15 in patients with cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2015;33(1):74–82. https://doi.org/10.1200/JCO.2014.57.3329. In this first clinical trial with recombinant IL-15, the authors show that r-IL15 most strongly promotes NK and γδT cells.
Huntington ND, Legrand N, Alves NL, Jaron B, Weijer K, Plet A, et al. IL-15 trans-presentation promotes human NK cell development and differentiation in vivo. J Exp Med. 2009;206(1):25–34. https://doi.org/10.1084/jem.20082013.
Rubinstein MP, Kovar M, Purton JF, Cho JH, Boyman O, Surh CD, et al. Converting IL-15 to a superagonist by binding to soluble IL-15R{alpha}. Proc Natl Acad Sci U S A. 2006;103(24):9166–71. https://doi.org/10.1073/pnas.0600240103.
Wong HC, Jeng EK, Rhode PR. The IL-15-based superagonist ALT-803 promotes the antigen-independent conversion of memory CD8+ T cells into innate-like effector cells with antitumor activity. Oncoimmunology. 2013;2(11):e26442. https://doi.org/10.4161/onci.26442.
Mortier E, Quemener A, Vusio P, Lorenzen I, Boublik Y, Grotzinger J, et al. Soluble interleukin-15 receptor alpha (IL-15R alpha)-sushi as a selective and potent agonist of IL-15 action through IL-15R beta/gamma. Hyperagonist IL-15 x IL-15R alpha fusion proteins. J Biol Chem. 2006;281(3):1612–9. https://doi.org/10.1074/jbc.M508624200.
Weiner GJ. Rituximab: mechanism of action. Semin Hematol. 2010;47(2):115–23. https://doi.org/10.1053/j.seminhematol.2010.01.011.
Felices M, Lenvik TR, Davis ZB, Miller JS, Vallera DA. Generation of BiKEs and TriKEs to Improve NK Cell-Mediated Targeting of Tumor Cells. Methods Mol Biol. 2016;1441:333–46. https://doi.org/10.1007/978-1-4939-3684-7_28.
Gleason MK, Verneris MR, Todhunter DA, Zhang B, McCullar V, Zhou SX, et al. Bispecific and trispecific killer cell engagers directly activate human NK cells through CD16 signaling and induce cytotoxicity and cytokine production. Mol Cancer Ther. 2012;11(12):2674–84. https://doi.org/10.1158/1535-7163.MCT-12-0692.
Gleason MK, Ross JA, Warlick ED, Lund TC, Verneris MR, Wiernik A, et al. CD16xCD33 bispecific killer cell engager (BiKE) activates NK cells against primary MDS and MDSC CD33+ targets. Blood. 2014;123(19):3016–26. https://doi.org/10.1182/blood-2013-10-533398.
• Vallera DA, Felices M, McElmurry R, McCullar V, Zhou X, Schmohl JU, et al. IL15 Trispecific Killer Engagers (TriKE) Make Natural Killer Cells Specific to CD33+ Targets While Also Inducing Persistence, In Vivo Expansion, and Enhanced Function. Clin Cancer Res. 2016;22(14):3440–50. https://doi.org/10.1158/1078-0432.CCR-15-2710. Here the authors show that adding an IL-15 linker to a CD16-CD33 BiKE creates a TriKE with more robust NK cell mediated anti-leukemia responses.
Gillis C, Gouel-Cheron A, Jonsson F, Bruhns P. Contribution of Human FcgammaRs to Disease with Evidence from Human Polymorphisms and Transgenic Animal Studies. Front Immunol. 2014;5:254. https://doi.org/10.3389/fimmu.2014.00254.
Braakman E, van de Winkel JG, van Krimpen BA, Jansze M, Bolhuis RL. CD16 on human gamma delta T lymphocytes: expression, function, and specificity for mouse IgG isotypes. Cell Immunol. 1992;143(1):97–107.
Schiller CB, Braciak TA, Fenn NC, Seidel UJ, Roskopf CC, Wildenhain S, et al. CD19-specific triplebody SPM-1 engages NK and gammadelta T cells for rapid and efficient lysis of malignant B-lymphoid cells. Oncotarget. 2016. https://doi.org/10.18632/oncotarget.13110.
