Abstract
Introduction
Metabolic syndrome (MetS) is associated with an increased risk of major cardiovascular events. In women, increased serum uric acid (SUA) levels are associated with MetS and its components. However, whether baseline and changes in SUA predict incidence of MetS and its components remains unclear.
Methods
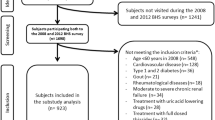
The subjects comprised 407 women aged 71 ± 8 years from a rural village. We have identified participants who underwent a similar examination 11 years ago, and examined the relationship between baseline and changes in SUA, and MetS based on the modified criteria of the National Cholesterol Education Program’s Adult Treatment Panel (NCEP-ATP) III report.
Results
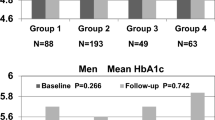
Of these subjects, 83 (20.4%) women at baseline and 190 (46.7%) women at follow-up had MetS. Multiple linear regression analysis was performed to evaluate the contribution of each confounding factor for MetS; both baseline and changes in SUA as well as history of cardiovascular disease, low-density lipoprotein cholesterol, and estimated glomerular filtration ratio (eGFR) were independently and significantly associated with the number of MetS components during an 11-year follow-up. The adjusted odds ratios (ORs) (95% confidence interval) for incident MetS across tertiles of baseline SUA and changes in SUA were 1.00, 1.47 (0.82–2.65), and 3.11 (1.66–5.83), and 1.00, 1.88 (1.03–3.40), and 2.49 (1.38–4.47), respectively. In addition, the combined effect between increased baseline and changes in SUA was also a significant and independent determinant for the accumulation of MetS components (F = 20.29, p < 0.001). The ORs for incident MetS were significant only in subjects with age ≥ 55 years, decline in eGFR, and no baseline MetS.
Conclusions
These results suggested that combined assessment of baseline and changes in SUA levels provides increased information for incident MetS, independent of other confounding factors in community-dwelling women.

Similar content being viewed by others
References
Lorenzo C, Okoloise M, Williams K, Stern MP, Haffner SM (2003) The metabolic syndrome as predictor of type 2 diabetes: the San Antonio heart study. Diabetes Care 26:3153–3159
McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, Ballantyne CM, Heiss G (2005) The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care 28:385–390
Shiwaku K, Nogi A, Kitajima K, Anuurad E, Enkhmaa B, Yamasaki M, Kim JM, Kim IS, Lee SK, Oyunsuren T, Yamane Y (2005) Prevalence of the metabolic syndrome using the modified ATP III definitions for workers in Japan, Korea and Mongolia. J Occup Health 47:126–135
Popa S, Mota M, Popa A, Mota E, Serafinceanu C, Guja C, Catrinoiu D, Hancu N, Lichiardopol R, Bala C, Popa A, Roman G, Radulian G, Timar R, Mihai B (2016) Prevalence of overweight/obesity, abdominal obesity and metabolic syndrome and atypical cardiometabolic phenotypes in the adult Romanian population: PREDATORR study. J Endocrinol Invest 39:1045–1053. https://doi.org/10.1007/s40618-016-0470-4
Kawamoto R, Tomita H, Oka Y, Ohtsuka N (2006) Relationship between serum uric acid concentration, metabolic syndrome and carotid atherosclerosis. Intern Med 45:605–614
Lee JM, Kim HC, Cho HM, Oh SM, Choi DP, Suh I (2012) Association between serum uric acid level and metabolic syndrome. J Prev Med Public Health 45:181–187. https://doi.org/10.3961/jpmph.2012.45.3.181
Ziaee A, Esmailzadehha N, Ghorbani A, Asefzadeh S (2012) Association between uric acid and metabolic syndrome in Qazvin Metabolic Diseases Study (QMDS) Iran. Glob J Health Sci 5:155–165. https://doi.org/10.5539/gjhs.v5n1p155
