Summary
Purpose
This project aimed to investigate allergen information practices of food businesses selling non-prepacked foods after the implementation of the new Swiss food law in May 2017.
Methods
A cross-sectional telephone survey was conducted with food businesses selling non-prepacked foods in Switzerland. A short, standardised questionnaire was developed in German, based on previous research and literature. It was subsequently translated into French and Italian. Altogether, 882 businesses (restaurants, dairies, butcher shops and bakeries) were contacted, of which 387 were willing to participate. SPSS® (IBM, Armonk, NY, USA) was used for statistical analyses.
Results
The vast majority (86.0%) of food businesses provides oral allergen information. Only 14.0% currently provide written allergen information to the customer, either upfront or on request. The most frequently used labelling system in written allergen declaration was naming all ingredients (35.2%). A significant number (39.8%) do not place a notice on how to obtain allergen information, although this is a legal requirement in Switzerland when not providing written information upfront.
Conclusion
So far, not all food businesses have been complying with the new Swiss food law on allergen information of non-prepacked food. Therefore, awareness of the legal obligations around communicating allergen information as well as the verification of its implementation should be enhanced. To meet the needs of consumers and avoid reactions, some form of written allergen information should be promoted. Giving this information on request might encourage communication between customer and staff, thus providing an extra measure of verification.
Similar content being viewed by others
Introduction
An estimated 1–10% of the Swiss population suffers from food allergies and around 15–20% from intolerances [1,2,3]. Whereas symptoms of food intolerance are mostly local and typically affect the gastrointestinal tract, allergic reactions vary from mild skin reactions to a potentially life-threatening anaphylactic shock.
For these persons, eating out represents a particular challenge. A review reports that 21–31% of allergic food reactions occur in restaurants [4] According to the European Anaphylaxis registry, 4.7% of recorded anaphylaxis cases in children and adolescents were located in restaurants [5]. Likewise, in consumers with coeliac disease, gluten exposure is associated with eating in restaurants [6, 7].
It is a challenge for providers of non-prepacked foods to provide reliable allergen information [8]. A systematic review of studies identified a lack of knowledge about food allergies in restaurant personnel [9]. Restaurant managers named the cost of training, high employee turnover, time constraints, language barriers, as well as employee apathy and lack of interest as barriers to increase their staff’s knowledge on how to prevent allergic reactions [10]. Only a small number of restaurant personnel receives some type of allergy training [8]. Moreover, the risk of cross-contamination may be higher in non-prepacked foods, especially in restaurants in which food preparation space is more constrained, dedicated equipment is uncommon, and constant switching occurs among many formulations [11].
In May 2017, the new Swiss food law took effect. It gives more responsibility to food businesses selling non-prepacked food to provide information on ingredients that may cause allergies or intolerances (hereafter referred to as “allergenic ingredients”). The general principle is providing a written allergen declaration (Art. 5, FoodIO). However, it also allows for the provision of oral information on the condition that a written note on how to obtain information is provided, and someone can provide this information accurately. Oral information can then be either given based on written documentation or by an informed person. In contrast to prepacked foods, information on possible cross-contact is not mandatory. This had first been decided informally (email conversation with the Federal Food Safety and Veterinary Office, 2018) and is now part of the amendment to Swiss food law (Art. 5, FoodIO).
Until now there has been little knowledge on how businesses implement these new regulations in daily practice in Switzerland. Thus, the present survey aimed to evaluate the ways of oral and written allergen information, as well as the allergen declaration systems currently used by food providers.
Methods
To investigate the allergen information provision by food businesses selling non-prepacked foods, we conducted a cross-sectional survey using a structured telephone interview with food businesses. This option was chosen based on previous experience of how to best contact this target group.
Sampling and data collection
Food businesses were randomly selected from the online directory ‘search.ch®’ by choosing restaurants, dairies, butcher shops and bakeries that displayed a telephone number and an email address online. The aim was to include ten businesses per category per canton. In some cantons less than this number were available in the directory.
