Abstract
Background
Severe hypertension may be a prominent manifestation of complement-mediated thrombotic microangiopathy. Furthermore, patients with severe hypertension-associated thrombotic microangiopathy may present with concurrent hematologic abnormalities that mimic complement-mediated thrombotic microangiopathy. Whether or not severe hypertension-associated thrombotic microangiopathy is associated with genetic susceptibility in complement- and/or coagulation-pathway genes remains unclear, and there is thus a need to identify clinicopathological clues to distinguish between these entities.
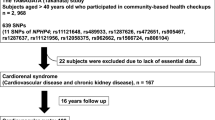
Methods
Forty-five patients with concomitant severe hypertension and thrombotic microangiopathy on kidney biopsy were identified retrospectively. Whole-exome sequencing was performed to identify rare variants in 29 complement- and coagulation-cascade genes. Clinicopathological features were compared between patients with severe hypertension-associated thrombotic microangiopathy and complement-mediated thrombotic microangiopathy with severe hypertension.
Results
Three patients with pathogenic variants diagnostic of complement-mediated thrombotic microangiopathy and two with anti-factor H antibody positivity were diagnosed with complement-mediated thrombotic microangiopathy with severe hypertension. Among the 40 patients with severe hypertension-associated thrombotic microangiopathy, 53 rare variants of uncertain significance were found in the analyzed genes in 34 (34/40, 85%) patients, of whom 12 patients harbored two or more variants. Compared with complement-mediated thrombotic microangiopathy patients with severe hypertension, patients with severe hypertension-associated thrombotic microangiopathy were more likely to have left ventricular wall thickening (p < 0.001), less-severe acute glomerular thrombotic microangiopathy lesions including mesangiolysis and subendothelial space widening (both p < 0.001), and less arteriolar thrombosis formation (p < 0.001).
Conclusions
Rare genetic variants involving complement and coagulation pathways can be found in patients with severe hypertension-associated thrombotic microangiopathy; their role needs further investigation. Cardiac remodeling and acute glomerular TMA lesions may help to differentiate between severe hypertension-associated thrombotic microangiopathy and complement-mediated thrombotic microangiopathy with severe hypertension.
Graphical Abstract




Similar content being viewed by others
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
George JN, Nester CM (2014) Syndromes of thrombotic microangiopathy. N Engl J Med 371(7):654–666. https://doi.org/10.1056/NEJMra1312353
Fakhouri F, Zuber J, Frémeaux-Bacchi V, Loirat C (2017) Haemolytic uraemic syndrome. Lancet 390(10095):681–696. https://doi.org/10.1016/s0140-6736(17)30062-4
Legendre CM, Licht C, Muus P, Greenbaum LA, Babu S, Bedrosian C, Bingham C, Cohen DJ, Delmas Y, Douglas K, Eitner F, Feldkamp T, Fouque D, Furman RR, Gaber O, Herthelius M, Hourmant M, Karpman D, Lebranchu Y, Mariat C, Menne J, Moulin B, Nürnberger J, Ogawa M, Remuzzi G, Richard T, Sberro-Soussan R, Severino B, Sheerin NS, Trivelli A, Zimmerhackl LB, Goodship T, Loirat C (2013) Terminal complement inhibitor eculizumab in atypical hemolytic-uremic syndrome. N Engl J Med 368(23):2169–2181. https://doi.org/10.1056/NEJMoa1208981
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 71(19):e127–e248. https://doi.org/10.1016/j.jacc.2017.11.006
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I (2018) 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens 36(10):1953–2041. https://doi.org/10.1097/hjh.0000000000001940
