Abstract
Continuity of care has been considered, as a key component of the treatment process, especially after discharge from the hospital. Establishing treatment continuity is critical to achieving successful treatment outcomes. Roozbeh Home Care Program was developed to ensure the continuity of care in patients with severe mental illness. This study aims to investigate the consequences of discontinuing a home care service including; relapse, readmission, service satisfaction, severity and disability, in patients with severe mental illness in Iran. Forty-three patients who received home care service for more than 6 months were included. They were assessed 3 and 6 months after receiving the service; and 12 months after the program discontinuation. There was a significant difference between the hospitalization rate during (0.42 ± 0.64) and 1 year after the program's discontinuation (0.65 ± 1.46). The majority of the caregivers (70%) were highly satisfied with the home care services. Among the patients who received the homecare services, 40.4% were highly satisfied; and 21.2% were moderately satisfied. There was no significant difference between disability (as measured by World Health Organization Disability Assessment Schedule), clinical improvement (as measured by Clinical Global Impression-Improvement Scale), or severity of illness (as measured by Clinical Global Impression Severity of the Illness Scale) during and 1 year after program's discontinuation. During the time of receiving the service, hospitalization rate was reduced. Patients and caregivers were satisfied with the service. Providing psychiatric services at home should be considered as a solution to maintain the continuity of care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psychiatric disorders are common in the general population. Severe mental illnesses (SMI) have always been a major cause of disability associated with chronic illnesses. Mental disorders caused 7% of all global burden of disease as measured in DALYs-Disability adjusted life years and 19% of all years lived with disability (Rehm and Shield 2019). Therefore, providing comprehensive long-term care to patients with SMI has become a significant concern (Nicaise et al. 2020). Continuity of care has been considered a key component of the treatment process, especially after discharge from the hospital. Establishing treatment continuity is critical to achieving successful treatment outcomes (Burns et al. 2009; Huang et al. 2017; Lam et al. 2020). Continuity of care is an indicator of the quality of care. Treatment continuity has been defined as a structure with different dimensions, both therapeutic and socio-supportive, which is obtained by combining different levels of treatment with social services according to the patient's needs (Huang et al. 2017; Ruud et al. 2016). Currently, most health system structures focus on the treatment of hospitalized patients and the acute phase of the disease. Outpatient medical services are followed in different ways, concentrating on the principle of continuity of treatment due to the critical situation of the patient in the discharge process (Dewa et al. 2011; Lam et al. 2020). Different methods of maintaining continuity of treatment for psychiatric patients have been explored in several studies. Therefore, further study on this basic principle of care for patients with severe psychiatric disorders is considered necessary (Andrade et al. 2014; Nicaise et al. 2020; Puntis et al. 2016; Belling et al. 2011).
In recent years in Iran, some efforts were made to provide home care services to patients with SMI. Sharifi et al. (2012) investigated the effectiveness of home care services in patients with severe mental disorders. During a 1-year follow-up, after-home care led to further reductions in readmission rates, further improvement in psychotic symptoms, and greater service satisfaction. Therefore, implementing a home care program was recommended, especially in hospitals with fewer facilities (Sharifi et al. 2012). Another study has shown that patients with a severe mental disorder who received intervention in the form of follow-up phone calls, home visits, and psycho-education for families had significantly lesser psychiatric readmission than patients who did not receive the intervention (Barekatain et al. 2014).
Roozbeh Home Care Program was developed in 2004 to ensure the continuity of care in patients with severe mental illness. This program provided home visit services monthly and phone call follow-ups every two weeks by psychiatry residents assisted by a nurse and a social worker. They provided social support in some cases like occupational or housing hel, along with medical support. Patients with at least two hospitalizations in the past year were enrolled in the program. In January 2019, this service faced challenges due to limited economic and human resources. In the beginning of the COVID-19 pandemic, the program stopped in March 2020. However, there are sufficient studies concerning the effectiveness of aftercare services for patients with severe mental illness, evidence on the consequences of service discontinuation for this group of patients, particularly in countries with low resources is sparse. This study aims to investigate the consequences of discontinuation of a home care program on relapse, readmission, the satisfaction of the service, severity and disability in patients with severe mental illness.
