Abstract
Purpose
Papillary thyroid microcarcinoma (PTMC) frequently presents a favorable clinical outcome, while aggressive invasiveness can also be found in some of this population. Identifying the risk clinical factors of high-volume (> 5) central lymph node metastasis (CLNM) in PTMC patients could help oncologists make a better-individualized clinical decision.
Methods
We retrospectively reviewed the clinical characteristics of adult patients with PTC in the Surveillance, Epidemiology, and End Results (SEER) database between Jan 2010 and Dec 2015 and in one medical center affiliated to Chongqing Medical University between Jan 2018 and Oct 2020. Univariate and multivariate logistic regression analyses were used to determine the risk factors for high volume of CLNM in PTMC patients.
Results
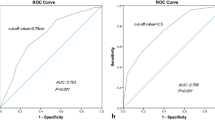
The male gender (OR = 2.02, 95% CI 1.46–2.81), larger tumor size (> 5 mm, OR = 1.64, 95% CI 1.13–2.38), multifocality (OR = 1.87, 95% CI 1.40–2.51), and extrathyroidal invasion (OR = 3.67; 95% CI 2.64–5.10) were independent risk factors in promoting high-volume of CLNM in PTMC patients. By contrast, elderly age (≥ 55 years) at diagnosis (OR = 0.57, 95% CI 0.40–0.81) and PTMC-follicular variate (OR = 0.60, 95% CI 0.42–0.87) were determined as the protective factors. Based on these indicators, a nomogram was further constructed with a good concordance index (C-index) of 0.702, supported by an external validating cohort with a promising C-index of 0.811.
Conclusion
A nomogram was successfully established and validated with six clinical indicators. This model could help surgeons to make a better-individualized clinical decision on the management of PTMC patients, especially in terms of whether prophylactic central lymph node dissection and postoperative radiotherapy should be warranted.



Similar content being viewed by others
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
The software application generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Roman BR, Morris LG, Davies L (2017) The thyroid cancer epidemic, 2017 perspective. Curr Opin Endocrinol Diabetes Obes 24(5):332–336. https://doi.org/10.1097/med.0000000000000359
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70(1):7–30. https://doi.org/10.3322/caac.21590
Wang J, Yu F, Shang Y, Ping Z, Liu L (2020) Thyroid cancer: incidence and mortality trends in China, 2005–2015. Endocrine 68(1):163–173. https://doi.org/10.1007/s12020-020-02207-6
Casella C, Ministrini S, Galani A, Mastriale F, Cappelli C, Portolani N (2018) The new TNM staging system for thyroid cancer and the risk of disease downstaging. Front Endocrinol (Lausanne) 9:541. https://doi.org/10.3389/fendo.2018.00541
Tuttle RM, Haugen B, Perrier ND (2017) Updated American Joint Committee on Cancer/tumor-node-metastasis staging system for differentiated and anaplastic thyroid cancer (eighth edition): what changed and why? Thyroid 27(6):751–756. https://doi.org/10.1089/thy.2017.0102
Calò PG, Lombardi CP, Podda F, Sessa L, Santini L, Conzo G (2017) Role of prophylactic central neck dissection in clinically node-negative differentiated thyroid cancer: assessment of the risk of regional recurrence. Updates Surg 69(2):241–248. https://doi.org/10.1007/s13304-017-0438-8
Lang BH, Ng SH, Lau LL, Cowling BJ, Wong KP, Wan KY (2013) A systematic review and meta-analysis of prophylactic central neck dissection on short-term locoregional recurrence in papillary thyroid carcinoma after total thyroidectomy. Thyroid 23(9):1087–1098. https://doi.org/10.1089/thy.2012.0608
Moo TA, McGill J, Allendorf J, Lee J, Fahey T 3rd, Zarnegar R (2010) Impact of prophylactic central neck lymph node dissection on early recurrence in papillary thyroid carcinoma. World J Surg 34(6):1187–1191. https://doi.org/10.1007/s00268-010-0418-3
Ryu YJ, Yoon JH (2020) Impact of prophylactic unilateral central neck dissection needed for patients with papillary thyroid microcarcinoma. Gland Surg 9(2):352–361. https://doi.org/10.21037/gs.2020.03.03
