Abstract
Background
Clinical severity of pneumonia in older persons increases the risk for short-term mortality. Comprehensive geriatric assessment (CGA) may provide further insight in prognostic stratification.
Aims
To investigate whether CGA may improve prognostic stratification among older patients with pneumonia admitted to hospital.
Methods
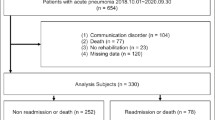
Our series consisted of 318 consecutive patients hospitalized for pneumonia in a multicenter observational study. Disease severity was assessed by Sequential Organ Failure Assessment (SOFA) and Pneumonia Severity Index (PSI). CGA included the occurrence of delirium, Basic Activities of Daily Living (BADL) disability, cognitive impairment at Short Portable Mental Status Questionnaire (SPMSQ) and overall comorbidity assessed by Cumulative Illness Rating Scale (CIRS). The outcomes were in-hospital and post-discharge 3 month mortality. Statistical analysis was carried out by Cox regression, area under receiver operating curve (AUC) and net reclassification index (NRI).
Results
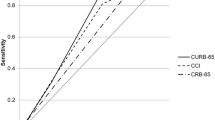
Overall, 53 patients died during hospitalization and 52 after discharge. Delirium, SOFA score and admission BADL disability were significant predictors of in-hospital mortality. SOFA score, CIRS, previous long-term oxygen therapy and discharge BADL dependency significantly predicted post-discharge mortality. The accuracy of SOFA in predicting in-hospital and post-discharge mortality was fair (AUC = 0.685, 95% CI = 0.610–0.761 and AUC = 0.663, 95% CI = 0.593–0.734, respectively). BADL dependency and delirium improved predictive accuracy for in-hospital mortality (ΔAUC = 0.144, 95% CI = 0.062–0.227, p < 0.001), while pre-admission oxygen therapy, CIRS and BADL dependency improved predictivity for 3 month mortality (ΔAUC = 0.177, 95% CI = 0.102–0.252, p < 0.001).
Discussion
Among older pneumonia patients, prognostic stratification obtained by clinical severity indexes is significantly improved by CGA risk factors.
Conclusions
CGA provides important information for prognostic stratification and clinical management of older pneumonia patients.
Similar content being viewed by others
References
Laporte L, Hermetet C, Jouan Y et al (2018) Ten-year trends in intensive care admissions for respiratory infections in the elderly. Ann Intensive Care 8:84
Kaplan V, Clermont G, Griffin MF et al (2003) Pneumonia: still the old man’s friend? Arch Intern Med 163:317–323
Kothe H, Bauer T, Marre R et al (2008) Outcome of community-acquired pneumonia: influence of age, residence status and antimicrobial treatment. Eur Respir J 32:139–146
Capelastegui A, Espana PP, Quintana JM et al (2009) Development of a prognostic index for 90-day mortality in patients discharged after admission to hospital for community-acquired pneumonia. Thorax 64:496–501
Ma HM, Tang WH, Woo J (2011) Predictors of in-hospital mortality of older patients admitted for community-acquired pneumonia. Age Ageing 40:736–741
Corrao S, Argano C, Natoli G et al (2018) Disability, and not diabetes, is a strong predictor of mortality in oldest old patients hospitalized with pneumonia. Eur J Intern Med 54:53–59
Torres OH, Munoz J, Ruiz D et al (2004) Outcome predictors of pneumonia in elderly patients: importance of functional assessment. J Am Geriatr Soc 52:1603–1609
Kaplan V, Angus DC, Griffin MF et al (2002) Hospitalized community-acquired pneumonia in the elderly: age- and sex-related patterns of care and outcome in the United States. Am J Respir Crit Care Med 165:766–772
Metersky ML, Waterer G, Nsa W et al (2012) Predictors of in-hospital vs postdischarge mortality in pneumonia. Chest 142:476–481
Ruiz LA, Zalacain R, Capelastegui A et al (2014) Bacteremic pneumococcal pneumonia in elderly and very elderly patients: host- and pathogen-related factors, process of care, and outcome. J Gerontol A Biol Sci Med Sci 69:1018–1024
Fernandez-Sabe N, Carratala J, Roson B et al (2003) Community-acquired pneumonia in very elderly patients: causative organisms, clinical characteristics, and outcomes. Medicine (Baltimore) 82:159–169
Garcia-Ordonez MA, Garcia-Jimenez JM, Paez F et al (2001) Clinical aspects and prognostic factors in elderly patients hospitalised for community-acquired pneumonia. Eur J Clin Microbiol Infect Dis 20:14–19
Waterer GW, Kessler LA, Wunderink RG (2006) Delayed administration of antibiotics and atypical presentation in community-acquired pneumonia. Chest 130:11–15
Wunderink RG, Waterer GW (2014) Community-acquired pneumonia. N Engl J Med 370:1863
Venditti M, Falcone M, Corrao S et al (2009) Outcomes of patients hospitalized with community-acquired, health care-associated, and hospital-acquired pneumonia. Ann Intern Med 150:19–26