Sui X, Church TS, Meriwether RA, Lobelo F, Blair SN (2008) Uric acid and the development of metabolic syndrome in women and men. Metabolism 57:845–852. https://doi.org/10.1016/j.metabol.2008.01.030
Yang T, Chu CH, Bai CH, You SL, Chou YC, Chou WY, Chien KL, Hwang LC, Su TC, Tseng CH, Sun CA (2012) Uric acid level as a risk marker for metabolic syndrome: a Chinese cohort study. Atherosclerosis 220:525–531. https://doi.org/10.1016/j.atherosclerosis.2011.11.014
Goncalves JP, Oliveira A, Severo M, Santos AC, Lopes C (2012) Cross-sectional and longitudinal associations between serum uric acid and metabolic syndrome. Endocrine 41:450–457. https://doi.org/10.1007/s12020-012-9629-8
Zhang ML, Gao YX, Wang X, Chang H, Huang GW (2013) Serum uric acid and appropriate cutoff value for prediction of metabolic syndrome among Chinese adults. J Clin Biochem Nutr 52:38–42. https://doi.org/10.3164/jcbn.12-65
Oda E (2014) Serum uric acid is an independent predictor of metabolic syndrome in a Japanese health screening population. Heart Vessels 29:496–503. https://doi.org/10.1007/s00380-013-0386-2
Zurlo A, Veronese N, Giantin V, Maselli M, Zambon S, Maggi S, Musacchio E, Toffanello ED, Sartori L, Perissinotto E, Crepaldi G, Manzato E, Sergi G (2016) High serum uric acid levels increase the risk of metabolic syndrome in elderly women: the PROVA study. Nutr Metab Cardiovasc Dis 26:27–35. https://doi.org/10.1016/j.numecd.2015.10.007
Cicero AF, Salvi P, D’Addato S, Rosticci M, Borghi C (2014) Association between serum uric acid, hypertension, vascular stiffness and subclinical atherosclerosis: data from the Brisighella Heart Study. J Hypertens 32:57–64. https://doi.org/10.1097/HJH.0b013e328365b916
Norvik JV, Storhaug HM, Ytrehus K, Jenssen TG, Zykova SN, Eriksen BO, Solbu MD (2016) Overweight modifies the longitudinal association between uric acid and some components of the metabolic syndrome: The Tromso Study. BMC Cardiovasc Disord 16:85. https://doi.org/10.1186/s12872-016-0265-8
Nakanishi N, Okamoto M, Yoshida H, Matsuo Y, Suzuki K, Tatara K (2003) Serum uric acid and risk for development of hypertension and impaired fasting glucose or Type II diabetes in Japanese male office workers. Eur J Epidemiol 18:523–530
Filiopoulos V, Hadjiyannakos D, Vlassopoulos D (2012) New insights into uric acid effects on the progression and prognosis of chronic kidney disease. Ren Fail 34:510–520. https://doi.org/10.3109/0886022x.2011.653753
Bickel C, Rupprecht HJ, Blankenberg S, Rippin G, Hafner G, Daunhauer A, Hofmann KP, Meyer J (2002) Serum uric acid as an independent predictor of mortality in patients with angiographically proven coronary artery disease. Am J Cardiol 89:12–17
Johnson RJ, Kang DH, Feig D, Kivlighn S, Kanellis J, Watanabe S, Tuttle KR, Rodriguez-Iturbe B, Herrera-Acosta J, Mazzali M (2003) Is there a pathogenetic role for uric acid in hypertension and cardiovascular and renal disease? Hypertension 41:1183–1190. https://doi.org/10.1161/01.hyp.0000069700.62727.c5
Glantzounis GK, Tsimoyiannis EC, Kappas AM, Galaris DA (2005) Uric acid and oxidative stress. Curr Pharm Des 11:4145–4151
Kawamoto R, Ninomiya D, Kasai Y, Kusunoki T, Ohtsuka N, Kumagi T, Abe M (2016) Serum uric acid is positively associated with handgrip strength among Japanese community-dwelling elderly women. PLoS One 11:e0151044. https://doi.org/10.1371/journal.pone.0151044
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S (2010) Modification of the CKD epidemiology collaboration (CKD-EPI) equation for Japanese: accuracy and use for population estimates. Am J Kidney Dis 56:32–38. https://doi.org/10.1053/j.ajkd.2010.02.344
Kahn R, Buse J, Ferrannini E, Stern M (2005) The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 28:2289–2304
