Abstract
Purpose of Review
It is reported that the prevalence of asthma is as high as 25% in patients with CRS, resulting in prolonged inflammation and recurrence. The remission of asthma has been found to be highly significant in contribution to the remission of CRS; hence, the usage of biologics treatment for asthma can be expanded towards the treatment for CRS with asthma. In this review, we summarized the usage of biologics in CRS with asthma treatment, their mechanisms, and future biologics in the development pipeline that would aid treatment for CRS with asthma.
Recent Findings
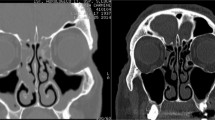
Chronic rhinosinusitis is an inflammatory disease of the upper airway, and many are often accompanied by an asthma comorbidity of the lower airway. Chronic rhinosinusitis with comorbid asthma is commonly known as the manifestation of refractory rhinosinusitis, which is a major challenge of its treatment for otolaryngologists. In recent years, the treatment strategy of chronic rhinosinusitis with asthma has garnered increasing research interest. Particularly, the targeting of TH2 inflammatory cytokines, such as IgE, IL5, IL4, and IL13, has spawned an antibody-based biologics treatment against the disease. The availability of the biologics and their clinical efficacy has lent confidence to the overall management of CRS with asthma in order to reduce the socioeconomic burden of the diseases.
Summary
This paper reviews the current biologics available for chronic rhinosinusitis with asthma, focusing on its mechanism and clinical efficacy, as well as highlighting promising biologics currently in trials that may aid in the treatment of the disease.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Fokkens WJ, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology. 2020;58(Suppl S29):1–464. https://doi.org/10.4193/rhin20.600 This paper summarizes the latest European guidelines on rhinosinusitis and nasal polyps.
Hastan D, et al. Chronic rhinosinusitis in Europe--an underestimated disease. A GA(2)LEN study. Allergy. 2011;66(9):1216–23. https://doi.org/10.1111/j.1398-9995.2011.02646.x.
Hirsch AG, et al. Nasal and sinus symptoms and chronic rhinosinusitis in a population-based sample. Allergy. 2017;72(2):274–81. https://doi.org/10.1111/all.13042.
Pilan RR, et al. Prevalence of chronic rhinosinusitis in Sao Paulo. Rhinology. 2012;50(2):129–38. https://doi.org/10.4193/rhino11.256.
Shi JB, et al. Epidemiology of chronic rhinosinusitis: results from a cross-sectional survey in seven Chinese cities. Allergy. 2015;70(5):533–9. https://doi.org/10.1111/all.12577.
Gliklich RE, Metson R. The health impact of chronic sinusitis in patients seeking otolaryngologic care. Otolaryngol Head Neck Surg. 1995;113(1):104–9. https://doi.org/10.1016/s0194-5998(95)70152-4.
Rivero A, Liang J. Anti-IgE and Anti-IL5 biologic therapy in the treatment of nasal polyposis: a systematic review and meta-analysis. Ann Otol Rhinol Laryngol. 2017;126(11):739–47. https://doi.org/10.1177/0003489417731782.
Rosenfeld RM, et al. Clinical practice guideline (update): adult sinusitis executive summary. Otolaryngol Head Neck Surg. 2015;152(4):598–609. https://doi.org/10.1177/0194599815574247.
Rudmik L, Soler ZM. Medical therapies for adult chronic sinusitis: a systematic review. Jama. 2015;314(9):926–39. https://doi.org/10.1001/jama.2015.7544.
Ha YK, et al. Burden of respiratory disease in Korea: an observational study on allergic rhinitis, asthma, COPD, and rhinosinusitis. J Allergy Asthma Immunol Res. 2016;8(6):527–34. https://doi.org/10.4168/aair.2016.8.6.527.
Hellings PW, Prokopakis EP. Global airway disease beyond allergy. J Curr Allergy Asthma Rep. 2010;10(2):143–9. https://doi.org/10.1007/s11882-010-0107-1.
Jarvis D, et al. Asthma in adults and its association with chronic rhinosinusitis: the GA2LEN survey in Europe. J Allergy Ther. 2012;67(1):91–8. https://doi.org/10.1111/j.1398-9995.2011.02709.x.
