Abstract
Migrant workers are disproportionately affected by HIV due to poverty, social isolation, lack of access to and availability of health care services, acculturation, language barriers, constant mobility, and lack of knowledge. This study examined the impact of changes in social support on ethnic identity and HIV risk behaviors among migrant workers in South Florida. For this study, baseline and 6-month follow-up data were collected from an HIV intervention study among migrant workers in South Florida (n = 270) who reported unprotected sex in the past 30 days. The Multigroup Identity Measure was used to assess ethnic identity and the Social Provisions Scale examined the degree to which respondents’ social relationships provide various dimensions of social support. Social support was a significant predictor of ethnic identity and of ethnic identity subscales, ethnic identity belonging and ethnic identity explore. There were small but statistically significant short-term changes in ethnic identity and ethnic identity subscales among the migrant workers over the 6-month time period assessed after controlling for the intervention. Future studies should be conducted over a longer period of time to better assess this relationship and possible factors to reduce HIV risk behaviors. There is a need to focus on improving the quality of health and reduce HIV and other risks experienced by this marginalized community.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The South Florida region has been severely affected by the HIV epidemic, with elevated risks being detected in the migrant worker (MW) community [6, 28]. MWs are disproportionately affected by HIV due to poverty, social isolation, lack of access to and availability of health care services, and lack of knowledge [16, 24, 30]. HIV/AIDS prevalence rates among migrant workers are very difficult to assess due to the limited research conducted on this marginalized, hard-to-reach community. Also, the available studies assessing this topic are usually done in small, local populations. According to the National Center for Farmworker Health (NCFH) Factsheet [5] in the USA, the prevalence of HIV among migrant workers ranged from 2.6% to as high as 13%.
Social isolation, language barriers, and constant mobility are additional challenges MWs face. Underreporting of health conditions among migrant workers is common because of the limited access to health and availability of health care services and the fear of loss of wages. Underreporting of medical conditions contributes to the lack of data on illnesses throughout the MW community [8]. Coping mechanisms often used to deal with many of the hardships in their way of life are engaging in risky sexual activity and substance and alcohol abuse behaviors that may place MWs at heightened risk for HIV and many other chronic and infectious diseases [4, 6, 9, 31].
Acculturation and ethnic identity (EI) further impact HIV/AIDS risk, especially among MWs. Acculturation is the exchange of cultural practices and beliefs between two or more cultural groups. EI, a dimension of acculturation, involves group affiliation with, feelings of belongingness to, and a sense of shared values with one’s own ethnic group. EI also includes aspects of ethnic involvement, such as language, practices, and knowledge of ethnic group history. Moreover, EI describes an individual’s attachment to his or her ethnic origin and is considered to be a measureable component of or, at times, a proxy measure for acculturation [18, 22]. Prior research suggests that a decline in EI is common among individuals who emigrated to a new country or region at a young age or lived in a foreign place for an extensive amount of time. Complex effects on health outcomes in US migrant populations are influenced by changes in acculturation and EI, especially among Hispanics [10].
Studies have shown that higher levels of EI are associated with stronger social support networks and greater likelihood of utilizing social support services [11, 32]. EI, particularly the degree of closeness one feels with his or her ethnic group, may increase utilization of social support and other services when accessed via members of their own ethnic group network. Increased access to services from within one’s own ethnic community may contribute to more positive health outcomes [17, 23]. EI, along with the social support it provides, may serve as a protective factor for ethnic minorities and new immigrants. For example, a study by Cole et al. [2] with adolescent ethnic minorities found that ethnic identity and social support moderated the mental well-being and academic performance among ethnic minorities [2]. A study by Lopez and her colleagues [11] concluded that women living with HIV who had high EI displayed less perceived stress; this was suggested to be a result of better coping and more social support resources [11]. The focus of this study is to examine the impact that changes in social support have on EI and, ultimately, HIV risk behaviors among migrant workers in South Florida.