Seidel UJ, Vogt F, Grosse-Hovest L, Jung G, Handgretinger R, Lang P. gammadelta T Cell-Mediated Antibody-Dependent Cellular Cytotoxicity with CD19 Antibodies Assessed by an Impedance-Based Label-Free Real-Time Cytotoxicity Assay. Front Immunol. 2014;5:618. https://doi.org/10.3389/fimmu.2014.00618.
Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell. 2015;27(4):450–61. https://doi.org/10.1016/j.ccell.2015.03.001.
Guillerey C, Huntington ND, Smyth MJ. Targeting natural killer cells in cancer immunotherapy. Nat Immunol. 2016;17(9):1025–36. https://doi.org/10.1038/ni.3518.
Iwasaki M, Tanaka Y, Kobayashi H, Murata-Hirai K, Miyabe H, Sugie T, et al. Expression and function of PD-1 in human gammadelta T cells that recognize phosphoantigens. Eur J Immunol. 2011;41(2):345–55. https://doi.org/10.1002/eji.201040959.
Wistuba-Hamprecht K, Martens A, Haehnel K, Geukes Foppen M, Yuan J, Postow MA, et al. Proportions of blood-borne Vdelta1+ and Vdelta2+ T-cells are associated with overall survival of melanoma patients treated with ipilimumab. Eur J Cancer. 2016;64:116–26. https://doi.org/10.1016/j.ejca.2016.06.001.
Albring JC, Inselmann S, Sauer T, Schliemann C, Altvater B, Kailayangiri S, et al. PD-1 checkpoint blockade in patients with relapsed AML after allogeneic stem cell transplantation. Bone Marrow Transplant. 2017;52(2):317–20. https://doi.org/10.1038/bmt.2016.274.
Yared JA, Hardy N, Singh Z, Hajj S, Badros AZ, Kocoglu M, et al. Major clinical response to nivolumab in relapsed/refractory Hodgkin lymphoma after allogeneic stem cell transplantation. Bone Marrow Transplant. 2016;51(6):850–2. https://doi.org/10.1038/bmt.2015.346.
Boeckh M, Nichols WG, Papanicolaou G, Rubin R, Wingard JR, Zaia J. Cytomegalovirus in hematopoietic stem cell transplant recipients: Current status, known challenges, and future strategies. Biol Blood Marrow Transplant. 2003;9(9):543–58.
Foley B, Cooley S, Verneris MR, Pitt M, Curtsinger J, Luo X, et al. Cytomegalovirus reactivation after allogeneic transplantation promotes a lasting increase in educated NKG2C+ natural killer cells with potent function. Blood. 2012;119(11):2665–74. https://doi.org/10.1182/blood-2011-10-386995.
•• Schlums H, Cichocki F, Tesi B, Theorell J, Beziat V, Holmes TD, et al. Cytomegalovirus infection drives adaptive epigenetic diversification of NK cells with altered signaling and effector function. Immunity. 2015;42(3):443–56. https://doi.org/10.1016/j.immuni.2015.02.008. Here the authors show that CMV infection induces a epigenetic diversification of adaptive NK cells, parallelling T cell differentiation.
Elmaagacli AH, Steckel NK, Koldehoff M, Hegerfeldt Y, Trenschel R, Ditschkowski M, et al. Early human cytomegalovirus replication after transplantation is associated with a decreased relapse risk: evidence for a putative virus-versus-leukemia effect in acute myeloid leukemia patients. Blood. 2011;118(5):1402–12. https://doi.org/10.1182/blood-2010-08-304121.
Dechanet J, Merville P, Lim A, Retiere C, Pitard V, Lafarge X, et al. Implication of gammadelta T cells in the human immune response to cytomegalovirus. J Clin Invest. 1999;103(10):1437–49. https://doi.org/10.1172/JCI5409.
• Scheper W, van Dorp S, Kersting S, Pietersma F, Lindemans C, Hol S, et al. gammadeltaT cells elicited by CMV reactivation after allo-SCT cross-recognize CMV and leukemia. Leukemia. 2013;27(6):1328–38. https://doi.org/10.1038/leu.2012.374. This report shows cross reactivity of CMV induced vδ1+ T cells with cancer cells.