Questions for the interviews were developed on the basis of previous research, relevant literature [12, 13, 13, 14] and discussion within the research team. As we identified time as a limiting factor for interviews with this target group, we kept the questionnaire as short as possible. The questionnaire consisted of three sections and used predominantly closed questions: (1) Information on the business; (2) Allergen information provision; (3) Training of employees. Italian and French native speakers from the research team translated the questionnaire into their first language. All three versions were pretested with at least two businesses and adapted accordingly.
Four interviewers conducted the interviews from March to November 2019 and entered the answers directly in a SurveyMonkey® format to minimize recording mistakes and facilitate data analysis.
Statistics
Statistical analyses were conducted using SPSS 24 Statistics® (IBM, Armonk, NY, USA). The data from SurveyMonkey® (Survey Monkey, San Mateo, CA, USA) were exported and were merged into one database. The classification into urban, intermediate and rural area was completed in line with the typology used by the Swiss Federal Statistical Office [15]. Frequencies and relative frequencies were calculated. Pearson’s Χ2 test was performed comparing categorial variables. In case more than 20% of the categories had an expected frequency under 5, Fischer’s exact test was used. Qualitative questions were categorized in Excel 365® (Microsoft Corporation, Redmond, WA, USA).
Results
In total, 882 businesses were contacted, and 387 (43.9%) were willing to take part; 198 were located in the German-speaking, 170 in the French-speaking and 19 in the Italian-speaking regions of Switzerland. The characteristics of the food businesses are summarised in Table 1.
Guests mentioned food allergies or intolerances at least weekly in 221 of the 387 businesses, 91 said monthly, 55 seldom or never and 20 participants could not name the frequency. When comparing urban, intermediate and rural areas, 29.4% of the urban business representatives indicated that they had such inquiries daily, compared to 15.2% in the intermediate and 10.7% in rural areas (Χ2 (2, N = 367) = 16,338, p < 0.001). In contrast, 13.4% of rural business representatives said they never received such inquiries, compared to 6.7% in urban and 3.3% in intermediate areas (Χ2 (2, N = 367) = 7.661, p = 0.022). Differences between language regions can be found in supplemental table A.
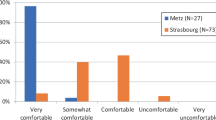
In all, 331 businesses reported that they give oral allergen information, and only 54 in writing (Χ2 (1, N = 385) = 199.296, p < 0.001). Two business representatives said that they did not provide any information on allergens. A similar number of businesses were giving oral information using the option of exclusive oral information by an informed person or written documentation. When written information was provided to the customer, there was a clear preference for displaying this information upfront, without the customer having to ask for it, for example in the menu cards, rather than on request {36 versus 18 (Χ2 (1, N = 54) = 6.000, p = 0.014)}. Out of these 54 businesses, 19 list all ingredients, 11 only the allergenic ingredients, 8 used symbols, 7 used number systems, 6 used letter systems and 3 used a table matrix. Types of information provision besides menus were cash register or scaling systems and signs naming the allergens (Fig. 1).
Methods of providing allergen information used by food businesses selling non-prepacked food. The green roof represents all surveyed food businesses. The number and percentage of businesses using the option of exclusive oral allergen information is shown in blue, those giving written allergen information in purple. Written allergen information is further divided into those businesses giving this information upfront without the customer having to ask and those giving the information on request. Oral information is divided into the options of having a written documentation or giving the information by an informed person. The bar chart on the right illustrates the various declarations systems used for written information. aTwo businesses answered not to provide any allergen-information
There were some differences observed between types of businesses. Restaurants and dairy shops used oral communication by an informed person more frequently compared to written documentation {65 versus 15 (Χ2 (1, N = 80) = 31.250, p < 0.001) and 54 versus 23 (Χ2 (1, N = 77) = 12.481, p < 0.001), respectively}, whereas bakeries/patisseries and butcher shops preferred written documentation for their staff to provide the allergen information orally {71 versus 20 (Χ2 (1, N = 91) = 28.582, p < 0.001) and 52 versus 31 (Χ2 (1, N = 83) = 5.313, p = 0.021), respectively}. Furthermore, the frequency of providing written allergen information varied significantly between different types of businesses (Χ2 (3, N = 385) = 36.650, p < 0.001). While 29.8% of restaurants present written information, this percentage dropped to 11.7% in bakeries/patisseries, 6.7% in butcher shops and 2.5% in dairy shops. Various types of written declaration systems were used in restaurants, whereas dairies exclusively used a list of ingredients, butcher shops used a list of ingredients or the allergenic ingredients and bakeries/patisseries use a list of ingredients symbols or allergenic ingredients. Differences in the methods of providing allergen information between language regions and typology were not significant.