• Wu D, et al. Clinical phenotypes of nasal polyps and comorbid asthma based on cluster analysis of disease history. J Allergy Clin Immunol Pract. 2018;6(4):1297–1305 e1. https://doi.org/10.1016/j.jaip.2017.09.020. This paper pointed out the overlaps in morbidity of CRSwNP and Asthma.
Zhang Y, et al. Chronic rhinosinusitis in Asia. J J Allergy Clin Immunol. 2017;140(5):1230–9. https://doi.org/10.1016/j.jaci.2017.09.009.
Bachert C, Gevaert P, Hellings P. Biotherapeutics in chronic rhinosinusitis with and without nasal polyps. J Allergy Clin Immunol Pract. 2017;5(6):1512–6. https://doi.org/10.1016/j.jaip.2017.04.024.
•• Bidder T, et al. Omalizumab treats chronic rhinosinusitis with nasal polyps and asthma together-a real life study. Rhinology. 2018;56(1):42–5. https://doi.org/10.4193/rhin17.139 This is a good paper focus on the treatment for omalizumab on CRSwNP with asthma.
• Gevaert P, et al. Omalizumab is effective in allergic and nonallergic patients with nasal polyps and asthma. J Allergy Clin Immunol. 2013;131(1):110–6.e1. https://doi.org/10.1016/j.jaci.2012.07.047 This paper provides important clinical evidence for the therapeutic effect evalation of Omalizumab.
Ballantyne S, et al. Blocking IL-25 prevents airway hyperresponsiveness in allergic asthma. J Allergy Clin Immunol. 2007;120(6):1324–31. https://doi.org/10.1016/j.jaci.2007.07.051.
Bachert C, et al. Dupilumab improves patient-reported outcomes in patients with chronic rhinosinusitis with nasal polyps and comorbid asthma. J Allergy Clin Immunol Pract. 2019;7(7):2447–2449.e2. https://doi.org/10.1016/j.jaip.2019.03.023.
Xu M, Dong CJIR. IL-25 in allergic inflammation. Immunol Rev. 2017;278(1):185–91. https://doi.org/10.1111/imr.12558.
•• Chen ZG, et al. Neutralization of TSLP inhibits airway remodeling in a murine model of allergic asthma induced by chronic exposure to house dust mite. PLoS One. 2013;8(1):e51268. https://doi.org/10.1371/journal.pone.0051268 This paper give idea on the role of TSLP in the context of chronic allergic asthma.
Bachert C, et al. Reduced need for surgery in severe nasal polyposis with mepolizumab: randomized trial. J Allergy Clin Immunol. 2017;140(4):1024–1031.e14. https://doi.org/10.1016/j.jaci.2017.05.044.
Seshasayee D, et al. In vivo blockade of OX40 ligand inhibits thymic stromal lymphopoietin driven atopic inflammation. J Clin Invest. 2007;117(12):3868–78. https://doi.org/10.1172/jci33559.
Castro M, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet Respir Med. 2015;3(5):355–66. https://doi.org/10.1016/s2213-2600(15)00042-9.
Bleecker ER, et al. Efficacy and safety of benralizumab for patients with severe asthma uncontrolled with high-dosage inhaled corticosteroids and long-acting β(2)-agonists (SIROCCO): a randomised, multicentre, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2115–27. https://doi.org/10.1016/s0140-6736(16)31324-1.
Holgate ST, et al. The anti-inflammatory effects of omalizumab confirm the central role of IgE in allergic inflammation. J Allergy Clin Immunol. 2005;115(3):459–65. https://doi.org/10.1016/j.jaci.2004.11.053.
• Gilfillan AM, Tkaczyk CJNRI. Integrated signalling pathways for mast-cell activation. Nat Rev Immunol. 2006;6(3):218–30. https://doi.org/10.1038/nri1782.
•• Gandhi NA, et al. Targeting key proximal drivers of type 2 inflammation in disease. J Nat Rev Drug Discov. 2016;15(1):35–50. https://doi.org/10.1038/nrd4624 This paper state the importance of key proximal type 2 cytokines therapy in allergic diseases.
