Abstract
Wearable fitness trackers are an increasingly popular tool for measuring physical activity (PA) due their accuracy and momentary data collection abilities. Despite the benefits of using wearable fitness trackers, there is limited research in the eating disorder (ED) field using wearable fitness trackers to measure PA in the context of EDs. Wearable fitness trackers are often underused in ED research because there is limited knowledge about whether wearable fitness trackers negatively or positively impact PA engagement and ED symptoms in individuals with EDs. The current study aimed to assess the perceived impact wearable fitness trackers have on PA engagement and ED symptoms over a 12-week CBT treatment for 30 individuals with binge eating and restrictive eating that presented to treatment engaging or not engaging in maladaptive exercise. Participants in the maladaptive exercise group (n = 17) and non-maladaptive exercise group (n = 13) wore a fitness tracker for 12 weeks and completed questionnaires assessing participants’ perceptions of the fitness trackers’ influence on ED symptoms and PA engagement throughout treatment. Results demonstrated a small percentage of individuals perceived the fitness tracker influenced ED behaviors or PA engagement, and there were mixed results on whether participants positively or negatively perceived the fitness tracker influenced them to engage in ED behaviors or PA engagement. Although preliminary, these results demonstrate the need to continue using objective measurements of PA via wearable fitness trackers to further our understanding of the positive and negative effects of fitness trackers on clinical ED samples.
Level of Evidence: Level 1, randomized controlled trial.
Similar content being viewed by others
Introduction
Exercise in the context of eating disorders (EDs) can be either maladaptive (i.e., used to compensate for binge eating [compensatory] or feels compelled to avoid negative consequences of not exercising such as weight gain[driven]; [5, 14, 15] or adaptive (i.e., neither driven nor compensatory; [9]13). The inclusion of fitness trackers in research studies may be a useful methodology in understanding objective characteristics of overall physical activity (PA: any physical movement) in EDs (e.g., duration, frequency, intensity) including intentional exercise episodes, but such methods are underutilized in research studies to-date due to concerns about participant reactivity to trackers. The current study aims to improve understanding of the perceived impact of fitness trackers on ED symptoms and PA engagement in an ED population to evaluate the safety and potential efficacy of use for research studies.
Use of fitness trackers in extant research
There is a growing literature base examining PA in the context of EDs. To date, most research on PA in ED populations has relied on retrospective self-report measures of PA frequency and duration [1]. These retrospective self-report measures are subject to several biases, such as recall bias (e.g. forgetting) and social desirability bias (e.g. over/underreporting) [1]. Other literature has used ecological momentary assessment (EMA) to examine PA in EDs. While EMA reporting reduces recall errors, it is still subject to social desirability bias. Extant literature supports these concerns; self-report measurements of PA have been found to be inaccurate both in ED groups and in the general adult population [1, 12, 16].
Objective measurement of PA via sensors (e.g., accelerometry) shows great promise for a more accurate measurement of PA engagement in ED populations. Sensor-based assessment tools (e.g., wearable fitness trackers) use objective measurement, more accurately measure the amount of PA, and increase the credibility and validity of research findings [7, 12]. Despite these strong benefits of objective PA measurement, few studies have objectively measured the amount of PA cross sectionally [2, 12]. There are 2 main reasons why the ED field tends to under-use objective measures of PA in research assessment. First, many characteristics of both maladaptive and adaptive exercise are cognitive in nature, and prior research suggests these cognitive components of exercise are more clinically relevant in defining maladaptive exercise as compared to exercise frequency and duration [3]. For example, wearable fitness trackers cannot measure a sense of being compelled or driven to continue exercise or the intended reason for exercise. As a result, researchers cannot presently depend on wearable fitness trackers to distinguish adaptive from maladaptive exercise, though they can use these devices to gain objective data about other important exercise features such as duration and intensity. Second, researchers and clinicians are often concerned about the potential negative effects wearable fitness trackers could have on the development and maintenance of ED symptoms [18]. Thus, the use of fitness trackers in ED research has remained limited.
Despite concerns about reactivity to sensor measurement of PA among individuals with EDs, little research has specifically examined this phenomenon. To date, only three studies have tested the effects of a wearable fitness trackers on ED symptoms in non-clinical populations, with mixed results. Two were observational studies of university students or young adults which found fitness tracker devices and apps (e.g., Fitbit) were associated with ED symptomatology (e.g., rates of binge eating or purging) and higher rates of body dissatisfaction [8, 18]. The third study assigned half their sample of university students to wear fitness trackers and found those that were assigned to wear fitness trackers were more likely to report exercising to support their health and fitness and were less likely to report engagement in ED behaviors (e.g., dietary restraint, binge eating) [6]. A major limitation of all the studies described above is that none of them included individuals with a diagnosed ED. Despite the valuable contributions of the aforementioned studies, it remains unknown how using wearable fitness trackers impacts individuals with EDs, specifically.