•• Ravens S, Schultze-Florey C, Raha S, Sandrock I, Drenker M, Oberdorfer L, et al. Human gammadelta T cells are quickly reconstituted after stem-cell transplantation and show adaptive clonal expansion in response to viral infection. Nat Immunol. 2017; https://doi.org/10.1038/ni.3686. This report utilizes NGS to show that γδT cells reconstitute quickly post allo-HCT. CMV reactivation results in adaptive clonal expansion of γδT cells.
Laberko A, Bogoyavlenskaya A, Shelikhova L, Shekhovtsova Z, Balashov D, Voronin K, et al. Risk Factors for and the Clinical Impact of Cytomegalovirus and Epstein-Barr Virus Infections in Pediatric Recipients of TCR Alpha/Beta- and CD19-Depleted Grafts. Biol Blood Marrow Transplant. 2016; https://doi.org/10.1016/j.bbmt.2016.12.635.
Knight A, Madrigal AJ, Grace S, Sivakumaran J, Kottaridis P, Mackinnon S, et al. The role of Vdelta2-negative gammadelta T cells during cytomegalovirus reactivation in recipients of allogeneic stem cell transplantation. Blood. 2010;116(12):2164–72. https://doi.org/10.1182/blood-2010-01-255166.
Pitard V, Roumanes D, Lafarge X, Couzi L, Garrigue I, Lafon ME, et al. Long-term expansion of effector/memory Vdelta2-gammadelta T cells is a specific blood signature of CMV infection. Blood. 2008;112(4):1317–24. https://doi.org/10.1182/blood-2008-01-136713.
Lalor SJ, McLoughlin RM. Memory gammadelta T Cells-Newly Appreciated Protagonists in Infection and Immunity. Trends Immunol. 2016;37(10):690–702. https://doi.org/10.1016/j.it.2016.07.006.
Schleiss MR. Cytomegalovirus vaccines under clinical development. J Virus Erad. 2016;2(4):198–207.
Kharfan-Dabaja MA, Boeckh M, Wilck MB, Langston AA, Chu AH, Wloch MK, et al. A novel therapeutic cytomegalovirus DNA vaccine in allogeneic haemopoietic stem-cell transplantation: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Infect Dis. 2012;12(4):290–9. https://doi.org/10.1016/S1473-3099(11)70344-9.
• Nakamura R, La Rosa C, Longmate J, Drake J, Slape C, Zhou Q, et al. Viraemia, immunogenicity, and survival outcomes of cytomegalovirus chimeric epitope vaccine supplemented with PF03512676 (CMVPepVax) in allogeneic haemopoietic stem-cell transplantation: randomised phase 1b trial. Lancet Haematol. 2016;3(2):e87–98. https://doi.org/10.1016/S2352-3026(15)00246-X. Clinical trial showing that administration of the CMV specific peptide vaccine early after allo-HCT is safe, results in less CMV viremia and improved relape free survival
Schmitt M, Schmitt A, Wiesneth M, Hückelhoven A, Wu Z, Kuball J, et al. Peptide Vaccination Against Cytomegalovirus (CMV) Elicits Immunological and Clinical Responses after Allogeneic Stem Cell Transplantation Even from a CMV Seronegative Donor. San Diego: ASH; 2016.
Goodier MR, Rodriguez-Galan A, Lusa C, Nielsen CM, Darboe A, Moldoveanu AL, et al. Influenza Vaccination Generates Cytokine-Induced Memory-like NK Cells: Impact of Human Cytomegalovirus Infection. J Immunol. 2016;197(1):313–25. https://doi.org/10.4049/jimmunol.1502049.
Rubin LG, Levin MJ, Ljungman P, Davies EG, Avery R, Tomblyn M, et al. 2013 IDSA clinical practice guideline for vaccination of the immunocompromised host. Clinical Infectious Diseases. 2014;58(3):e44–100. https://doi.org/10.1093/cid/cit684.