In case of oral communication by an informed person (n = 170), information was provided by service staff (n = 109), the chef, butcher or baker (n = 73), the business head (n = 42), management staff (n = 10), trainees (n = 5) as well as other persons (n = 20), such as the head of quality management, administration or the events department. Multiple answers were possible.
Only 14 businesses reported that their staff had received external training. Training was either provided in-house (n = 183), via information material (n = 76) or via “other training” (n = 87), which included during vocational training, through internal discussions, learning by doing and other types of training. Multiple answers were possible. About one quarter (n = 101) reported that the staff had not received any training. This differed significantly between the methods of how allergen information is given (Χ2 (3, N = 385) = 12.721, p = 0.05). Whereas 34.7% of those businesses giving allergen information exclusively orally do not provide any training, this percentage was lower in those giving allergen information using written documentation (19.9%), written information upfront (19.4%) and written information on request (11.1%).
A notice on how to obtain allergen information was provided by 203 of the 349 of those businesses not providing written information upfront (Fig. 1). This differed significantly between the types of businesses (Χ2 (3, N = 349) = 46.280, p < 0.001). While 84.0% restaurants provided such a sign, this percentage decreased to 63.1% in butcher shops, 40.4% in bakeries/patisseries and 42.9% in dairy shops. Moreover, there was a difference between the three language regions (Χ2 (2, N = 349) = 7.904, p = 0.019), with 64.8% in the German-speaking region, 52.6% in the French-speaking region and 38.9% in the Italian-speaking regions, respectively. Another significant difference was observed between urban 67.1%, intermediate 52.9% and rural areas 49.1% (Χ2 (2, N = 349) = 9.738, p = 0.008, Table 2). There was no significant difference between members and non-members of professional associations.
Even though it is not obligatory for non-prepacked foods, 182 food businesses warn their customers about potential cross-contact; reasons for that included reassurance (n = 123), customer request (n = 54), internal concern (n = 30) and content of certification (n = 11) (multiple answers possible). Usage of this information varied significantly between types of businesses (Χ2 (3, N = 387) = 61.386, p < 0.001). Bakeries /patisseries reported using this information frequently (72.8%), whereas only few dairies did (13.9%; Table 3). Warnings about possible cross-contamination were more common in urban (51.7%) and intermediate areas (51.5%) compared to rural areas (36.4%) (Χ2 (2, N = 387) = 7.640, p = 0.022, Table 2). Businesses inform consumers in various ways, including statements that products ‘may contain traces of a certain allergenic ingredient’ or that they ‘may contain traces of all allergenic ingredients’. Some specify the ‘may contain’ statement on specific products, whereas others make more general statements for all products. Few businesses report that they do not serve customers, if they indicate having a severe food allergy.
Discussion
To our knowledge this is the first survey investigating current allergen information practice in Swiss businesses selling non-prepacked foods. The majority of businesses reported regular inquiries by food allergic or intolerant consumers, especially in urban regions. Food allergen information is mostly provided orally. If allergen information is provided in written form, most food businesses name the ingredients explicitly.