Patient perceptions of influence of fitness trackers on ED behaviors
In addition to the field’s limited understanding of the relationship between wearable fitness trackers, ED symptoms, and PA engagement, no study has assessed the perceived impact of fitness trackers on ED symptoms and PA engagement over an extended period (e.g., > 10 days), nor throughout the course of an ED treatment. Importantly, there could be increased reactivity during the first few days of wear as compared to longer-term wear of fitness trackers. Assessing the perceived impact of a fitness tracker on PA engagement and ED symptoms during an ED treatment will allow for the opportunity to further understand the perceived impact of the fitness tracker at the start of treatment when ED symptoms are likely more severe or during the treatment when ED symptoms are likely subsiding.
Influence of maladaptive exercise on fitness tracker reactivity
To date, research has also not assessed the perceived influence of fitness trackers on PA engagement and ED symptoms separately in individuals with EDs that do and do not engage in maladaptive exercise. It is possible the perceived impact of fitness trackers may be different among those with and without maladaptive exercise as these groups tend to show different symptom presentations prior to treatment [11, 17, 19]. Further, reductions in maladaptive exercise facilitated by treatment may lead to the decreased perceived influence of the fitness tracker on PA due to overall reductions in the amount of PA. Assessing the perceived impact of fitness trackers on PA engagement and ED symptoms during an ED treatment may reveal whether specific ED symptoms, like maladaptive exercise, predict whether an individual perceives the fitness tracker to positively or negatively impact their ED symptoms and/or PA engagement.
Current study
The current study aimed to characterize participants’ perception of the fitness tracker’s influence on ED symptoms across a 12-week CBT treatment for individuals with an ED characterized by both clinically significant binge eating and restrictive eating. There were 2 aims of the current study and each aim consisted of two parts. Aim 1a was to describe session-by-session perception of the fitness tracker’s influence on overall PA and maladaptive PA among individuals who did and did not engage in maladaptive exercise at pre-treatment. For Aim 1b, we aimed to examine the moderating role of pre-treatment maladaptive exercise engagement on the perceived influence of the fitness tracker on overall PA engagement across treatment. Due to the potentially greater perceived impact of fitness trackers on PA engagement among individuals currently engaging in maladaptive exercise, we hypothesized the individuals that entered treatment engaging in maladaptive exercise would experience greater reductions in the perceived influence of the fitness tracker on PA engagement during treatment compared to those that did not engage in maladaptive exercise at the start of treatment. Aim 2a was to characterize session-by-session perception of the fitness trackers influence on ED symptoms among individuals who did and did not engage in maladaptive exercise at pre-treatment. For Aim 2b, we aimed to examine the moderating role of pre-treatment maladaptive exercise engagement on the perceived influence of the fitness tracker on ED symptoms across treatment. We had no specific directional hypotheses for whether the perceived influence of the fitness tracker on ED symptoms would differ throughout the course of treatment between those that did and did not engage in maladaptive exercise at the start of treatment.
Methods
Participants and recruitment
Participants (n = 30) ages 18 years and older were recruited via referrals from internal and external health care clinics, flyers, newspapers, radio, and online postings including social media campaigns from May 2020 to June 2021. Sample characteristics are presented in Table 1. Participants were recruited to participate in a larger parent study (ClinicalTrials.gov Identifier: NCT04126694; R43 MH121205) designed to test the feasibility and acceptability of a novel sensor-based smartphone application when used as an adjunct to CBT for adult patients with transdiagnostic binge eating and restrictive eating pathology. Participants were included if they were 18–65 years of age, experienced clinically significant binge eating (defined as 12 or more objectively large binge eating episodes in the past 3 months), engaged in clinically significant dietary restriction (defined as 3 or more episodes of fasting for 5 or more waking hours per week in the last 4 weeks), had a body mass index (BMI) 17.5–35, and were willing and able to use a wearable fitness tracker every day for 12 weeks. Participants were excluded if they were receiving other treatment for an ED, were receiving structured behavioral weight loss treatment (e.g., Weight Watchers), or required immediate treatment for medical complications as a result of ED symptoms.