Viola D, Materazzi G, Valerio L, Molinaro E, Agate L, Faviana P, Seccia V, Sensi E, Romei C, Piaggi P, Torregrossa L, Sellari-Franceschini S, Basolo F, Vitti P, Elisei R, Miccoli P (2015) Prophylactic central compartment lymph node dissection in papillary thyroid carcinoma: clinical implications derived from the first prospective randomized controlled single institution study. J Clin Endocrinol Metab 100(4):1316–1324. https://doi.org/10.1210/jc.2014-3825
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward DL, Tuttle RM, Wartofsky L (2016) 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1):1–133. https://doi.org/10.1089/thy.2015.0020
Jeon MJ, Kim WG, Chung KW, Baek JH, Kim WB, Shong YK (2019) Active surveillance of papillary thyroid microcarcinoma: where do we stand? Eur Thyroid J 8(6):298–306. https://doi.org/10.1159/000503064
Jeon MJ, Lee YM, Sung TY, Han M, Shin YW, Kim WG, Kim TY, Chung KW, Shong YK, Kim WB (2019) Quality of life in patients with papillary thyroid microcarcinoma managed by active surveillance or lobectomy: a cross-sectional study. Thyroid 29(7):956–962. https://doi.org/10.1089/thy.2018.0711
Davies L, Roman BR, Fukushima M, Ito Y, Miyauchi A (2019) Patient experience of thyroid cancer active surveillance in Japan. JAMA Otolaryngol Head Neck Surg 145(4):363–370. https://doi.org/10.1001/jamaoto.2018.4131
Oh HS, Ha J, Kim HI, Kim TH, Kim WG, Lim DJ, Kim TY, Kim SW, Kim WB, Shong YK, Chung JH, Baek JH (2018) Active surveillance of low-risk papillary thyroid microcarcinoma: a multi-center cohort study in Korea. Thyroid 28(12):1587–1594. https://doi.org/10.1089/thy.2018.0263
Sugitani I, Ito Y, Takeuchi D, Nakayama H, Masaki C, Shindo H, Teshima M, Horiguchi K, Yoshida Y, Kanai T, Hirokawa M, Hames KY, Tabei I, Miyauchi A (2020) Indications and strategy for active surveillance of adult low-risk papillary thyroid microcarcinoma: consensus statements from the japan association of endocrine surgery task force on management for papillary thyroid microcarcinoma. Thyroid. https://doi.org/10.1089/thy.2020.0330
Ito Y, Miyauchi A, Oda H (2018) Low-risk papillary microcarcinoma of the thyroid: a review of active surveillance trials. Eur J Surg Oncol 44(3):307–315. https://doi.org/10.1016/j.ejso.2017.03.004
Koshkina A, Fazelzad R, Sugitani I, Miyauchi A, Thabane L, Goldstein DP, Ghai S, Sawka AM (2020) Association of patient age with progression of low-risk papillary thyroid carcinoma under active surveillance: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg 146(6):552–560. https://doi.org/10.1001/jamaoto.2020.0368
Huang J, Song M, Shi H, Huang Z, Wang S, Yin Y, Huang Y, Du J, Wang S, Liu Y, Wu Z (2021) Predictive factor of large-volume central lymph node metastasis in clinical n0 papillary thyroid carcinoma patients underwent total thyroidectomy. Front Oncol 11:574774. https://doi.org/10.3389/fonc.2021.574774
Huang XP, Ye TT, Zhang L, Liu RF, Lai XJ, Wang L, Yang M, Zhang B, Li XY, Liu ZW, Xia Y, Jiang YX (2018) Sonographic features of papillary thyroid microcarcinoma predicting high-volume central neck lymph node metastasis. Surg Oncol 27(2):172–176. https://doi.org/10.1016/j.suronc.2018.03.004
Raue F, Frank-Raue K (2016) Thyroid cancer: risk-stratified management and individualized therapy. Clin Cancer Res 22(20):5012–5021
Jung KW, Won YJ, Hong S, Kong HJ, Lee ES (2020) Prediction of cancer incidence and mortality in Korea, 2020. Cancer Res Treat 52(2):351–358. https://doi.org/10.4143/crt.2020.203
Zhai M, Zhang D, Long J, Gong Y, Ye F, Liu S, Li Y (2021) The global burden of thyroid cancer and its attributable risk factor in 195 countries and territories: a systematic analysis for the Global Burden of Disease Study. Cancer Med. https://doi.org/10.1002/cam4.3970
Yan B, Hou Y, Chen D, He J, Jiang Y (2018) Risk factors for contralateral central lymph node metastasis in unilateral cN0 papillary thyroid carcinoma: a meta-analysis. Int J Surg 59:90–98. https://doi.org/10.1016/j.ijsu.2018.09.004
Feng JW, Ye J, Wu WX, Qu Z, Qin AC, Jiang Y (2020) Management of cN0 papillary thyroid microcarcinoma patients according to risk-scoring model for central lymph node metastasis and predictors of recurrence. J Endocrinol Invest. https://doi.org/10.1007/s40618-020-01326-1