Only 54 businesses implemented written allergen information, even though this is defined as the general principle by Swiss food law (Art. 5, FoodIO). Reasons may include effort and cost of written allergen declarations, as it requires identifying and systematically evaluating allergens in all purchased and self-prepared products, as well as providing materials such as menus with supplementary declaration systems. A report for the federal government concluded that the new law will cause one-time costs of 118 million Swiss francs and annual costs of 17.3 million Swiss francs for food businesses in Switzerland [16]. The providers could question this effort, as ultimately only few customers might benefit from written allergen labelling. This includes those suffering from one of the 14 allergens requiring declaration and not reacting to small amounts. This is also reflected by the observation of the majority of businesses that receive inquiries on allergens only weekly or even less often. These factors may explain the businesses’ preference to provide oral allergen information as long as they are allowed to do so.
Nearly half of the businesses (44.2%) reported that they use the option of an informed person providing customer allergen information (Art. 5, FoodIO). Especially restaurants and dairy shops used this option. In restaurants, constant switching of menu and recipes may complicate having written information [11]. However, exclusive oral allergen information may put customers at risk of reactions, as it is in most cases not possible to remember all ingredients without any written documentation. Moreover, studies find that food allergic and intolerant customers wish to have written allergy information, preferably without requesting it specifically [12,13,14, 17]. It is assumed that written allergen information is more trustworthy because it forces the provider to focus on allergen management [12]. On the other hand, written information upfront could inhibit communication between the staff and the customer, which could lead to unintended reactions due to less careful preparation of meals or selection of foods because staff members are not aware of the special needs of the allergic consumer [8, 18]. For this reason, providing written information on request might be the safest way. Currently, this method is only used by a small number of food businesses. This might be due to the extra effort and costs.
Another issue of exclusive oral communication is the person giving this information. The results show that there is no consistent interpretation of the term “informed person”. However, providing adequate allergen information may be difficult for staff without adequate training, and in about one quarter of the surveyed businesses staff has not received any training. Young and Thaivalappi reported in their 2018 systematic review even higher rates of non-training. Across 12 studies, a median of 65% of the participants had not received any prior food allergy training [9]. They further reported for three included studies that only 25–56% of participants were able to correctly identify at least three of the major allergens [9]. Correct identification, however, is a requirement for giving reliable oral allergen information. Preliminary data of a pilot trial showed that this competence can already be increased by completing a 1 h workshop [19]. Therefore, clear training obligations in the case of oral allergen information, as required in Austria (§3 para 3 AIV), may improve business staff’s knowledge and thus lead to more reliable information. Free online training as offered by the Food Standards Agency for UK may be an effective way to reach a wide audience and improve food allergy management skills [20, 21].
Those businesses that give written information mostly provide a list where they either name all ingredients, or solely the allergenic ones. Symbols, number and letter systems are rarely used, but with similar frequency. The biggest variety of labelling systems were found in restaurants, where all the above systems were used. One reason for this could be that restaurants use menu cards, which offer more freedom of design than for example cash registers. Nevertheless, the space in menu cards is limited, which could explain why coding systems are popular [12]. These, however, are not the preferred labelling system of food allergic and intolerant customers. Customers clearly stated in surveys that they prefer the written name of the allergenic ingredient as information [12, 17] Only participants in a 2016 qualitative study by Begen et al. showed a preference for abbreviations or symbols by consumers in the UK [14].
Although not mandatory by law, nearly half of the businesses in this survey provide information on potential cross-contact, mainly for liability reasons. One explanation could be that, by the time the new food law took effect, cross-contact was not definitely regulated, so that some businesses might have the impression that they are obliged to give this information (Food IO, SR 81.022.16, status as of 1 May 2017). Moreover, this information is obligatory for prepacked foods in Switzerland in case a certain threshold is exceeded (Art. 5, FoodIO). This might have reinforced that impression. As seen in other countries, a lack of regulation can lead to an overuse of precautionary labelling on the one hand and non-use in relevant situations on the other hand [22]. As a consequence, the consumer has a too limited food choice, or gets a false sense of security [22]. A German survey confirmed that the non-use of precautionary labelling may lead to unintended allergic reactions [23]. These kinds of shortcomings are especially important for persons with severe reactions to small amounts of the eliciting food [24], as well as persons with coeliac disease, who must follow a strict gluten-free diet [25]. Therefore, better regulation is necessary. As processes in businesses providing non-prepacked food are often less standardised, it may not be possible to apply the same rules as for prepacked food. However, a statement on which allergenic ingredients are used in the kitchen or factory might help the consumer to make their own risk assessment.