Methods
Sample
Data were collected from a larger study assessing the effectiveness of an enhanced/adapted cognitive behavioral intervention, Peer Education Ends Risky Behaviors (PEER), with a health promotion control program, Health Education Always Leads To a Healthy You (HEALTHY), for producing long-term reductions in HIV risk among alcohol and other drug-using migrant workers [15]. Both intervention and control groups were conducted in English and Spanish. Participants in the parent study were migrant workers residing in Immokalee, an agricultural area in Collier County, Florida. The participants included in this study were selected by targeted sampling and were recruited from “camps” which referred to trailer parks, dormitory-style housing, apartment buildings, motels, duplexes, and neighborhoods of single/duplex housing in the immediate and surrounding areas. In this setting, potential participants were approached and asked a few questions to see if they complied with the eligibility criteria. Inclusion criteria were the following: age 18 years or older; at least one episode of unprotected (without a condom) vaginal, anal, and/or oral sex; alcohol or other drug intake in the past 90 days; and fluent in English and/or Spanish. After the sample was recruited, participants were randomly assigned into one of the two groups, PEER or HEALTHY [15]. The present study was limited to participants who were present for both baseline and 6-month follow-up assessment (n = 270).
Low socioeconomic status, low formal education level, unstable employment, hazardous working conditions, and the stress of migration to a new environment are a few of the life circumstances that migrant workers endure. There are several reasons for the high loss of follow-up, but a major reason may be the fear that is common among many migrant workers of being reported to immigration services. The study defined potential participants as migrant workers (migratory agricultural workers and seasonal agricultural workers) who conformed to the Public Health Services Act definition (Public Health Service Act of 1944 § 330, 42 USCS § 254b). According to PHSA, “a migratory agricultural worker is an individual whose principal employment is in agriculture, who has been so employed within the last 24 months, and who establishes for the purposes of such employment a temporary abode and seasonal agricultural worker is an individual whose principal employment is in agriculture on a seasonal basis and who is not a migratory agricultural worker.”
Measures
All the variables used in this study were self-reported and collected through the HIV/AIDS Risk Reduction Questionnaire (HRRQ), composed of 204 questions and covered 13 sections, utilized in the parent study. The 13 sections are Demographics, Mulitgroup Ethnic Identity Measure (MEIM), Social Provisions Scale (SPS), General Health, Sex Behavior, Stages of Change, Self Efficacy, Condom Social Norms, Sex Relates Alcohol Expectancies (SRAE), Short Inventory of Problems, Alcohol and Drug Use, and Abuse History.
Multigroup Ethnic Identity Measure
The Multigroup Ethnic Identity Measure (MEIM) was used to assess participants’ ethnic identity level [20, 25]. The MEIM is a 12-item questionnaire divided into two components: ethnic identity explore and ethnic identity belonging. Ethnic identity explore (five items) measured the extent to which individuals explore or take an active role to become better acquainted with and learn about their ethnic group. Ethnic identity belonging (seven items) included ethnic pride, positive feelings toward one’s ethnic group, and satisfaction with being a member of one’s ethnic group. Responses for each item ranged from 1 (strongly disagree) to 4 (strongly agree). Scores for each scale were calculated as well as a mean score for the measure as a whole; the higher the mean MEIM score, the higher the participant’s ethnic identity.
HIV Risk Behavior
HIV risk behavior was measured by number of sexual partners without a condom. The number of unprotected sexual partners variable specifies the number of partners with whom the participant engaged in sex without a condom in the last 30 days.
Social Provisions Scale
The Social Provisions Scale (SPS) examined the degree to which respondents’ social relationships provide various dimensions of social support [3]. SPS will be referred to as social support throughout this manuscript. This 24-item scale was a multi-dimensional construct which yields a total score. The responses utilize a Likert scale ranging from 1 (strongly agree) to 5 (strongly disagree). The Cronbach’s alpha for SPS was 0.80.
Change Scores
Change scores were created for social support, ethnic identity total, ethnic identity belonging, and ethnic identity explore. Change scores were created by subtracting baseline values from 6-month follow-up values.