Cremer A, Amraoui F, Lip GY, Morales E, Rubin S, Segura J, Van den Born BJ, Gosse P (2016) From malignant hypertension to hypertension-MOD: a modern definition for an old but still dangerous emergency. J Hum Hypertens 30(8):463–466. https://doi.org/10.1038/jhh.2015.112
Mishima E, Funayama Y, Suzuki T, Mishima F, Nitta F, Toyohara T, Kikuchi K, Kunikata H, Hashimoto J, Miyazaki M, Harigae H, Nakazawa T, Ito S, Abe T (2021) Concurrent analogous organ damage in the brain, eyes, and kidneys in malignant hypertension: reversible encephalopathy, serous retinal detachment, and proteinuria. Hypertens Res 44(1):88–97. https://doi.org/10.1038/s41440-020-0521-2
Shantsila A, Dwivedi G, Shantsila E, Butt M, Beevers DG, Lip GY (2011) Persistent macrovascular and microvascular dysfunction in patients with malignant hypertension. Hypertension 57(3):490–496. https://doi.org/10.1161/hypertensionaha.110.166314
Sallée M, Ismail K, Fakhouri F, Vacher-Coponat H, Moussi-Francés J, Frémaux-Bacchi V, Burtey S (2013) Thrombocytopenia is not mandatory to diagnose haemolytic and uremic syndrome. BMC Nephrol 14:3. https://doi.org/10.1186/1471-2369-14-3
Cavero T, Arjona E, Soto K, Caravaca-Fontán F, Rabasco C, Bravo L, de la Cerda F, Martín N, Blasco M, Ávila A, Huerta A, Cabello V, Jarque A, Alcázar C, Fulladosa X, Carbayo J, Anaya S, Cobelo C, Ramos N, Iglesias E, Baltar J, Martínez-Gallardo R, Pérez L, Morales E, González R, Macía M, Draibe J, Pallardó L, Quintana LF, Espinosa M, Barros X, Pereira F, Cao M, Moreno JA, Rodríguez de Córdoba S, Praga M (2019) Severe and malignant hypertension are common in primary atypical hemolytic uremic syndrome. Kidney Int 96(4):995–1004. https://doi.org/10.1016/j.kint.2019.05.014
van den Born BJ, Honnebier UP, Koopmans RP, van Montfrans GA (2005) Microangiopathic hemolysis and renal failure in malignant hypertension. Hypertension 45(2):246–251. https://doi.org/10.1161/01.HYP.0000151620.17905.ee
Timmermans S, Abdul-Hamid MA, Vanderlocht J, Damoiseaux J, Reutelingsperger CP, van Paassen P (2017) Patients with hypertension-associated thrombotic microangiopathy may present with complement abnormalities. Kidney Int 91(6):1420–1425. https://doi.org/10.1016/j.kint.2016.12.009
Timmermans S, Abdul-Hamid MA, Potjewijd J, Theunissen R, Damoiseaux J, Reutelingsperger CP, van Paassen P (2018) C5b9 formation on endothelial cells reflects complement defects among patients with renal thrombotic microangiopathy and severe hypertension. J Am Soc Nephrol 29(8):2234–2243. https://doi.org/10.1681/asn.2018020184
Timmermans S, Wérion A, Damoiseaux J, Morelle J, Reutelingsperger CP, van Paassen P (2020) Diagnostic and risk factors for complement defects in hypertensive emergency and thrombotic microangiopathy. Hypertension 75(2):422–430. https://doi.org/10.1161/hypertensionaha.119.13714
Zhang Y, Yang C, Zhou X, Hu R, Quan S, Zhou Y, Li Y, Xing G (2020) Association between thrombotic microangiopathy and activated alternative complement pathway in malignant nephrosclerosis. Nephrol Dial Transplant. https://doi.org/10.1093/ndt/gfaa280
Larsen CP, Wilson JD, Best-Rocha A, Beggs ML, Hennigar RA (2018) Genetic testing of complement and coagulation pathways in patients with severe hypertension and renal microangiopathy. Mod Pathol 31(3):488–494. https://doi.org/10.1038/modpathol.2017.154
Li H, Durbin R (2009) Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25(14):1754–1760. https://doi.org/10.1093/bioinformatics/btp324
Tarasov A, Vilella AJ, Cuppen E, Nijman IJ, Prins P (2015) Sambamba: fast processing of NGS alignment formats. Bioinformatics 31(12):2032–2034. https://doi.org/10.1093/bioinformatics/btv098