Our results show that the majority of participating businesses implement the current legislation correctly. However, two businesses reported that they refused to give allergen information. Additionally, only 58.1% of those businesses giving allergen information orally or written on demand provided a notice that allergen information can be obtained orally if required, despite the legal obligation to do so (Art. 5, FoodIO). This might be due to the unawareness of this relatively new obligation. This would also explain why they reveal this omission in a survey. While most restaurants (84%) fulfilled this obligation, this is less common in other types of businesses. This may be due to the more frequent inquiries by food allergic or intolerant consumers and consequently greater awareness in restaurants. The same might apply to urban compared to rural areas. Similar to our survey, cantonal chemists found that 55% had not fully complied with the legal requirements regarding allergen information when inspecting 1100 businesses selling non-prepacked foods in 2018 [26]. They also attributed this to a lack of awareness on the part of the businesses regarding their duties and responsibilities. In the case of the offending businesses, the rectification of the deficiencies was ordered. As a further consequence of this observation, the chemists announced that the allergen information provided by these businesses would be specifically monitored on continuous basis.
There are some limitations that need to be considered. Firstly, even though it was planned to differentiate further between types of restaurants, it turned out to be difficult to clearly assign a business to one category, as many of them provide more than one service, such as in-house and take-away services. Secondly, despite our effort to interview as many of the 882 selected food businesses as possible, we reached 387 businesses. The non-participating businesses could differ from the participating businesses in some relevant way. This may have led to a selection bias because these businesses might be less interested in the topic or even not comply with the law. In addition, we did not collect further data of the interviewee and have left his or her choice to the business to lower the burden of participation. The quality of the answers could, however, depend on the training and position of the participant. Lastly, the interviews were conducted by four interviewers. This was partly necessary due to language issues. Still, the quality of interviewing may differ. Most obviously, the interviewer conducting the French interviews attained much higher participation rates than the other interviewers.
In this survey, we intended to reach a representative sample size and therefore used a short and easily answerable questionnaire. It was not possible with this method to evaluate the quality of the allergen information given by the food businesses. A further observational study with mystery customers could give more in-depth knowledge on the quality of the allergen information. Another interesting investigation would be to evaluate, why businesses do not use written declaration in more depth. As training is a key factor for successful allergen management, the type(s) of training that can best reach the target group and that are most effective should be systematically evaluated.
Conclusion
Two years after the new food law took effect, legal obligations were not met by a substantial portion of food businesses taking part in this survey that sell non-prepacked foods. This part might even be higher, as fewer than half of the requested businesses participated. Measures must be taken to increase awareness of the obligations resulting from the new legislation, and its implementation should be verified more consistently as foreseen by Swiss cantonal chemists. Furthermore, information on possible cross-contamination should be regulated, as should the term “informed person” be more precisely defined in law. Forms of written allergen information should be promoted and established as principal standard as foreseen by the new food law. Where oral information is given without written documentation, training requirements should be established. When using written allergen information, a labelling system listing either all ingredients with the allergenic ingredients highlighted, or solely the allergenic ingredient can be recommended across different types of food businesses. Giving this information on request could promote communication between customer and staff. This might additionally solve restaurants’ concerns around menu design. It must be acknowledged that implementation is a big challenge and very costly for food businesses. The way in which the new food law is currently being implemented does not allow consumers with food allergies or intolerances to assess their risk when buying non-prepacked food or eating out and this may expose them to an increased risk of adverse reactions.
References
Lyons SA, Burney PGJ, Ballmer-Weber BK, Fernandez-Rivas M, Barreales L, Clausen M, et al. Food allergy in adults: substantial variation in prevalence and causative foods across Europe. J Allergy Clin Immunol Pract. 2019; https://doi.org/10.1016/j.jaip.2019.02.044.
