Opinion statement
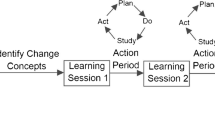
Purpose of review This review summarizes the current need for Quality Improvement Collaboratives (QICs) and includes considerations specific to pediatric healthcare, such as low-frequency of outcomes and unique funding barriers. This review will consider nuances within measure formation and data collection within QICs, available models for structured formation of a QIC, components that are integral to a QICs success, as well as lessons learned and future directions.Recent findings The literature has demonstrated an increase in the number of pediatric QI collaboratives in recent years. These collaboratives have varied in size, duration, and composition of team members. While some QICs have included members at the organizational level, others have included more novel groups such as insurance companies. Novel methodologies have also been utilized such as N of 1 trials focused on continued interventions for one patient and provider dyad. Successful QICs include use of a steering committee or pre-planning group to guide measures development, use of robust QI methodology to implement small tests of change and continuous feedback of individual and aggregate data and transparency among benchmarking sites. Ideal QI methods for use within QICs have been vetted in prior collaboratives and include formal barriers assessments using driver diagrams, PDSA cycles and analyzing data and measures using run and statistical process control (SPC) charts to inform real-time change and interventions.Summary QICs are pivotal to closing the gap in delivery of evidence based practice while minimizing widespread unnecessary practice variation across multiple organizations using available QI methodologies and tools. Novel approaches to funding such as partnership with insurance companies and educational organizations can allow for more robust participation. Future research should broaden the scope of their measures to include patient centered outcomes.


Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Miller MR, Niedner MF, Huskins WC, et al. National Association of Children’s Hospitals and Related Institutions Pediatric Intensive Care Unit Central Line-Associated Bloodstream Infection Quality Transformation Teams. Reducing PICU central line-associated bloodstream infections: 3-year results. Pediatrics. 2011;128(5). Available at: www.pediatrics.org/cgi/content/full/128/5/e1077.
Blumenthal A. The stories behind the stats: NACHRI quality transformation network reaches milestone. Pediatr Nurs. 2011;37(5):276–8. 3. Ohio Children’s Hospitals Solutions for Patient Safety. Available at: http://solutionsforpatientsafety.org/. Accessed 4 April 2013
Watson RS, Carcillo JA, Linde-Zwirble WT, et al. The epidemiology of severe sepsis in children in the United States. Am J Respir Crit Care Med. 2003;167(5):695–701.
Cameron DB, Rangel S. Quality improvement in pediatric surgery. J Curr Opin Pediatr. 2016;28(3):348–55.
Wennberg JE. Dartmouth Atlas of Health Care. Available at: www.dartmouthatlas.org. Practice variation: implications for our health care system. Manag Care. 2004;13(supplement 9):3–7.
Committee on Quality of Health Care in America and the Institute of Medicine, Crossing the Quality Chasm; 2001.
Substance Abuse and Mental Health Services Administration Bulletin; Rockland. 2012. www.Samhsa.gov.
Children’s Hospital Association webpage: www.childrenshospitals.org/About-Us/About-the-Association.
•• Miles PV, Conway PH, Pawlson G. Physician professionalism and accountability: the role of collaborative improvement networks. Pediatrics. 2013;131(Supplement 4):S204–9. This seminal manuscript details how Quality Improvement Collaboratives and Networks can add tremendous value to multiple stakeholders in the healthcare area and postulates strategies to ensure onoing collaborative work.
Institute for Healthcare Improvement. The breakthrough series: IHI’s collaborative model for achieving breakthrough improvement. IHI Innovation series white paper. Boston; 2003.
Kilo CM. A framework for collaborative improvement: lessons from the institute for healthcare improvement’s breakthrough series. Qual Manag Health Care Summer. 1998;6(4):1–14.
Mistry KP, Jaggers J, Lodge A. Using six sigma methodology to improve handoff communication in high risk patients. In: Henriksen K, Battles JB, Keyes MA, et al., editors. Advances in patient safety; new directions and alternative approaches (Vol 3: Performance and tools). Rockville: Agency for Healthcare Research and Quality; 2008.