Materials and Methods
Study Design
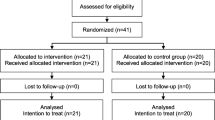
In this study, patients with severe mental illness who have received home care service for at least 6 months were included. Patients who were not willing to participate in the study and those who were recently introduced to the service (less than six consecutive months), were excluded.
Data Collection
After explaining the aim of the project and obtaining oral consent from the patients and caregivers, the participants enrolled in the study. Sociodemographic and clinical data were collected using the patient's clinical file and a telephone interview. Clinical data were recorded using standardized scales, including the adult self-administered version of the World Health Organization Disability Assessment Schedule version 2.0 (WHODAS) to measure patients’ disability. This version was filled by the patient. We used a simple scoring system according to WHO guidelines to calculate this scale. Each item takes a score from 1 (no disability) to 5 (completely disabled). Clinical Global Impression-Improvement scale (CGI-I) was used to measure clinical improvement, and the Clinical Global Impression-Severity scale (CGI-S) to measure clinical severity. These scales are scored by clinician self-interpretation from scores 1 (least severity) to 7 (most severity). The patients were assessed using these scales at the 3rd and 6th months of receiving the service and 1 year after the discontinuation. Relapse, readmission, adherence to treatment, substance abuse, level of education, history of underlying disease, and treatment follow-up after discontinuation were assessed via a telephone interview with the patient or the primary caregiver by a trained intern (SR). Moreover, the patient's and caregiver's satisfaction with the service was evaluated using a Likert scale from 1 to 5 (with 5 as the highest level of satisfaction).
Ethical Considerations
The Ethics Committee of the Tehran University of Medical Sciences approved the study (Ethics Code: IR.TUMS.MEDICINE.REC.1400.344).
Statistical Analysis
The collected data were analyzed using SPSS software version 23. The results were presented as averages and percentages. Chi-square and T-test were used to examine the differences between the study subgroups.
Results
Baseline data
In this study, 44 patients (21 men, 23 women) were included. The mean age of participants was 42.52 ± 10.84 years. The patients were diagnosed with schizophrenia (20 patients, 45.5%), bipolar disorder (12 patients, 27.3%), and schizoaffective disorder (12 patients, 27.3%). After discontinuation of the home care program, 20 patients (45.45%) continued the previous medications without any appointment with a psychiatrist, 18 patients (40.91%) reached the hospital outpatient clinic, four patients (9.09%) stopped taking medication, and two patients (4.55%) went to a private psychiatrist clinic. According to the family report, 32 cases (72.73%) experienced relapse, and 13 out of whom (29.55%) were hospitalized 1 year after discontinuation of service.
Hospitalization
The average duration of patients' enrollment in this service was 4.09 ± 1.51 years; the maximum time of enrollment was 11 years and the minimum time was about 9 months. There was a significant difference between the rate of hospitalization during the service (0.42 ± 0.64) and 1 year after the service termination (0.65 ± 1.46) (P value = 0.013). The most number of hospitalization before enrollment was 20, and the most number of hospitalization during the program was 7 for one patient and 2 for another.
Patient and Caregiver Satisfaction
A Likert scale was used to assess patients' and caregivers' satisfaction regarding home care services. On a scale of 1–5 (5 as the highest level of satisfaction), 19 patients (40.4%) chose a satisfaction score of 5, 13 (27.7%) chose 4, and 6 (12.8%) chose 3. Using the same scale, 33 caregivers (70.2%) chose a satisfaction score of 5, 10 (21.3%) chose 4, and 1 (2.1%) chose 3. The patients' and caregivers' satisfaction differed significantly; caregivers were more satisfied than patients. (Pearson Chi-Square = 12.385, P value = 0.002).
Function and Disability
The patients were assessed using the World Health Organization Disability Assessment Schedule (WHODAS) at the third and sixth months of program enrollment and a year after its termination. The mean WHODAS score of patients was 23.59 ± 7.87 in the third month of enrollment, 23.51 ± 8.94 in the sixth month, and 25.85 ± 9.32 a year after the program termination. The WHODAS score did not differ significantly in the third and sixth months of enrollment (t = − 0.31, P = 0.75), and at the third month of enrollment and a year after the program's termination (t = -1.72, P value = 0.06).