Mustalahti K, Catassi C, Reunanen A, Fabiani E, Heier M, McMillan S, et al. The prevalence of celiac disease in Europe: results of a centralized, international mass screening project. Ann Med. 2010;42:587–95. https://doi.org/10.3109/07853890.2010.505931.
Storhaug CL, Fosse SK, Fadnes LT. Country, regional, and global estimates for lactose malabsorption in adults: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2017;2:738–46. https://doi.org/10.1016/S2468-1253(17)30154-1.
Versluis A, Knulst AC, Kruizinga AG, Michelsen A, Houben GF, Baumert JL, et al. Frequency, severity and causes of unexpected allergic reactions to food: a systematic literature review. Clin Exp Allergy. 2015;45:347–67. https://doi.org/10.1111/cea.12328.
Grabenhenrich LB, Dölle S, Moneret-Vautrin A, Köhli A, Lange L, Spindler T, et al. Anaphylaxis in children and adolescents: the European anaphylaxis registry. J Allergy Clin Immunol. 2016;137:1128–1137.e1. https://doi.org/10.1016/j.jaci.2015.11.015.
Arnaiz P. Wie leben Zöliakie-Betroffene in der Schweiz?: Studentisches Forschungsprojekt zum Thema Zöliakie. Basel: University of Basel; 2011.
Silvester JA, Graff LA, Rigaux L, Walker JR, Duerksen DR. Symptomatic suspected gluten exposure is common among patients with coeliac disease on a gluten-free diet. Aliment Pharmacol Ther. 2016;44:612–9. https://doi.org/10.1111/apt.13725.
Wen H, Kwon J. Restaurant servers’ risk perceptions and risk communication-related behaviors when serving customers with food allergies in the U.S. Int J Hosp Manag. 2017;64:11–20. https://doi.org/10.1016/j.ijhm.2017.03.009.
Young I, Thaivalappil A. A systematic review and meta-regression of the knowledge, practices, and training of restaurant and food service personnel toward food allergies and celiac disease. PLoS ONE. 2018;13:e203496. https://doi.org/10.1371/journal.pone.0203496.
Abbot JM, Byrd-Bredbenner C, Grasso D. Know before you serve. Cornell Hotel Restaur Adm Q. 2007;48:274–83. https://doi.org/10.1177/0010880407302779.
Taylor SL, Baumert JL. Cross-contamination of foods and implications for food allergic patients. Curr Allergy Asthma Rep. 2010;10:265–70. https://doi.org/10.1007/s11882-010-0112-4.
Schnadt S. Allergeninformation bei unverpackten Lebensmitteln – was Lebensmittelallergiker sich wünschen. Ergebnisse von Befragungen des Deutschen Allergie- und Asthmabundes zum Thema „Lose Ware“ im Zeitraum 2008–2013. AL. 2014;37:503–10. https://doi.org/10.5414/ALX01723.
Begen FM, Barnett J, Payne R, Gowland MH, DunnGalvin A, Lucas JS. Eating out with a food allergy in the UK: change in the eating out practices of consumers with food allergy following introduction of allergen information legislation. Clin Exp Allergy. 2018;48:317–24. https://doi.org/10.1111/cea.13072.
Begen FM, Barnett J, Payne R, Roy D, Gowland MH, Lucas JS. Consumer preferences for written and oral information about allergens when eating out. PLoS ONE. 2016;11:e156073. https://doi.org/10.1371/journal.pone.0156073.
Swiss Federal Statistical Office (BFS). Raumgliederungen. 2019. https://www.agvchapp.bfs.admin.ch/de/typologies/results?SnapshotDate=01.01.2019&SelectedTypologies%5B0%5D=HR_GDETYP2000. Accessed 1 Oct 2021.
Oesch T, Gehrig M, Graff A‑L, Küng V. Regulierungsfolgenabschätzung zum neuen Lebensmittelrecht: Schlussbericht. Bern: Schweizerische Eidgenossenscahft. Staatssekretariat für Wirtschaft SECO; 2015.