Statistical Analysis
IBM SPSS Statistics (version 23) was used for data analysis (Armonk, NY: IBM Corp). Descriptive statistics were calculated to describe the characteristics of the sample. Chi-square analysis and independent samples t tests were used to compare demographic characteristics, ethnic identity, social support, sexual risk behaviors of participants at baseline, and those lost to follow-up. Multiple linear regressions were performed to assess the nature of the relationship between ethnic identity total change, ethnic identity belonging change, and ethnic identity explore change with changes in social support between baseline and 6-month follow-up. Change was calculated by computing the difference between EI scores at baseline and 6-month follow-up data. Three models were tested predicting ethnic identity total change, ethnic identity belonging change and ethnic identity explore change. For each model, the independent variables in block 1 were gender, education, country of birth, length of stay, marital status, and intervention group (included to control for intervention effects). In block 2, social support change was added. Multiple linear regressions were also conducted to assess predictors of number of unprotected sex partners. Regression was done in two blocks. In block 1, predictors included gender, education, country of birth, age, length of stay, marital status, and intervention group. In block 2, changes in ethnic identity (including ethnic identity total, ethnic identity explore and ethnic identity belonging) and social support change were added.
Results
Demographics
Data used for this study was drawn from a larger sample (n = 431) of participants in the parent study. Participants included in the analyses below include 270 migrant workers who were assessed at both baseline and 6-month follow-up. Those who were lost to follow-up were not able to be located for follow-up assessment. The sample (n = 270) was composed of 67% (n = 180) males and 33% (n = 90) females; the average level of educational achievement was ninth grade (M = 9.19, SD = 3.10); the mean age of the sample was 42.5 years (SD = 12.76); and 69% (n = 185) were single. The sample was composed of both Hispanic (n = 142, 52%) and African-American (n = 128, 48%) ethnicities. Table 1 shows the sociodemographic characteristics of the participants.
When comparing cases not included in the analyses (n = 161) and those followed (n = 270), there were a number of significant differences. The cases lost to follow-up were significantly younger (M = 39.86 years, SD = 11.48) than the cases that participated (M = 42.58 years, SD = 12.82) in the 6-month assessment period (t = −2.172, p < .05), and those lost to follow-up had a significantly lower level of education (M = 7.37 years, SD = 3.57) compared to participants (M = 9.19 years, SD = 3.10) included in this study (t = −5.207, p < .001). A large portion (80%) of the lost cases were of Hispanic ethnicity (80%, χ 2 = 31.99, p < .001), and lost cases consumed significantly larger amounts of crack in the last 30 days compared to the followed cases (M = 27.55, SD = 85.91 vs. M = 4.01, SD = 23.55), respectively; t = 4.209, p < .001). Means and standard deviations for those followed vs. those lost to follow-up are presented in Table 2.
Social Support Levels
Baseline social support levels ranged from 50 to 119, with an average score of 85.48 (SD = 11.18). This measure represents the feeling that people can be counted on when the individual is under stress (high and low stress situations). At 6-month follow-up, social support levels ranged from 24 to 119, with an average score of 90.66 (SD = 13.70). On average, social support scores increased between baseline to 6-month follow-up by 4.97 points (SD = 13.84). The Cronbach’s alpha for SPS was 0.80.
Ethnic Identity Levels
Baseline and 6-month total ethnic identity scores ranged from 1 to 4 with average scores of 2.86 (SD = .38) and 2.97 (SD = .40), respectively. The MEIM (EI scores) focuses on areas of acculturation, ethnic identification, and commitment or level of belonging to one’s ethnic group. The score gives an indication of the comfort level participants have with the individuals, beliefs, and practices from their ethnic group. The higher the score, the more comfortable the participant feels with their ethnic group. Baseline and 6-month ethnic identity belonging scores ranged from 1 to 4 with average scores of 3.05 (SD = .42) and 3.19 (SD = .50), respectively. Ethnic identity belonging examines the extent to which individuals feel a positive sense of belonging with their ethnic group. This subscale is composed of seven items from the MEIM measure. On average, ethnic identity belonging scores increased by .20 points (SD = .68).