• Djaoud Z, Guethlein LA, Horowitz A, Azzi T, Nemat-Gorgani N, Olive D, et al. Two alternate strategies for innate immunity to Epstein-Barr virus: One using NK cells and the other NK cells and gammadelta T cells. J Exp Med. 2017; https://doi.org/10.1084/jem.20161017. Here the authors show that EBV infections results in differential NK and γδT cell mediated innate immune responses.
Gale RP, Fuchs EJ. Is there really a specific graft-versus-leukaemia effect? Bone Marrow Transplant. 2016;51(11):1413–5. https://doi.org/10.1038/bmt.2016.183.
Restifo NP, Dudley ME, Rosenberg SA. Adoptive immunotherapy for cancer: harnessing the T cell response. Nat Rev Immunol. 2012;12(4):269–81. https://doi.org/10.1038/nri3191.
Fesnak AD, June CH, Levine BL. Engineered T cells: the promise and challenges of cancer immunotherapy. Nat Rev Cancer. 2016;16(9):566–81. https://doi.org/10.1038/nrc.2016.97.
de Witte MA, Kierkels GJ, Straetemans T, Britten CM, Kuball J. Orchestrating an immune response against cancer with engineered immune cells expressing alphabetaTCRs, CARs, and innate immune receptors: an immunological and regulatory challenge. Cancer Immunol Immunother. 2015;64(7):893–902. https://doi.org/10.1007/s00262-015-1710-8.
Thomas ED, Lochte HL Jr, Cannon JH, Sahler OD, Ferrebee JW. Supralethal whole body irradiation and isologous marrow transplantation in man. J Clin Invest. 1959;38:1709–16. https://doi.org/10.1172/JCI103949.
Singer M, Wang C, Cong L, Marjanovic ND, Kowalczyk MS, Zhang H, et al. A Distinct Gene Module for Dysfunction Uncoupled from Activation in Tumor-Infiltrating T Cells. Cell. 2016;166(6):1500–1511 e9. https://doi.org/10.1016/j.cell.2016.08.052.
• Horowitz A, Strauss-Albee DM, Leipold M, Kubo J, Nemat-Gorgani N, Dogan OC, et al. Genetic and environmental determinants of human NK cell diversity revealed by mass cytometry. Sci Transl Med. 2013;5(208):208ra145. https://doi.org/10.1126/scitranslmed.3006702. First report using CyTOF to perform a more comprehensive analysis of NK cell diversity as compared to classical immuno flow cytometry.
Acknowledgments
Moniek A. de Witte received the following funding: KWF UU 2015-7553. Jeffrey S. Miller received the following funding: NIH/NCI P01 CA65493, NIH/NCI P01 CA111412, NIH/NCI R35 CA197292. Funding for this study was provided by ZonMW 43400003 and VIDI-ZonMW 917.11.337, KWF UU 2010-4669, UU 2013-6426, UU 2014-6790 and UU 2015-7601, Vrienden van het UMCU, AICR 10-0736 & 15-0049 to J.K.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Moniek A. de Witte has no conflict of interest.
Jürgen Kuball is scientific co-founder and CSO of Gadeta BV (www.gadeta.nl) and is a shareholder. He is also an inventor on different patents given to Gadeta via the University Medical Centre Utrecht that deal with γδ TCR, processing strategies, and their ligands. In addition, he has received grants from Novartis and Miltenyi Biotech.
Jeffrey S. Miller is a consultant and scientific advisory for Fate Therapeutics and GT Biopharma. He also is on the scientific advisory board for Celgene. In addition, he has pending patents via the University of Minnesota for Fate Therapeutics and GT Biopharma.
Human and Animal Rights and Informed Consent
This article refers to published studies with both human and animal subjects performed by the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Additional information
This article is part of the Topical Collection on Cellular Therapies: Preclinical and Clinical
Rights and permissions
About this article
Cite this article
de Witte, M.A., Kuball, J. & Miller, J.S. NK Cells and γδT Cells for Relapse Protection after Allogeneic Hematopoietic Cell Transplantation (HCT). Curr Stem Cell Rep 3, 301–311 (2017). https://doi.org/10.1007/s40778-017-0106-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40778-017-0106-4