Wang K, Li M, Hakonarson H (2010) ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res 38(16):e164. https://doi.org/10.1093/nar/gkq603
Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, Marchini JL, McCarthy S, McVean GA, Abecasis GR (2015) A global reference for human genetic variation. Nature 526(7571):68–74. https://doi.org/10.1038/nature15393
Kumar P, Henikoff S, Ng PC (2009) Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc 4(7):1073–1081. https://doi.org/10.1038/nprot.2009.86
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, Kondrashov AS, Sunyaev SR (2010) A method and server for predicting damaging missense mutations. Nat Methods 7(4):248–249. https://doi.org/10.1038/nmeth0410-248
Schwarz JM, Rödelsperger C, Schuelke M, Seelow D (2010) MutationTaster evaluates disease-causing potential of sequence alterations. Nat Methods 7(8):575–576. https://doi.org/10.1038/nmeth0810-575
Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J (2014) A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet 46(3):310–315. https://doi.org/10.1038/ng.2892
Muona M, Berkovic SF, Dibbens LM, Oliver KL, Maljevic S, Bayly MA, Joensuu T, Canafoglia L, Franceschetti S, Michelucci R, Markkinen S, Heron SE, Hildebrand MS, Andermann E, Andermann F, Gambardella A, Tinuper P, Licchetta L, Scheffer IE, Criscuolo C, Filla A, Ferlazzo E, Ahmad J, Ahmad A, Baykan B, Said E, Topcu M, Riguzzi P, King MD, Ozkara C, Andrade DM, Engelsen BA, Crespel A, Lindenau M, Lohmann E, Saletti V, Massano J, Privitera M, Espay AJ, Kauffmann B, Duchowny M, Møller RS, Straussberg R, Afawi Z, Ben-Zeev B, Samocha KE, Daly MJ, Petrou S, Lerche H, Palotie A, Lehesjoki AE (2015) A recurrent de novo mutation in KCNC1 causes progressive myoclonus epilepsy. Nat Genet 47(1):39–46. https://doi.org/10.1038/ng.3144
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17(5):405–424. https://doi.org/10.1038/gim.2015.30
Van Laecke S, Van Biesen W (2017) Severe hypertension with renal thrombotic microangiopathy: what happened to the usual suspect? Kidney Int 91(6):1271–1274. https://doi.org/10.1016/j.kint.2017.02.025
Fremeaux-Bacchi V, Fakhouri F, Garnier A, Bienaimé F, Dragon-Durey MA, Ngo S, Moulin B, Servais A, Provot F, Rostaing L, Burtey S, Niaudet P, Deschênes G, Lebranchu Y, Zuber J, Loirat C (2013) Genetics and outcome of atypical hemolytic uremic syndrome: a nationwide French series comparing children and adults. Clin J Am Soc Nephrol 8(4):554–562. https://doi.org/10.2215/cjn.04760512
Noris M, Remuzzi G (2009) Atypical hemolytic-uremic syndrome. N Engl J Med 361(17):1676–1687. https://doi.org/10.1056/NEJMra0902814
Noris M, Caprioli J, Bresin E, Mossali C, Pianetti G, Gamba S, Daina E, Fenili C, Castelletti F, Sorosina A, Piras R, Donadelli R, Maranta R, van der Meer I, Conway EM, Zipfel PF, Goodship TH, Remuzzi G (2010) Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype. Clin J Am Soc Nephrol 5(10):1844–1859. https://doi.org/10.2215/cjn.02210310
Bu F, Borsa NG, Jones MB, Takanami E, Nishimura C, Hauer JJ, Azaiez H, Black-Ziegelbein EA, Meyer NC, Kolbe DL, Li Y, Frees K, Schnieders MJ, Thomas C, Nester C, Smith RJ (2016) High-Throughput genetic testing for thrombotic microangiopathies and C3 glomerulopathies. J Am Soc Nephrol 27(4):1245–1253. https://doi.org/10.1681/asn.2015040385
Osborne AJ, Breno M, Borsa NG, Bu F, Frémeaux-Bacchi V, Gale DP, van den Heuvel LP, Kavanagh D, Noris M, Pinto S, Rallapalli PM, Remuzzi G, Rodríguez de Cordoba S, Ruiz A, Smith RJH, Vieira-Martins P, Volokhina E, Wilson V, Goodship THJ, Perkins SJ (2018) Statistical validation of rare complement variants provides insights into the molecular basis of atypical hemolytic uremic syndrome and C3 glomerulopathy. J Immunol 200(7):2464–2478. https://doi.org/10.4049/jimmunol.1701695