Baseline and 6-month ethnic identity explore scores ranged from 1 to 4 with average scores of 2.61 (SD = .43) and 2.68 (SD = .46), respectively. The ethnic identity explore component measures the degree to which individuals explore or take an active role to become better acquainted with and learn about their ethnic group. Ethnic identity explore was created by taking the mean of five items from the MEIM scale.
On average, ethnic identity explore scores increased by .07 points (SD = .60). Cronbach’s alpha for the overall instrument was 0.85, for ethnic identity belonging α = 0.85, and for ethnic identity belonging α = 0.51.
HIV Risk Behavior
At baseline, participants reported an average of 2.14 (SD = 4.32) sex partners, an average of .75 (SD = 1.70) unprotected sex partners and an average of 3.36 (SD = 6.97) unprotected vaginal sex acts. At baseline, 23.0% of subjects reported not having any sex partners during the last 30 days. At 6-month follow-up, participants reported an average of 1.46 (SD = 6.387) sex partners, an average of .29 (SD = .83) unprotected sex partners and an average of 1.94 (SD = 5.32) unprotected vaginal sex acts. At 6-month follow-up, 50.0% of subjects reported not having any sex partners. Of those that did report sex at 6-month follow-up (n = 135), only 43% (n = 58) of subjects engaged in unprotected sex.
Association between Change in Social Support and Changes in Ethnic Identity
Multiple regression was used to assess the relationships between change in social support and ethnic identity changes (including ethnic identity total, ethnic identity explore, and ethnic identity belonging). Block 1 predictors included gender, education, country of birth, length of stay, marital status, and intervention group (included to control for intervention effects). In block 2, social support change was added. The variables in the first block did not contribute significantly to predicting change in ethnic identity total, R 2 = .04, F(7, 268) = 1.42, p = .199. The inclusion of social support change in the second block resulted in a significant model, R 2 = .22, F(8, 268) = 9.02, p < .001. The standardized regression coefficients show that social support change was the only significant predictor of change in ethnic identity total. Those with greater increases in social support had greater increases in ethnic identity total. A similar trend was seen with the regression model predicting change in ethnic identity belonging. The variables in the first block did not contribute significantly to predicting change in ethnic identity belonging, R 2 = .04, F(7, 268) = 1.62, p = .130. The inclusion of social support change in the second block resulted in a significant model, R 2 = .17, F(8, 268) = 6.40, p < .001. The standardized regression coefficients show that social support change was the only significant predictor of change in ethnic identity belonging. Those with greater increases in social support had greater increases in ethnic identity belonging. With regard to change in ethnic identity explore, the variables in the first block did not contribute significantly to predicting change in ethnic identity explore, R 2 = .05, F(7, 268) = 1.85, p = .079. The inclusion of social support change in the second block resulted in a significant model, R 2 = .11, F(8, 268) = 4.14, p < .001. The standardized regression coefficients show that marital status and social support change were the only significant predictors of change in ethnic identity explore. Those with greater increases in social support had greater increases in ethnic identity explore and those who were single were more likely to have increases in ethnic identity explore between baseline and 6-month follow-up. The variance (R 2), standardized regression (β), the standard error (SE), and the unstandardized regression coefficients (B) for all three regression models are shown in Table 2.
Association between Ethnic Identity, Social Support, and HIV Risk Behavior
Correlations and regression were used to assess the relationship between changes in ethnic identity (including ethnic identity total, ethnic identity explore, and ethnic identity belonging); changes in social support; and HIV risk behavior (unprotected sex partners at 6-month follow-up) among those who reported having sex at 6-month follow-up (n = 135). Correlations are shown in Table 3. Change scores for ethnic identity total, ethnic identity explore, and ethnic identity belonging were significantly correlated with number of unprotected sex partners (r = .316, p < .001; r = .233, p = .007; r = .285, p = .001, respectively). In addition, change in social support was significantly correlated with number of unprotected sex partners at 6-month follow-up (r = .198, p = .021). Greater increases in ethnic identity total, ethnic identity explore, ethnic identity belonging, and social support were associated with a greater number of unprotected sex partners at 6-month follow-up.