• Schulman ES. Development of a monoclonal anti-immunoglobulin e antibody (Omalizumab) for the treatment of allergic respiratory disorders. Am J Respir Crit Care Med. 2001;164(8):S6–11. https://doi.org/10.1164/ajrccm.164.supplement_1.2103025.
Hanf G, et al. Omalizumab inhibits allergen challenge-induced nasal response. Eur Respir J. 2004;23(3):414–9. https://doi.org/10.1183/09031936.04.00024504.
MacGlashan DW Jr, et al. Down-regulation of Fc(epsilon)RI expression on human basophils during in vivo treatment of atopic patients with anti-IgE antibody. J Immunol. 1997;158(3):1438–45 https://pubmed.ncbi.nlm.nih.gov/9013989/.
Presta LG, et al. Humanization of an antibody directed against IgE. J Immunol. 1993;151(5):2623–32 https://pubmed.ncbi.nlm.nih.gov/8360482/.
Rebecca N, et al., Omalizumab for asthma in adults and children. J Cochrane Database Syst Rev. 2014(1). https://doi.org/10.1002/14651858.cd003559.
Bagnasco D, et al. A critical evaluation of anti-IL-13 and anti-IL-4 strategies in severe asthma. Int Arch Allergy Immunol. 2016;170(2):122–31. https://doi.org/10.1159/000447692.
Wechsler ME. Inhibiting interleukin-4 and interleukin-13 in difficult-to-control asthma. N Engl J Med. 2013;368(26):2511–3. https://doi.org/10.1056/nejme1305426.
Keisuke O, et al. IL-33 and airway inflammation. J Allergy Asthma Immunol Res. 2011;3(2):81–8. https://doi.org/10.4168/aair.2011.3.2.81.
Rankin SM, Conroy DM, Williams TJ. Eotaxin and eosinophil recruitment: implications for human disease. Mol Med Today. 2000;6(1):20–7.
Howard M, Farrar J, Hilfiker M, Johnson B, Takatsu K, Hamaoka T, et al. Identification of a T cell-derived b cell growth factor distinct from interleukin 2. J J Exp Med. 1982;155(3):914–23. https://doi.org/10.1084/jem.155.3.914.
Gascan H, et al. Anti-CD40 monoclonal antibodies or CD4+ T cell clones and IL-4 induce IgG4 and IgE switching in purified human B cells via different signaling pathways. J Immunol. 1991;147(1):8–13 https://pubmed.ncbi.nlm.nih.gov/1711085/.
Wenzel S, et al. Dupilumab in persistent asthma with elevated eosinophil levels. N Engl J Med. 2013;368(26):2455–66. https://doi.org/10.1056/nejmoa1304048.
Bachert C, et al. Effect of Subcutaneous dupilumab on nasal polyp burden in patients with chronic sinusitis and nasal polyposis: a randomized clinical trial. Jama. 2016;315(5):469–79. https://doi.org/10.1001/jama.2015.19330.
•• Bachert C, et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet. 2019;394(10209):1638–50. https://doi.org/10.1016/s0140-6736(19)31881-1 This is an excellent randomized clinical trial for dupilumab on patient with CRSwNP.
Broughton SE, et al. The GM-CSF/IL-3/IL-5 cytokine receptor family: from ligand recognition to initiation of signaling. Immunol Rev. 2012;250(1):277–302. https://doi.org/10.1111/j.1600-065x.2012.01164.x.
Lopez AF, et al. Recombinant human interleukin 5 is a selective activator of human eosinophil function. J Exp Med. 1988;167(1):219–24. https://doi.org/10.1084/jem.167.1.219.
•• Denburg JA, et al. Regulation of IL-5 receptor on eosinophil progenitors in allergic inflammation: Role of Retinoic Acid. Int Arch Allergy Immunol. 2001;124(1-3):246–8. https://doi.org/10.1159/000053724 This is a paper demonstrating how the IL-5 works.
E BS, et al. The βc receptor family - structural insights and their functional implications. J Cytokine. 2015;74(2):247–58. https://doi.org/10.1016/j.cyto.2015.02.005.
Ortega HG, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med. 2014;371(13):1198–207. https://doi.org/10.1056/nejmoa1403290.
