Abstract
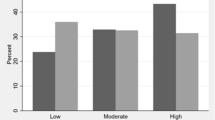
Diabetes and hypertension are socially patterned by individual race/ethnicity and by neighborhood economic context, but distributions among Asian subgroups are undercharacterized. We examined variation in prevalence for both conditions, comparing between US Asian subgroups, including within South Asian nationalities, and comparing within subgroups by neighborhood economic context. We obtained data on a non-probability sample of 633,664 patients ages 18–64 in New York City, NY, USA (2014–2017); 30,138 belonged to one of seven Asian subgroups (Asian Indian, Bangladeshi, Pakistani, Chinese, Korean, Japanese, and Filipino). We used electronic health records to classify disease status. We characterized census tract economic context using the Index of Concentration at the Extremes and estimated prevalence differences using multilevel models. Among Asian men, hypertension prevalence was highest for Filipinos. Among Asian women, hypertension prevalence was highest for Filipinas and Bangladeshis. Diabetes prevalence was highest among Pakistanis and Bangladeshis of both genders, exceeding all other Asian and non-Asian groups. There was consistent evidence of an economic gradient for both conditions, whereby persons residing in the most privileged neighborhood tertile had the lowest disease prevalence. The economic gradient was particularly strong for diabetes among Pakistanis, whose prevalence in the most deprived tertile exceeded that of the most privileged by 9 percentage points (95% CI 3, 14). Only Koreans departed from the trend, experiencing the highest diabetes prevalence in the most privileged tertile. US Asian subgroups largely demonstrate similar neighborhood economic gradients as other groups. Disaggregating Asian subgroups, including within South Asian nationalities, reveals important heterogeneity in prevalence.




Similar content being viewed by others
References
Watson T, Carlino G, Ellen IG. Metropolitan growth, inequality, and neighborhood segregation by income [with Comments]. Brookings-Wharton Papers on Urban Affairs. Published online 2006;1–52.
Krieger N, Waterman PD, Spasojevic J, Li W, Maduro G, Van Wye G. Public health monitoring of privilege and deprivation with the index of concentration at the extremes. Am J Public Health. 2015;106(2):256–63. https://doi.org/10.2105/AJPH.2015.302955.
Feldman JM, Waterman PD, Coull BA, Krieger N. Spatial social polarisation: using the index of concentration at the extremes jointly for income and race/ethnicity to analyse risk of hypertension. J Epidemiol Community Health. 2015;69(12):1199–207. https://doi.org/10.1136/jech-2015-205728.
Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55(2):111–22. https://doi.org/10.1136/jech.55.2.111.
Kandula NR, Wen M, Jacobs EA, Lauderdale DS. Association between neighborhood context and smoking prevalence among Asian Americans. Am J Public Health. 2009;99(5):885–92. https://doi.org/10.2105/AJPH.2007.131854.
Ladabaum U, Clarke CA, Press DJ, Mannalithara A, Myer PA, Cheng I, et al. Colorectal cancer incidence in Asian populations in California: effect of nativity and neighborhood-level factors. Am J Gastroenterol. 2014;109(4):579–88. https://doi.org/10.1038/ajg.2013.488.
Lim S, Yi SS, Lundy De La Cruz N, Trinh-Shevrin C. Defining ethnic enclave and its associations with self-reported health outcomes among Asian American adults in New York City. J Immigrant Minority Health. 2017;19(1):138–46. https://doi.org/10.1007/s10903-015-0334-6.
Islam NS, Khan S, Kwon S, Jang D, Ro M, Trinh-Shevrin C. Methodological issues in the collection, analysis, and reporting of granular data in Asian American populations: historical challenges and potential solutions. J Health Care Poor Underserved. 2010;21(4):1354–81. https://doi.org/10.1353/hpu.2010.0939.
Jiali Y, Rust G, Baltrus P, Daniels E. Cardiovascular risk factors among Asian Americans: results from a National Health Survey. Ann Epidemiol. 2009;19(10):718–23. https://doi.org/10.1016/j.annepidem.2009.03.022.