The patients were assessed using the Clinical Global Impressio-Improvement (CGI-I) scale and Clinical Global Impression-Severity (CGI-S) scale at the same intervals as the WHODAS assessment. The mean CGI-I score of patients was 4.48 ± 1.19 in the third month of enrollment, 4.43 ± 1.11 in the sixth month, and 4.60 ± 0.87 a year after the program's termination. The CGI-I score did not differ significantly at the third and sixth months of enrollment (t = 0.19, P = 0. 84), and at the third month of enrollment and a year after the program's termination (t = − 0.28, P value = 0.77). The mean CGI-S score of patients was 3.59 ± 1.24 in the third month of enrollment, 3.73 ± 1.14 in the sixth month, and 3.86 ± 1.32 a year after the program's termination. The CGI-S score did not differ significantly in the third and sixth months of enrollment (t = − 0.74, P = 0.46), and at the third month of enrollment and a year after the program's termination (t = − 1.08, P value = 0.28). Table 1 shows the WHODAS, CGI-I, and CGI-S scores.
There was no significant relationship between substance use (P value = 0.441), underlying disease (P value = 0.340), education (P value = 0.937) and follow-up type (P value = 0.415) with disease recurrence. There was no significant relationship between substance use (P value = 0.485) and underlying disease (P value = 0.733) and hospitalization during the study. There was no significant relationship between substance use (P value = 0.322) and underlying disease (P value = 0.082) and hospitalization after the study (P value = 0.322).
Discussion
This study aims to assess the consequences of discontinuing an established home care program on relapse, readmission, the satisfaction of the service, severity and disability in patients with severe mental illness (SMI). To the best of our knowledge, this study is unique as it assessed the consequences of a home care program cessation on patients with SMI. Roozbeh home care program is designed to deliver aftercare services by using a multidisciplinary approach to care for persons with severe mental illnesses. The objectives of the program were preventing relapse and re-hospitalization; increasing treatment adherence, and increasing patient and family satisfaction with the services. The program consisted of monthly home visits by home care teams, including a psychiatry resident, a nurse, and a social worker. They provided the services planned by a faculty member psychiatrist. The team members had special training in mental health care. Additionally, weekly meetings were held for teams with a faculty member where home visits were discussed to attain personalized decisions for each patient. The provided care included biopsychosocial and clinical assessment, development of the plan of care, medication management, psycho-educating the patient and the family, doing social work and guiding the family on how to access the community resources. All services were provided free of charge.
The results showed that the hospitalization rate of the patients reduced during the home care program significantly. The patients' and caregivers' satisfaction with the program differed significantly, and caregivers were more satisfied than their patients. In our study, there was no significant difference between the disability caused by the disease in six areas of daily life (WHODAS) and the severity of clinical improvement (CGI) compared within the third and sixth months after treatment.
Our home care program could successfully reduce hospitalization rates among enrolled patients. Similar to our findings, in a study by Lam et al. hospitalization and readmission rates were significantly lowered following a home visit program (Lam et al. 2020). A study by Tomita et al. reported less readmission and homelessness among psychiatric patients registered with a comprehensive supportive program (Tomita and Herman 2015). Puntis et al. demonstrated a significant association between readmission, hospitalization rate, and hospitalization days with treatment continuity (Puntis et al. 2016).
Both our patients and their caregivers showed high satisfaction levels with the home care program, but the caregiver’s satisfaction levels were significantly higher. A study on patients' satisfaction with a mental health home visit service showed improved satisfaction after 6 months, but decreased after 12 months (Chang and Chou 2015). Many factors may contribute to this satisfaction reduction over time. Patients with severe mental health problems require long-term treatment and rehabilitation. Therefore, home care programs need constant evaluations to remain efficient.