Agarwal A, et al. Therapeutic antibodies for nasal polyposis treatment: where are we headed? Clin Rev Allergy Immunol. 2019. https://doi.org/10.1007/s12016-019-08734-z.
Corren J, et al. Phase 3 study of reslizumab in patients with poorly controlled asthma Effects across a broad range of eosinophil counts. Chest. 2016;150(4):799–810. https://doi.org/10.1016/j.chest.2016.03.018.
Gevaert P, et al. Nasal IL-5 levels determine the response to anti-IL-5 treatment in patients with nasal polyps. J Allergy Clin Immunol. 2006;118(5):1133–41. https://doi.org/10.1016/j.jaci.2006.05.031.
Busse WW, et al. Long-term safety and efficacy of benralizumab in patients with severe, uncontrolled asthma: 1-year results from the BORA phase 3 extension trial. Lancet Respir Med. 2019;7(1):46–59. https://doi.org/10.1016/s2213-2600(18)30406-5.
•• FitzGerald JM, et al. Predictors of enhanced response with benralizumab for patients with severe asthma: pooled analysis of the SIROCCO and CALIMA studies. Lancet Respir Med. 2018;6(1):51–64. https://doi.org/10.1016/s2213-2600(17)30344-2 This paper is an polled analysis of two phase 3 trials on benralizumab.
FitzGerald JM, et al. Benralizumab, an anti-interleukin-5 receptor α monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2128–41. https://doi.org/10.1016/s0140-6736(16)31322-8.
Patel GB, et al. Current and future treatments of rhinitis and sinusitis. J Allergy Clin Immunol Pract. 2020;8(5):1522–31. https://doi.org/10.1016/j.jaip.2020.01.031.
Arm JP, et al. Pharmacokinetics, pharmacodynamics and safety of QGE031 (ligelizumab), a novel high-affinity anti-IgE antibody, in atopic subjects. Clin Exp Allergy. 2014;44(11):1371–85. https://doi.org/10.1111/cea.12400.
Gauvreau GM, et al. Efficacy and safety of multiple doses of QGE031 (ligelizumab) versus omalizumab and placebo in inhibiting allergen-induced early asthmatic responses. J Allergy Clin Immunol. 2016;138(4):1051–9. https://doi.org/10.1016/j.jaci.2016.02.027.
Nakagome K, et al. High expression of IL-22 suppresses antigen-induced immune responses and eosinophilic airway inflammation via an IL-10–associated mechanism. J Immunol. 2011;187(10):5077–89. https://doi.org/10.4049/jimmunol.1001560.
Takahashi K, et al. IL-22 attenuates IL-25 production by lung epithelial cells and inhibits antigen-induced eosinophilic airway inflammation. J Allergy Clin Immunol. 2011;128(5):1067–1076.e6. https://doi.org/10.1016/j.jaci.2011.06.018.
Taube C, et al. IL-22 Is Produced by innate lymphoid cells and limits inflammation in allergic airway disease. PLoS One. 2011;6(7):e21799. https://doi.org/10.1371/journal.pone.0021799.
Besnard A, et al. Dual Role of IL-22 in allergic airway inflammation and its cross-talk with IL-17A. Am J Respir Crit Care Med. 2011;183(9):1153–63. https://doi.org/10.1164/rccm.201008-1383oc.
• Badi Y, et al. Is fezakinumab, an anti-IL22 antibody, a putative novel therapy for a subset of severe asthma? Eur Respir J. 2019;54(suppl 63):OA1606. https://doi.org/10.1183/13993003.congress-2019.OA1606 This paper raise a promising orientation for the treatment on asthma.
Fort MM, et al. IL-25 induces IL-4, IL-5, and IL-13 and Th2-associated pathologies in vivo. Immunity. 2001;15(6):985–95. https://doi.org/10.1016/s1074-7613(01)00243-6.
Kim MR, et al. Transgenic overexpression of human IL-17E results in eosinophilia, B-lymphocyte hyperplasia, and altered antibody production. Blood. 2002;100(7):2330–40. https://doi.org/10.1182/blood-2002-01-0012.
Chen F, et al. Nasal interleukin 25 as a novel biomarker for patients with chronic rhinosinusitis with nasal polyps and airway hypersensitiveness: A pilot study. Ann Allergy Asthma Immunol. 2017;119(4):310–316.e2. https://doi.org/10.1016/j.anai.2017.07.012.