Multiple regression was used to identify predictors of number of unprotected partners at 6-month follow-up (Table 4). Block 1 predictors included gender, education, country of birth, age, length of stay, marital status, and intervention group (included to control for intervention effects). In block 2, changes in ethnic identity (including ethnic identity total, ethnic identity explore, and ethnic identity belonging) and social support change were added. The variables in the first block did not contribute significantly to predicting number of unprotected sex partners at 6-month follow-up, R 2 = .05, F(7, 126) = .89, p = .516. The inclusion of ethnic identity change variables and social support change in the second block resulted in a model that approached significance, R 2 = .14, F(10, 126) = 1.86, p ≤ .058. The standardized regression coefficients show that change in ethnic identity belonging was the only significant predictor of number of unprotected sex partners at 6-month follow-up. Those with greater increases in social support had greater increases in HIV risk.
Discussion
This study makes a number of contributions to the present literature on migrant workers and the impact of social support on their engagement in HIV risk behaviors. Change in social support was a significant predictor of change in ethnic identity and of change in ethnic identity subscales, ethnic identity belonging, and ethnic identity explore. This association has been supported in previous research; however, in the reverse direction, suggesting that social support and ethnic identity may have a reciprocal relationship. Utilization of social support is a manner of coping with the new environment for immigrants. Particularly among minority groups, strong social support has been associated with higher levels of ethnic identity. In many cases, strong levels of group identification may improve group support or allow such support to be accessible [2, 23]. Previous literature found that social support was a mediator of ethnic identity and adjustment to college for Latino college students [27]. High levels of ethnic identity have also been associated with stronger social support as well as a higher likelihood of accessing social support services [11]. Evaluations of the effects of social support generally assessed a single point in time rather than changes over time. In this study, changes in social support were found to be associated with changes in ethnic identity for the migrant workers in this sample.
Social support is known to have a strong influence upon health outcomes and psychological well-being. Studies have consistently found social support to aid in preventing negative health outcomes in times of duress, often referred to as the Social Support Buffering Hypothesis [1, 7, 12]. However, social support may play different roles in different cultures. For example, a study analyzing HIV-positive Latinas’ positive and negative coping styles concluded that those individuals who utilized positive coping styles, such as obtaining social support, were found to consume fewer cigarettes and less alcohol, and showed greater adherence to their HIV medication [26].
Social support has also been found to be a protective factor against risky sexual behaviors. Research has shown that low social support places young females at higher likelihood of engaging in sexual behaviors which put them at risk for STIs, especially HIV [14]. The association between social support and risk behaviors may be direct or indirect. For example, one study found social support to be directly associated with substance abuse and indirectly with risky sexual behaviors [19]. The same indirect relationship may be present in this study since there was a direct link between social support and ethnic identity and ethnic identity has been demonstrated to be associated with HIV risk behaviors [29].
In terms of ethnic identity subscales, the changing environment in which one lives may be another contributor to ethnic identity explore. In the present study, the primary predictor of ethnic identity explore change was marital status, suggesting that social support is built into marital status, requiring that singles seek support from their community. A recent study by Phinney [21] explains that ethnic identity exploration in emerging adults is affected by the stability of their surrounding environment [21]. Phinney posits that if one resides in a constantly changing environment, this may influence one’s level of ethnic identity explore [21]. This phenomenon seems to be applicable to the migrant worker sample examined in this study; they live with unstable housing and employment, and their ethnic identity was found in this study to change over time.
It is important to consider certain study limitations when interpreting outcomes from this study. First, the data reported were self-reported, therefore potentially increasing bias and may not be as accurate as other forms of reporting. It is also important to note that there was a minimal difference found between ethnic identity from baseline and 6-month follow-up period, possibly a result of error. Finally, although longitudinal research on ethnic identity and support among Hispanic migrant workers is valuable and unprecedented, the time period over which the data were analyzed was relatively short. It is possible that a longer follow-up period would have led to additional findings.