El Karoui K, Boudhabhay I, Petitprez F, Vieira-Martins P, Fakhouri F, Zuber J, Aulagnon F, Matignon M, Rondeau E, Mesnard L, Halimi JM, Frémeaux-Bacchi V (2019) Impact of hypertensive emergency and rare complement variants on the presentation and outcome of atypical hemolytic uremic syndrome. Haematologica 104(12):2501–2511. https://doi.org/10.3324/haematol.2019.216903
Schaefer F, Ardissino G, Ariceta G, Fakhouri F, Scully M, Isbel N, Lommelé Å, Kupelian V, Gasteyger C, Greenbaum LA, Johnson S, Ogawa M, Licht C, Vande Walle J, Frémeaux-Bacchi V (2018) Clinical and genetic predictors of atypical hemolytic uremic syndrome phenotype and outcome. Kidney Int 94(2):408–418. https://doi.org/10.1016/j.kint.2018.02.029
Fakhouri F, Frémeaux-Bacchi V (2021) Thrombotic microangiopathy in aHUS and beyond: clinical clues from complement genetics. Nat Rev Nephrol 17(8):543–553. https://doi.org/10.1038/s41581-021-00424-4
Zhang B, Xing C, Yu X, Sun B, Zhao X, Qian J (2008) Renal thrombotic microangiopathies induced by severe hypertension. Hypertens Res 31(3):479–483. https://doi.org/10.1291/hypres.31.479
Johnson W, Nguyen ML, Patel R (2012) Hypertension crisis in the emergency department. Cardiol Clin 30(4):533–543. https://doi.org/10.1016/j.ccl.2012.07.011
Rubin S, Cremer A, Boulestreau R, Rigothier C, Kuntz S, Gosse P (2019) Malignant hypertension: diagnosis, treatment and prognosis with experience from the Bordeaux cohort. J Hypertens 37(2):316–324. https://doi.org/10.1097/hjh.0000000000001913
Lane DA, Lip GY, Beevers DG (2009) Improving survival of malignant hypertension patients over 40 years. Am J Hypertens 22(11):1199–1204. https://doi.org/10.1038/ajh.2009.153
Polgreen LA, Suneja M, Tang F, Carter BL, Polgreen PM (2015) Increasing trend in admissions for malignant hypertension and hypertensive encephalopathy in the United States. Hypertension 65(5):1002–1007. https://doi.org/10.1161/hypertensionaha.115.05241
Shantsila A, Shantsila E, Beevers DG, Lip GYH (2017) Predictors of 5-year outcomes in malignant phase hypertension: the West Birmingham Malignant Hypertension Registry. J Hypertens 35(11):2310–2314. https://doi.org/10.1097/hjh.0000000000001446
Acknowledgements
We thank Richard Robins, PhD, and Susan Furness, PhD, from Liwen Bianji (Edanz) (www.liwenbianji.cn) for editing the English text of a draft of this manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (Nos. 81770671 and 82090021).
Author information
Authors and Affiliations
Contributions
YW conceived and designed research; XC collected and analyzed data, prepared figures and drafted manuscripts; XZ and SW reviewed kidney biopsy; MZ edited and revised manuscript; all authors approved final version.
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethics approval
This study adhered to the principles outlined in the Declaration of Helsinki for all human experimental investigations. Animal experiments were not involved and this study was approved by the Committee on Research Ethics of Peking University First Hospital (2017[1280]).
Informed consent
Written informed consent was obtained from each patient and the copy of the written consent is available upon request.
Consent for publication
Informed written consent was obtained from each patient for publication of their collected and analyzed data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, X., Zhang, X., Wang, Y. et al. Genetic, clinical, and pathological study of patients with severe hypertension-associated renal microangiopathy. J Nephrol 36, 2477–2490 (2023). https://doi.org/10.1007/s40620-023-01644-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-023-01644-6