• Hong HY, et al. Local IL-25 contributes to Th2-biased inflammatory profiles in nasal polyps. Allergy. 2018;73(2):459–69. https://doi.org/10.1111/all.13267 This paper nicely present the proof of the role of IL-25 in the pathogenesis of chronic sinusitis.
• Shin H, et al. IL-25 as a novel therapeutic target in nasal polyps of patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2015;135(6):1476–85. https://doi.org/10.1016/j.jaci.2015.01.003 This is an excellent paper which suggest the novel possibility of treating nasal polyposis with anti IL-25 therapy.
Corren J, et al. Tezepelumab in adults with uncontrolled asthma. N Engl J Med. 2017;377(10):936–46. https://doi.org/10.1056/nejmoa1704064.
• Gauvreau GM, et al. Effects of an anti-TSLP antibody on allergen-induced asthmatic responses. N Engl J Med. 2014;370(22):2102–10. https://doi.org/10.1056/nejmoa1402895 A meaningful pilot trial for anti-TSLP therapy.
Schmitz J, et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity. 2005;23(5):479–90. https://doi.org/10.1016/j.immuni.2005.09.015.
Smith DE. IL-33 meets allergens at the gate. Nat Immunol. 2018;19(4):318–20. https://doi.org/10.1038/s41590-018-0069-3.
• Shaw JL, et al. IL-33-responsive innate lymphoid cells are an important source of IL-13 in chronic rhinosinusitis with nasal polyps. Am J Respir Crit Care Med. 2013;188(4):432–9. https://doi.org/10.1164/rccm.201212-2227oc This is an very good explanation for the Mechanism of action of IL-33.
Oboki K, et al. IL-33 is a crucial amplifier of innate rather than acquired immunity. Proc Natl Acad Sci U S A. 2010;107(43):18581–6. https://doi.org/10.1073/pnas.1003059107.
Chen YL, et al. Proof-of-concept clinical trial of etokimab shows a key role for IL-33 in atopic dermatitis pathogenesis. Sci Transl Med. 2019;11(515):eaax29. https://doi.org/10.1126/scitranslmed.aax2945.
• Chinthrajah S, et al. Phase 2a randomized, placebo-controlled study of anti-IL-33 in peanut allergy. JCI Insight. 2019;4(22):e131347. https://doi.org/10.1172/jci.insight.131347 This is an challenging and promising clinical trials for anti-IL-33 treatment.
Holgate ST, et al. Efficacy and safety of a recombinant anti-immunoglobulin E antibody (omalizumab) in severe allergic asthma. Clin Exp Allergy. 2004;34(4):632–8. https://doi.org/10.1111/j.1365-2222.2004.1916.x.
Wenzel S, et al. Dupilumab efficacy and safety in adults with uncontrolled persistent asthma despite use of medium-to-high-dose inhaled corticosteroids plus a long-acting β2 agonist: a randomised double-blind placebo-controlled pivotal phase 2b dose-ranging trial. Lancet. 2016;388(10039):31–44. https://doi.org/10.1016/s0140-6736(16)30307-5.
Numata T, et al. Efficacy of mepolizumab for patients with severe asthma and eosinophilic chronic rhinosinusitis. BMC Pulm Med. 2019;19(1):176. https://doi.org/10.1186/s12890-019-0952-1.
Pavord ID, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet. 2012;380(9842):651–9. https://doi.org/10.1016/s0140-6736(12)60988-x.
Funding
This study was supported by the Natural Science Foundation of Guangdong Province (No. 2018A030313399) and the National Natural Science Foundation of China (No. 82071018).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Yingxiang Xu, Mingmin Bi, Kai Sen Tan, Jiaoping Mi, and Haiyu Hong declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Allergy Prevention
Rights and permissions
About this article
Cite this article
Xu, Y., Bi, M., Tan, K.S. et al. Biologics in Treatment for Chronic Rhinosinusitis with Comorbid Asthma. Curr Treat Options Allergy 8, 133–146 (2021). https://doi.org/10.1007/s40521-021-00282-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40521-021-00282-2