Conclusion
Future studies on the link between ethnic identity and social support among migrant workers may be helpful in reducing HIV risk. Research should be conducted over a longer period of time to better assess this relationship and possible factors to reduce HIV risk behaviors. Culturally sensitive HIV/STI prevention interventions have been beneficial among ethnic/minority groups, and future intervention research may be enhanced if culturally sensitive indicators such as ethnic identity are included. It has also been found that including concepts that are familiar to one’s ethnic background can be beneficial. Ethnically familiar context was included and implemented in the HIV risk reduction intervention used in the parent study. The low wages, difficult employment situations, and other stressors in the environment of migrant workers make them highly vulnerable to engaging in unhealthy and risky behaviors as coping mechanisms [13]. Future research should be geared toward improving the quality of health and reduction of HIV and other risks experienced by this marginalized community.
References
Clay OJ, Roth DL, Wadley VG, Haley WE. Changes in social support and their impact on psychosocial outcome over a 5-year period for African American and white dementia caregivers. International journal of geriatric psychiatry. 2008;23(8):857–62.
Cole B, Matheson K, Anisman H. The moderating role of ethnic identity and social support on relations between well-being and academic performance. J Appl Soc Psychol. 2007;37(3):592–615.
Cutrona C, Russell D, Rose J. Social support and adaptation to stress by the elderly. Psychol Aging. 1986;1(1):47.
Duke MR, Gómez Carpinteiro FJ. The effects of problem drinking and sexual risk among Mexican migrant workers on their community of origin. Hum Organ. 2009;68(3):328–39.
Farmworkers’ Health Fact Sheet – Data from the National Agricultural Workers Survey (2015). Farmworker Justice & The National Center for Farmworker Health. Retrieved from http://www.ncfh.org/uploads/3/8/6/8/38685499/fs-nawshealthfactsheet.pdf. Accessed 15 Sept 2016.
Fernández MI, Collazo JB, Hernández N, Bowen GS, Varga LM, Vila CK, …, Perrino T. Predictors of HIV risk among Hispanic farm workers in South Florida: women are at higher risk than men. AIDS Behav. 2004;8(2):165–74.
Gaylord-Harden NK, Ragsdale BL, Mandara J, Richards MH, Petersen AC. Perceived support and internalizing symptoms in African American adolescents: self-esteem and ethnic identity as mediators. Journal of Youth and Adolescence. 2007;36(1):77–88.
Hansen E, Donohoe M. Health issues of migrant and seasonal farm workers. J Health Care Poor Underserved. 2003;14(2):153–64.
Hirsch JS, Higgins J, Bentley ME, Nathanson CA. The social constructions of sexuality: marital infidelity and sexually transmitted disease-HIV risk in a Mexican migrant community. Am J Public Health. 2002;92(8):1227–37.
Iturbide MI, Raffaelli M, Carlo G. Protective effects of ethnic identity on Mexican American college students’ psychological well-being. Hisp J Behav Sci. 2009;31(4):536–52.
Lopez CR, Antoni MH, Fekete EM, Penedo FJ. Ethnic identity and perceived stress in HIV+ minority women: the role of coping self-efficacy and social support. International journal of behavioral medicine. 2012;19(1):23–8.
Lyyra T-M, Heikkinen R-L. Perceived social support and mortality in older people. J Gerontol Ser B Psychol Sci Soc Sci. 2006;61(3):S147–52.
MacNaughton NS. Health disparities and health-seeking behavior among Latino men a review of the literature. J Transcult Nurs. 2008;19(1):83–91.
Mazzaferro KE, Murray PJ, Ness RB, Bass DC, Tyus N, Cook RL. Depression, stress, and social support as predictors of high-risk sexual behaviors and STIs in young women. J Adolesc Health. 2006;39(4):601–3.