Horbar JD, Rogowski J, Plesek P, et al. Collaborative quality improvement for neonatal intensive care. Pediatrics. 107(1):14–22. https://doi.org/10.1542/peds.107.1.14.
Sundberg M,Paul R, Verghese G. Teamwork and Collaboration. Patient safety and quality in pediatric hematology/oncology and stem cell transplantation; 2017.
Berwick DM. A primer on leading the improvement of systems. BMJ. 1996;312(7031):619–22. https://doi.org/10.1136/bmj.312.7031.619.
Langley G, Moen R, Nolan K, et al. The improvement guide: a practical approach to enhancing organizational performance. 2nd ed. San Francisco: Jossey-Bass; 2009.
Schouten LMT, Grol RP, Hulscher ME. Factors influencing success in quality improvement Collaboratives: development and psychometric testing of an instrument. Implement Sci. 2010;5(1):1–9.
• Erum NS, Serene O, et al. Understanding the components of quality improvement Collaboratives: a systematic literature review. Milbank Q. 2013;91(2):354–94. This manuscript details in robust manner the potential components of successful QI collaboratives. It details the latest collaboratives in both pediatrics and adults and attempts to link successful components to outcomes, a novel approach.
Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The improvement guide: a practical approach to enhancing organizational performance. 2nd ed. San Francisco: Jossey-Bass Publishers; 2009.
National Pediatric Cardiology Quality Improvement Collaborative. For parents by parents http://jcchdqi.org/parents; 2012.
Families. Improve Care Now. https://improvecarenow.org/families; 2012.
Collaborative Chronic Care Network. N of 1 trials. http://c3nproject.org/innovations/n-1-trials. 2012.
Anderson JB, Beekman R, Kugler JD. Improvement in interstage survival in a national pediatric cardiology learning network: for the national pediatric cardiology quality improvement collaborative. Circ Cardiovasc Qual Outcomes. 2015;8:428–36.
Adirim T, Kelley MKamila M et al. A new era in quality measurement: the development and application of quality measures. Pediatrics. 2017; 139(1).
Pediatric Health Information System. Children’s Hospital Association. Available at: http://www.childrenshospitals.org. Accessed 31 Oct 2012.
Agency for Healthcare Research and Quality. Grants on-line database. Factors Associated with Quality of Care Delivered to Children in US EDs. Available at: http://gold.ahrq.gov/projectsearch/grant_summary.jsp?grant¼R01þHS19712-03. Accessed 3 Oct 2017. 36.
Agency for Healthcare Research and Quality. Grants on-line database. Improving the Quality of Pediatric Emergency Care Using an Electronic Medical Record. Available at: http://gold.ahrq.gov/projectsearch/grant_summary.jsp?grant¼R01þHS20270-02. Accessed 2 Oct 2017. 37.
Agency for Healthcare Research and Quality. Grants on-line database. ParentLink: Better and Safer Emergency Care for Children. Available at: http://gold.ahrq.gov/projectsearch/grant_summary.jsp?grant¼R01þHS14947-02. Accessed 3 Oct 2017.
Miller M, Wietecha M. Keeping children healthy. Fresh approaches are sorely needed to expand pediatric HAI prevention efforts. Mod Healthc. 2012;42(1):22.
Grades of Recommendation, Oxford Centre for Evidence Based Medicine. Available at: www.cebm.net/index.aspx?o=1047. Accessed 1 Oct 2017.
Dougherty D, Conway PH. The 3 Ts roadmap to transform U.S. healthcare: the “how” of high-quality care. JAMA. 2008;299(19):2319–21.
Clancy C, Margolis P, Miller M. Collaborative networks for both improvement and research. Pediatrics. 2013;13(Supplement 4):S210–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Raina Paul and George R. Verghese declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Quality Improvement
Rights and permissions
About this article
Cite this article
Paul, R., Verghese, G.R. Improving the Quality of Pediatric Healthcare through Quality Improvement Collaboratives. Curr Treat Options Peds 3, 362–373 (2017). https://doi.org/10.1007/s40746-017-0105-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-017-0105-9