In addition, hospital staff needs to be encouraged to implement such programs to achieve continuity of care (Smith et al. 2019). Another study suggested that adherence and continuity of treatment are multidimensional issues related to many factors such as age, sex, occupation, underlying disease, and education (Bindman et al. 2000). In the current study, no significant relationship was observed between substance use, underlying disease, education, and type of follow-up with disease recurrence and hospitalization during and after the service discontinuation. Contrary to our results, Adairein et al. found that in patients with older age, lower annual income, the experience of psychosis, no history of suicide, and no alcohol use, continuity of treatment was significantly better (Joyce et al. 2010). In most previous studies, the relationship between treatment continuity and hospitalization was generally significant regardless of the diagnosis, and the type of medical institution referred for outpatient services. The trends show that the extent of this difference was stronger in the group of tertiary hospitals. This tendency may be because people with poor follow-up in primary care are more likely to contact higher-level medical institutions (Kim et al. 2018).
Limitations
The absence of a control group, along with a relatively small sample size in a single center are the potential limitations of this study. The limited number of patients may have reduced the study's power to examine some correlations. In this study primary assessments of special indexes (WHODAS, CGI-I, CGI-S) was done at various times due to the long duration of the program running. The length of enrollment in the program, and so the hospitalization rates interval differed among patients during the program. To eliminate this bias, the mean hospitalization rates were measured during the program period.
Recommendations
It is suggested that studies with larger sample size, longer follow-up period, and control group be conducted to determine the consequences ofdiscontinuation of home care programs, especially from the patients' point of view and factors affecting social and occupational performance and promotion. Quality of life should be examined. In addition, it is better to examine and analyze the reasons for the lack of continuity of care after discharge from the service.
The authors believe that it is necessary to plan to continue home care services for patients with severe mental illness, especially during epidemics, such as the COVID-19 pandemic. More advocacy efforts and find sustained economic and human resources are recommended.
Implications for Behavioral Health
This study shows that some patients do not have sufficient continuity in the treatment process. This finding presents the importance of providing psychiatric services at home for patients with SMI to maintain the continuity of care. Various causes can play a role in not pursuing treatment. Therefore, it is recommended to examine the causes from the perspective of patients. Home visits are often satisfactory to families and patients and, regardless of many individual and clinical characteristics, can reduce the rate of hospitalization but may not have a significant impact on other important outcomes alone, such as improving social and occupational performance and quality of life. Perhaps improvement in patient's performance requires a more comprehensive treatment plan in which other domains of aftercare services are targeted. This hypothesis needs to be studied more carefully.
References
Andrade LH, Alonso J, Mneimneh Z, Wells JE, Al-Hamzawi A, Borges G, Bromet E, Bruffaerts R, de Girolamo G, de Graaf R, Florescu S, Gureje O, Hinkov HR, Hu C, Huang Y, Hwang I, Jin R, Karam EG, Kovess-Masfety V, Levinson D, Matschinger H, O’Neill S, Posada-Villa J, Sagar R, Sampson NA, Sasu C, Stein DJ, Takeshima T, Viana MC, Xavier M, Kessler RC. Barriers to mental health treatment: results from the WHO World Mental Health surveys. Psychol Med. 2014;44(6):1303–17. https://doi.org/10.1017/S0033291713001943.
Barekatain M, Maracy MR, Rajabi F, Baratian H. Aftercare services for patients with severe mental disorder: a randomized controlled trial. J Res Med Sci. 2014;19(3):240–5.
Belling R, Whittock M, McLaren S, Burns T, Catty J, Jones IR, Rose D, Wykes T, the ECHO Group. Achieving continuity of care: facilitators and barriers in community mental health teams. Implement Sci. 2011;6(1):23. https://doi.org/10.1186/1748-5908-6-23.
Bindman J, Johnson S, Szmukler G, Wright S, Kuipers E, Thornicroft G, Bebbington P, Leese M. Continuity of care and clinical outcome: a prospective cohort study. Soc Psychiatry Psychiatr Epidemiol. 2000;35(6):242–7. https://doi.org/10.1007/s001270050234.
Burns T, Catty J, White S, Clement S, Ellis G, Jones IR, Lissouba P, McLaren S, Rose D, Wykes T. Continuity of care in mental health: understanding and measuring a complex phenomenon. Psychol Med. 2009;39(2):313–23. https://doi.org/10.1017/S0033291708003747.
Chang Y-C, Chou FH-C. Effects of home visit intervention on re-hospitalization rates in psychiatric patients. Community Ment Health J. 2015;51(5):598–605. https://doi.org/10.1007/s10597-014-9807-7.