Eisenblätter J, Hächler S, Stalder K, Müller S, Schönberg S, Jent S. Allergene in unverpackten Lebensmitteln – welche Informationsvermittlung bevorzugen Betroffene? Allergologie. 2020;43:349–56. https://doi.org/10.5414/ALX02176.
Leftwich J, Barnett J, Muncer K, Shepherd R, Raats MM, Hazel Gowland M, et al. The challenges for nut-allergic consumers of eating out. Clin Exp Allergy. 2011;41:243–9. https://doi.org/10.1111/j.1365-2222.2010.03649.x.
Bailey S, Billmeier Kindratt T, Smith H, Reading D. Food allergy training event for restaurant staff; a pilot evaluation. Clin Transl Allergy. 2014;4:26. https://doi.org/10.1186/2045-7022-4-26.
Food Standards Agency. Allergy training for food businesses. 2020. https://www.food.gov.uk/business-guidance/allergy-training-for-food-businesses. Accessed 1 Oct 2021.
Pádua I, Moreira A, Moreira P, Barros R. Impact of a web-based program to improve food allergy management in schools and restaurants. Pediatr Allergy Immunol. 2020;31:851–7. https://doi.org/10.1111/pai.13264.
Allen KJ, Taylor SL. The consequences of precautionary allergen labeling: safe haven or unjustifiable burden? J Allergy Clin Immunol Pract. 2018;6:400–7. https://doi.org/10.1016/j.jaip.2017.12.025.
Trendelenburg V, Enzian N, Bellach J, Schnadt S, Niggemann B, Beyer K. Detection of relevant amounts of cow’s milk protein in non-pre-packed bakery products sold as cow’s milk-free. Allergy. 2015;70:591–7. https://doi.org/10.1111/all.12588.
Ballmer-Weber BK, Fernandez-Rivas M, Beyer K, Defernez M, Sperrin M, Mackie AR, et al. How much is too much? Threshold dose distributions for 5 food allergens. J Allergy Clin Immunol. 2015;135:964–71. https://doi.org/10.1016/j.jaci.2014.10.047.
Lebwohl B, Sanders DS, Green PHR. Coeliac disease. Lancet. 2018;391:70–81. https://doi.org/10.1016/S0140-6736(17)31796-8.
Swiss Association of Cantonal Chemists. Informationen zu Allergenen: Kantonschemiker bemängeln über die Hälfte der Betriebe. Lucerne: Swiss Association of Cantonal Chemists; 2019.
Acknowledgements
We would like to thank the Federal Food Safety and Veterinary Office (FSVO) for the financial support of this project and Corinne Mugny (FSVO) for her comments and constructive feedback on the first draft of this manuscript. Furthermore, our thanks go to Klazine van der Horst (BFH), who allowed internship students to work on this project and supported the project team with her knowledge and experience.
Funding
The project was financially supported by the Swiss Federal Food Safety and Veterinary Office (FSVO).
Funding
Open Access funding provided by Berner Fachhochschule BFH.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Gerry Schumacher, Loan Catalano, Marie Hirt, Janine Wild and Julia Eisenblätter. The first draft of the manuscript was written by Julia Eisenblätter and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
J. Eisenblätter, G. Schumacher, M. Hirt, J. Wild, L. Catalano, S. Schoenberg, B. Baru and S. Jent declare that they have no competing interests.
Ethical standards
In accordance with Article Two of the Swiss Human Research Act, requirements of ethical approval do not apply to this survey. Consent to participate: An email with relevant information on the study was sent to businesses prior to the interview, so that interviewees were able to give informed consent. Verbal informed consent was obtained prior to the interview. Consent for publication: n/a.
Additional information
Availability of data and code
The data and code that support the findings of this study are available upon reasonable request from the corresponding author.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eisenblätter, J., Schumacher, G., Hirt, M. et al. How do food businesses provide information on allergens in non-prepacked foods? A cross-sectional survey in Switzerland. Allergo J Int 31, 43–50 (2022). https://doi.org/10.1007/s40629-021-00191-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40629-021-00191-5