Falcone M, Venditti M, Shindo Y et al (2011) Healthcare-associated pneumonia: diagnostic criteria and distinction from community-acquired pneumonia. Int J Infect Dis 15:e545–e550
American Thoracic Society; Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171:388–416
Mandell LA, Wunderink RG, Anzueto A et al (2007) Infectious diseases society of America/American thoracic society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 1:S27–S72
Fimognari FL, Corsonello A, Pilotto A et al (2016) Community acquired pneumonia in the elderly: the pneumonia in Italian acute care for elderly units (PIACE) study protocol by the Italian Society of Hospital and Community Geriatrics (SIGOT). Geriatr Care 2:6569
Falcone M, Russo A, Giannella M et al (2015) Individualizing risk of multidrug-resistant pathogens in community-onset pneumonia. PLoS ONE 10:e0119528
Katz S, Downs TD, Cash HR et al (1970) Progress in development of the index of ADL. Gerontologist 10:20–30
Pfeiffer E (1975) A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 23:433–441
Linn BS, Linn MW, Gurel L (1968) Cumulative illness rating scale. J Am Geriatr Soc 16:622–626
Vincent JL, Moreno R, Takala J et al (1996) The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Med 22:707–710
Ferreira FL, Bota DP, Bross A et al (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286:1754–1758
Fine MJ, Auble TE, Yealy DM et al (1997) A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 336:243–250
Simonetti AF, Viasus D, Garcia-Vidal C et al (2014) Management of community-acquired pneumonia in older adults. Ther Adv Infect Dis 2:3–16
Metlay JP, Schulz R, Li YH et al (1997) Influence of age on symptoms at presentation in patients with community-acquired pneumonia. Arch Intern Med 157:1453–1459
Rello J, Rodriguez R, Jubert P et al (1996) Severe community-acquired pneumonia in the elderly: epidemiology and prognosis study group for severe community-acquired pneumonia. Clin Infect Dis 23:723–728
Fimognari FL, Pierantozzi A, De Alfieri W et al (2017) The severity of acute illness and functional trajectories in hospitalized older medical patients. J Gerontol A Biol Sci Med Sci 72:102–108
Metersky ML, Fine MJ, Mortensen EM (2012) The effect of marital status on the presentation and outcomes of elderly male veterans hospitalized for pneumonia. Chest 142:982–987
Rello J, Lujan M, Gallego M et al (2010) Why mortality is increased in health-care-associated pneumonia: lessons from pneumococcal bacteremic pneumonia. Chest 137:1138–1144
Acknowledgements
PIACE Study Group Collaborators: Filippo Luca Fimognari, Massimo Rizzo, Olga Cuccurullo, Giovanna Cristiano, Valentina Bambara, Andrea Arone, Andrea Corsonello, Bruno Mazzei, Giorgio Maiuri, Silvio Vena, Giovanni Ruotolo, Alfonso Merante, Giuliano Ceschia, Gabriele Toigo, Francesco Di Grezia, Immacolata Alviggi, Maurizio Luchetti, Rosa Maria Mereu, Olga Catte, Vittoria Tibaldi, Alberto Ferrari, Luca Carpi, Maria Lia Lunardelli, Pasquale Vizzo, Emilio Martini, Alfredo Zanatta, Giorgio Gasperini, Chiara Pavan, Francesco De Filippi, Michela Passamonte, Anna Nardelli, Sandra Visioli, Fabrizio Franchi, Marco Masina, Antonio Cherubini, Antonia Scrimieri, Demetrio Postacchini, Roberto Brunelli, Gianfranco Conati, Eleonora Ruberto, Alberto Pilotto, Mario Lo Storto, Paolo Chioatto, Maria Rita Gulino, Michele Pagano, Giovanna Crupi, Biagio Ierardi, Bruno Provenzano.
Funding
PIACE study was performed without any funding.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest regarding the study.
Ethical approval
The study protocol of PIACE study was examined and approved by the Institutional Ethical Committee of the coordinating center (Unit of Geriatrics, Annunziata Hospital, Azienda Ospedaliera di Cosenza, Cosenza, Italy). The approved protocol was transmitted to all participating centers; the Institutional Ethical Committee of each center could ask for clarifications of the protocol.
Statement of human and animal rights
This is an observational study conducted in humans. All patients or their surrogates provided written informed consent.
Informed consent
All enrolled patients or their surrogates provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The PIACE study group collaborators are listed in the acknowledgments section.
Rights and permissions
About this article
Cite this article
Fimognari, F.L., Corsonello, A., Rizzo, M. et al. Contribution of clinical severity and geriatric risk factors in predicting short-term mortality of older hospitalized pneumonia patients: the Pneumonia in Italian Acute Care for Elderly units (PIACE) study. Aging Clin Exp Res 34, 1419–1427 (2022). https://doi.org/10.1007/s40520-021-02063-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-02063-y