Fei K, Rodriguez-Lopez JS, Ramos M, Islam N, Trinh-Shevrin C, Yi SS, et al. Racial and ethnic subgroup disparities in hypertension prevalence, New York City Health and Nutrition Examination Survey, 2013-2014. Prev Chronic Dis. 2017;14:E33. https://doi.org/10.5888/pcd14.160478.
Health Disparities among Asian New Yorkers. New York City Department of Health and Mental Hygiene; 2018. https://www1.nyc.gov/assets/doh/downloads/pdf/epi/databrief100.pdf. Accessed 30 Sept 2019.
Sohani ZN, Deng WQ, Pare G, Meyre D, Gerstein HC, Anand SS. Does genetic heterogeneity account for the divergent risk of type 2 diabetes in South Asian and white European populations? Diabetologia. 2014;57(11):2270–81. https://doi.org/10.1007/s00125-014-3354-1.
Al Kibria GM. Racial/ethnic disparities in prevalence, treatment, and control of hypertension among US adults following application of the 2017 American College of Cardiology/American Heart Association guideline. Prev Med Rep. 2019;14. https://doi.org/10.1016/j.pmedr.2019.100850.
Williamson T, Green ME, Birtwhistle R, Khan S, Garies S, Wong ST, et al. Validating the 8 CPCSSN case definitions for chronic disease surveillance in a primary care database of electronic health records. Ann Fam Med. 2014;12(4):367–72. https://doi.org/10.1370/afm.1644.
Goldstein BA, Bhavsar NA, Phelan M, Pencina MJ. Controlling for informed presence bias due to the number of health encounters in an electronic health record. Am J Epidemiol. 2016;184(11):847–55. https://doi.org/10.1093/aje/kww112.
Massey DS. The prodigal paradigm returns: ecology comes back to sociology. Does it take a village. Published online 2001;41–48.
US Census Bureau. Table H-1. Income limits for each fifth and top 5 percent. Historical income tables: households. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-income-households.html. Accessed 28 Aug 2019.
Ruggles S, Flood S, Goeken R, et al. IPUMS USA: version 8.0 [dataset], vol. 10. Minneapolis: IPUMS; 2018. p. D010.
Staimez LR, Weber MB, Narayan KMV, Oza-Frank R. A systematic review of overweight, obesity, and type 2 diabetes among Asian American subgroups. Curr Diabetes Rev. 2013;9(4):312–31.
Lopez G, Ruiz N, Patten E. Key facts about Asian Americans. Pew Research Center: Fact Tank. Published September 8, 2017. https://www.pewresearch.org/fact-tank/2017/09/08/key-facts-about-asian-americans/. Accessed 29 Aug 2019.
Do DP, Finch BK. The link between neighborhood poverty and health: context or composition? Am J Epidemiol. 2008;168(6):611–9. https://doi.org/10.1093/aje/kwn182.
Funding
This study was supported by the NYU Center for the Study of Asian American Health Under the NIH National Institute on Minority Health & Health Disparities grant award #U54MD000538-15. It was additionally supported by grant award #U48DP005008 from the Centers for Disease Control and Prevention (CDC) and #R01DK110048 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Our study was deemed exempt from review by the NYU School of Medicine Institutional Review Board because the dataset did not contain individually identifiable patient records.
Disclaimer
The findings and conclusions in this article are solely the responsibility of the authors and may not represent the official view of the CDC, NIH, NIMHD, or NIH NIDDK.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Feldman, J.M., Conderino, S., Islam, N.S. et al. Subgroup Variation and Neighborhood Social Gradients—an Analysis of Hypertension and Diabetes Among Asian Patients (New York City, 2014–2017). J. Racial and Ethnic Health Disparities 8, 256–263 (2021). https://doi.org/10.1007/s40615-020-00779-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-020-00779-7