Sun W, Zheng B, Wang Z, Dong W, Qin Y, Zhang H (2020) Meta-analysis of risk factors for CCLNM in patients with unilateral cN0 PTC. Endocr Connect 9(5):387–395. https://doi.org/10.1530/ec-20-0058
Kim E, Park JS, Son KR, Kim JH, Jeon SJ, Na DG (2008) Preoperative diagnosis of cervical metastatic lymph nodes in papillary thyroid carcinoma: comparison of ultrasound, computed tomography, and combined ultrasound with computed tomography. Thyroid 18(4):411–418. https://doi.org/10.1089/thy.2007.0269
Kim SK, Park I, Woo JW, Lee JH, Choe JH, Kim JH, Kim JS (2016) Predictive factors for lymph node metastasis in papillary thyroid microcarcinoma. Ann Surg Oncol 23(9):2866–2873. https://doi.org/10.1245/s10434-016-5225-0
Zhou SC, Liu TT, Zhou J, Huang YX, Guo Y, Yu JH, Wang YY, Chang C (2020) An ultrasound radiomics nomogram for preoperative prediction of central neck lymph node metastasis in papillary thyroid carcinoma. Front Oncol 10:1591. https://doi.org/10.3389/fonc.2020.01591
Zhao W, He L, Zhu J, Su A (2020) A nomogram model based on the preoperative clinical characteristics of papillary thyroid carcinoma with Hashimoto’s thyroiditis to predict central lymph node metastasis. Clin Endocrinol (Oxf). https://doi.org/10.1111/cen.14302
Yang Z, Heng Y, Lin J, Lu C, Yu D, Tao L, Cai W (2020) Nomogram for predicting central lymph node metastasis in papillary thyroid cancer: a retrospective cohort study of two clinical centers. Cancer Res Treat 52(4):1010–1018. https://doi.org/10.4143/crt.2020.254
Tian X, Song Q, Xie F, Ren L, Zhang Y, Tang J, Zhang Y, Jin Z, Zhu Y, Zhang M, Luo Y (2020) Papillary thyroid carcinoma: an ultrasound-based nomogram improves the prediction of lymph node metastases in the central compartment. Eur Radiol 30(11):5881–5893. https://doi.org/10.1007/s00330-020-06906-6
Feng Y, Min Y, Chen H, Xiang K, Wang X, Yin G (2021) Construction and validation of a nomogram for predicting cervical lymph node metastasis in classic papillary thyroid carcinoma. J Endocrinol Invest. https://doi.org/10.1007/s40618-021-01524-5
Xu J, Zhang Y, Liu J, Qiu S, Wang M (2021) A population-based study of the three major variants of papillary thyroid carcinoma. J Int Med Res 49(2):300060520984618. https://doi.org/10.1177/0300060520984618
Thompson AM, Turner RM, Hayen A, Aniss A, Jalaty S, Learoyd DL, Sidhu S, Delbridge L, Yeh MW, Clifton-Bligh R, Sywak M (2014) A preoperative nomogram for the prediction of ipsilateral central compartment lymph node metastases in papillary thyroid cancer. Thyroid 24(4):675–682. https://doi.org/10.1089/thy.2013.0224
Acknowledgements
We acknowledged Dr. Shenghao Fan for the substantial contribution to thyroid surgery in our department. We also thank the designers of “Hiplot” software for drawing figures. Also, we acknowledge the contributions of the Surveillance, Epidemiology, and End Results (SEER) Program registries for creating and updating the SEER database.
Funding
This work was supported by the National Natural Science Foundation of China (NSFC No. 81972460) for Guobing Yin.
Author information
Authors and Affiliations
Contributions
(I) Conception and design: YM, XW, GY, DH. (II) Administrative support: GY, DH. (III) Provision of study materials or patients: XW, YF, HC, YM. (IV) Collection and assembly of data: DH, YH, XZ, YM, JC, KX. (V) Data analysis and interpretation: YM, HL, XW. (VI) Manuscript writing: all authors. (VII) Final approval of manuscript: all authors.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was waived by the local Ethics Committee of the Chongqing Medical University in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Informed consent
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wei, X., Min, Y., Feng, Y. et al. Development and validation of an individualized nomogram for predicting the high-volume (> 5) central lymph node metastasis in papillary thyroid microcarcinoma. J Endocrinol Invest 45, 507–515 (2022). https://doi.org/10.1007/s40618-021-01675-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-021-01675-5