Ota T, Takamura T, Hirai N, Kobayashi K (2002) Preobesity in World Health Organization classification involves the metabolic syndrome in Japanese. Diabetes Care 25:1252–1253
Doi Y, Ninomiya T, Hata J, Yonemoto K, Arima H, Kubo M, Tanizaki Y, Iwase M, Iida M, Kiyohara Y (2009) Proposed criteria for metabolic syndrome in Japanese based on prospective evidence: the Hisayama study. Stroke 40:1187–1194. https://doi.org/10.1161/strokeaha.108.531319
Tsouli SG, Liberopoulos EN, Mikhailidis DP, Athyros VG, Elisaf MS (2006) Elevated serum uric acid levels in metabolic syndrome: an active component or an innocent bystander? Metabolism 55:1293–1301. https://doi.org/10.1016/j.metabol.2006.05.013
Ruggiero C, Cherubini A, Ble A, Bos AJ, Maggio M, Dixit VD, Lauretani F, Bandinelli S, Senin U, Ferrucci L (2006) Uric acid and inflammatory markers. Eur Heart J 27:1174–1181. https://doi.org/10.1093/eurheartj/ehi879
Hosseinzadeh-Attar MJ, Golpaie A, Foroughi M, Hosseinpanah F, Zahediasl S, Azizi F (2016) The relationship between visfatin and serum concentrations of C-reactive protein, interleukin 6 in patients with metabolic syndrome. J Endocrinol Invest 39:917–922. https://doi.org/10.1007/s40618-016-0457-1
Wang T, Bi Y, Xu M, Huang Y, Xu Y, Li X, Wang W, Ning G (2011) Serum uric acid associates with the incidence of type 2 diabetes in a prospective cohort of middle-aged and elderly Chinese. Endocrine 40:109–116. https://doi.org/10.1007/s12020-011-9449-2
McArdle MA, Finucane OM, Connaughton RM, McMorrow AM, Roche HM (2013) Mechanisms of obesity-induced inflammation and insulin resistance: insights into the emerging role of nutritional strategies. Front Endocrinol (Lausanne) 4:52. https://doi.org/10.3389/fendo.2013.00052
Kanabrocki EL, Third JL, Ryan MD, Nemchausky BA, Shirazi P, Scheving LE, McCormick JB, Hermida RC, Bremner WF, Hoppensteadt DA, Fareed J, Olwin JH (2000) Circadian relationship of serum uric acid and nitric oxide. JAMA 283:2240–2241
Zhang JX, Zhang YP, Wu QN, Chen B (2015) Uric acid induces oxidative stress via an activation of the renin-angiotensin system in 3T3-L1 adipocytes. Endocrine 48:135–142. https://doi.org/10.1007/s12020-014-0239-5
Corry DB, Tuck ML (2006) Uric acid and the vasculature. Curr Hypertens Rep 8:116–119
Nakagawa T, Hu H, Zharikov S, Tuttle KR, Short RA, Glushakova O, Ouyang X, Feig DI, Block ER, Herrera-Acosta J, Patel JM, Johnson RJ (2006) A causal role for uric acid in fructose-induced metabolic syndrome. Am J Physiol Renal Physiol 290:F625–F631. https://doi.org/10.1152/ajprenal.00140.2005
Perez-Pozo SE, Schold J, Nakagawa T, Sanchez-Lozada LG, Johnson RJ, Lillo JL (2010) Excessive fructose intake induces the features of metabolic syndrome in healthy adult men: role of uric acid in the hypertensive response. Int J Obes (London) 34:454–461. https://doi.org/10.1038/ijo.2009.259
Kawamoto R, Ohtsuka N, Ninomiya D, Nakamura S (2007) Carotid atherosclerosis in normal-weight metabolic syndrome. Intern Med 46:1771–1777
Acknowledgements
This work was supported in part by a grant-in-aid from the Foundation for Development of Community (2017). No additional external funding was received for this study. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee at which the studies were conducted (IRB Approval number: 1402009).
Informed consent
We obtained consent through the opt-out procedure from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kawamoto, R., Ninomiya, D., Kasai, Y. et al. Baseline and changes in serum uric acid independently predict 11-year incidence of metabolic syndrome among community-dwelling women. J Endocrinol Invest 41, 959–968 (2018). https://doi.org/10.1007/s40618-017-0822-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-017-0822-8