McCoy HV, Hlaing WM, Ergon-Rowe E, Samuels D, Malow R. Lessons from the fields: a migrant HIV prevention project. Public Health Rep. 2009;124(6):790.
Munoz-Laboy M, Hirsch JS, Quispe-Lazaro A. Loneliness as a sexual risk factor for male Mexican migrant workers. Am J Public Health. 2009;99(5):802.
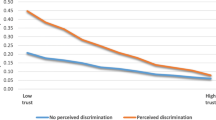
Noh S, Kaspar V. Perceived discrimination and depression: moderating effects of coping, acculturation, and ethnic support. Am J Public Health. 2003;93(2):232–8.
Persky I, Birman D. Ethnic identity in acculturation research a study of multiple identities of Jewish refugees from the former soviet union. J Cross-Cult Psychol. 2005;36(5):557–72.
Peterson CH, Buser TJ, Westburg NG. Effects of familial attachment, social support, involvement, and self-esteem on youth substance use and sexual risk taking. Fam J. 2010;18(4):369–76.
Phinney JS. The multigroup ethnic identity measure a new scale for use with diverse groups. J Adolesc Res. 1992;7(2):156–76.
Phinney JS. Bridging identities and disciplines: advances and challenges in understanding multiple identities. New directions for child and adolescent development. 2008;2008(120):97–109.
Phinney JS, DuPont S, Espinosa C, Revill J, Sanders K. Ethnic identity and American identification among ethnic minority youths. 1994.
Phinney JS, Horenczyk G, Liebkind K, Vedder P. Ethnic identity, immigration, and well-being: an interactional perspective. J Soc Issues. 2001;57(3):493–510.
Rhodes SD, Bischoff WE, Burnell JM, Whalley LE, Walkup MP, Vallejos QM, …, Arcury TA. HIV and sexually transmitted disease risk among male Hispanic/Latino migrant farm workers in the Southeast: findings from a pilot CBPR study. Am J Ind Med. 2010;53(10):976–83.
Roberts RE, Phinney JS, Masse LC, Chen YR, Roberts CR, Romero A. The structure of ethnic identity of young adolescents from diverse ethnocultural groups. The Journal of Early Adolescence. 1999;19(3):301–22.
Sánchez M, Rice E, Stein J, Milburn NG, Rotheram-Borus MJ. Acculturation, coping styles, and health risk behaviors among HIV positive Latinas. AIDS Behav. 2010;14(2):401–9.
Schneider ME, Ward DJ. The role of ethnic identification and perceived social support in Latinos' adjustment to college. Hisp J Behav Sci. 2003;25(4):539–54.
Shehadeh N, McCoy H. Risky sexual behaviors: the role of ethnic identity in HIV risk in migrant workers. J Assoc Nurses AIDS Care. 2013;25(4):330–40.
Shehadeh N, McCoy HV, Rubens M, Batra A, Renfrew R, Winter K. The impact of ethnic identity on changes in high risk HIV behaviors in sexually active migrant workers. J Immigr Minor Health. 2012;14(1):100–6.
Villarejo D. The health of US hired farm workers. Annu Rev Public Health. 2003;24(1):175–93.
Weatherby NL, McCoy HV, Bletzer KV, McCoy CB, Inciardi JA, McBride DC, Forney MA. Immigration and HIV among migrant workers in rural southern Florida. J Drug Issues. 1997;27(1):155–72.
Yoo HC, Lee RM. Ethnic identity and approach-type coping as moderators of the racial discrimination/well-being relation in Asian Americans. J Couns Psychol. 2005;52(4):497.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors report no real or perceived vested interests that relate to this article that could be construed as a conflict of interest.
Rights and permissions
About this article
Cite this article
Shehadeh, N., Rubens, M., Attonito, J. et al. Social Support and Its Impact on Ethnic Identity and HIV Risk among Migrant Workers. J. Racial and Ethnic Health Disparities 5, 96–103 (2018). https://doi.org/10.1007/s40615-017-0347-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-017-0347-z