Dewa CS, Chen M-C, Chau N, Dermer S. Examining factors associated with the length of short-term disability-free days among workers with previous short-term disability episodes. J Occup Environ Med. 2011;53(6):669–73. https://doi.org/10.1097/JOM.0b013e31821e5a0b.
Huang H-H, Chen C-Y, Tsay J-H, Chou Y-J, Huang N. Factors in maintaining a stable patient–physician relationship among individuals with Schizophrenia. Community Ment Health J. 2017;53(5):578–88. https://doi.org/10.1007/s10597-017-0123-x.
Joyce AS, Adair CE, Wild TC, McDougall GM, Gordon A, Costigan N, Pasmeny G. Continuity of care: validation of a self-report measure to assess client perceptions of mental health service delivery. Community Ment Health J. 2010;46(2):192–208. https://doi.org/10.1007/s10597-009-9215-6.
Kim W, Jang S-Y, Lee T-H, Lee JE, Park E-C. Association between continuity of care and subsequent hospitalization and mortality in patients with mood disorders: results from the Korea National Health Insurance cohort. PLoS ONE. 2018;13(11):e0207740. https://doi.org/10.1371/journal.pone.0207740.
Lam M, Li L, Anderson KK, Shariff SZ, Forchuk C. Evaluation of the transitional discharge model on the use of psychiatric health services: an interrupted time series analysis. J Psychiatr Ment Health Nurs. 2020;27(2):172–84. https://doi.org/10.1111/jpm.12562.
Nicaise P, Giacco D, Soltmann B, Pfennig A, Miglietta E, Lasalvia A, Welbel M, Wciórka J, Bird VJ, Priebe S, Lorant V. Healthcare system performance in the continuity of care for patients with severe mental illness: a comparison of five European countries. Health Policy. 2020;124(1):25–36. https://doi.org/10.1016/j.healthpol.2019.11.004.
Puntis SR, Rugkåsa J, Burns T. The association between continuity of care and readmission to hospital in patients with severe psychosis. Soc Psychiatry Psychiatr Epidemiol. 2016;51(12):1633–43. https://doi.org/10.1007/s00127-016-1287-3.
Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. 2019;21(2):10. https://doi.org/10.1007/s11920-019-0997-0.
Ruud T, Aarre TF, Boeskov B, Husevåg PS, Klepp R, Kristiansen SA, Sandvik J. Satisfaction with primary care and mental health care among individuals with severe mental illness in a rural area: a seven-year follow-up study of a clinical cohort. Int J Ment Health Syst. 2016;10(1):33. https://doi.org/10.1186/s13033-016-0064-8.
Sharifi V, Tehranidoost M, Yunesian M, Amini H, Mohammadi M, Jalali Roudsari M. Effectiveness of a low-intensity home-based aftercare for patients with severe mental disorders: a 12-month randomized controlled study. Community Ment Health J. 2012;48(6):766–70. https://doi.org/10.1007/s10597-012-9516-z.
Smith P, Nicaise P, Giacco D, Bird V, Bauer M, Ruggeri M, Welbel M, Pfennig A, Lasalvia A, Moskalewicz J, Priebe S, Lorant V. Predictors of personal continuity of care of patients with severe mental illness: a comparison across five European countries. Eur Psychiatry. 2019;56(1):69–74. https://doi.org/10.1016/j.eurpsy.2018.12.003.
Tomita A, Herman DB. The role of a critical time intervention on the experience of continuity of care among persons with severe mental illness following hospital discharge. J Nerv Ment Dis. 2015;203(1):65–70. https://doi.org/10.1097/NMD.0000000000000224.
Funding
This study was supported by a grant from Tehran University of Medical Sciences (Grant No: 1400-1-101-52570).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Razeghi, S., Amini, H. & Mirsepassi, Z. The Consequences of Discontinuing a Home Care Service for Patients with Severe Mental Illness After the COVID-19 Pandemic. J. Psychosoc. Rehabil. Ment. Health 10, 151–156 (2023). https://doi.org/10.1007/s40737-022-00294-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40737-022-00294-4