Procedure
All assessments were completed virtually due to the COVID-19 pandemic. Data for the current study was collected at each assessment point and weekly with the therapy sessions. Participants completed an initial phone screening, a baseline assessment, mid-treatment assessments after session four and session, 8 and a post-treatment assessment after session 12. At the baseline assessment participants were categorized into two groups based on their responses to questions about maladaptive exercise: (1) the maladaptive exercise group (n = 17) and 2) the non-maladaptive exercise group (n = 13). Participants were categorized into the maladaptive exercise group if they engaged in at least one maladaptive exercise episode during the 12 weeks leading up to the baseline assessment. Participants also completed a weekly pre-session questionnaire before every therapy session. Informed consent was obtained by a study assessor from each participant at the baseline assessment. At the baseline assessment, participants were given the Mi Smart Band, a wearable fitness tracker, and they were instructed to wear the tracker throughout the entirety of the 12-week treatment. When participants noticed the battery was running low on the fitness trackers (approximately every twenty days), they were instructed to charge the tracker either when showering or during a time when they were not exercising or sleeping. Of the 12 therapy sessions, only the fourth session focused on addressing maladaptive exercise behaviors for individuals that presented to treatment engaging in maladaptive exercise. The current study was conducted in compliance with the Drexel University Institutional Review Board.
Measures
Eating disorder examination (EDE)
The EDE is a semi-structured clinician-administered interview [4]. The current study used the EDE for diagnostic purposes and to assess adaptive and maladaptive exercise at the baseline assessment. The study team modified the EDE to separately assess adaptive and maladaptive exercise. In the modified EDE, assessors asked questions generated by our research team that separately assess the duration and frequency of solely adaptive exercise episodes and the duration and frequency of all maladaptive exercise episodes, which included driven exercise only episodes, compensatory exercise only episodes, and driven and compensatory exercise episodes. Adaptive exercise was defined as any exercise that was neither driven nor compensatory. If the primary motive for an exercise episode was for shape/weight reasons and was perceived by the participant and assessor as driven or compensatory, then it was counted as maladaptive exercise. Adaptive exercise was not assessed directly. Thus, assessors first assessed a participant’s total exercise pattern (i.e., frequency and duration of all exercise) and then assessed the participant’s exercise pattern of maladaptive exercise episodes. Once this information was collected, assessors subtracted frequencies of maladaptive exercise episodes from the frequency of the total exercise routine episode frequency to determine whether participants were engaging in any exercise that was not primarily maladaptive and the frequency of the participant’s adaptive exercise episodes. During the assessment, the assessors oriented the participants to maladaptive exercise episodes by explaining to the participants how to classify exercise episodes that are driven and/or compensatory and exercise episodes that are not. We used some of the following descriptions to help participants classify their maladaptive exercise episodes: the exercise felt driven or compelled, the exercise was hard or strenuous, they pushed themselves during the exercise, they chose to exercise over prior commitments, they exercised when it may have caused harm such as when injured or sick, and they felt strong negative emotions (e.g., guilt, anxiety) if they were unable to exercise. This explanation often helped participants both differentiate what exercise episodes from their total exercise routine were maladaptive and account for the duration and frequency of maladaptive exercise episodes.
MiFit smart band
The MiFit smart band is a wearable fitness tracker that collects daily step count and heart rate. The corresponding MiFit app recorded and compiled this data. Participants had access to the MiFit app on their phone and occasionally had to open the app to sync data for study purposes. Participants wore the MiFit smart band on the wrist of their choice during the 12-week study. The MiFit smart band has a small rectangular screen which was a touch screen and displayed the date and time. Using the touch screen, participants were able to access their steps count, heart rate, distance moved, and sleep duration. Participants were asked to not look at the data they had access to on the watch and the MiFit application on their phone. Participants were not directly told what data was being collected for the purpose of the study. Participants were also asked to not wear any additional wearable fitness trackers they own during the duration of the study.
Perceived fitness tracker reactivity and influence on ED symptoms
Participants’ perceived influence of the fitness tracker on PA engagement and ED symptoms were assessed through two measures developed for the purposes of this study. This included a 3-item weekly pre-session questionnaire and a 5-item mid-treatment and post-treatment questionnaire measuring two constructs: (1) perceived fitness tracker reactivity and (2) the perception of the fitness trackers influence on ED symptoms. The specific items used to measure perceived fitness tracker reactivity [6], Maher, Ryan, Ambrosi, & Edney, 2017) and perception of influence on ED symptoms [6, 8, 18] were based on previous work that similarly assessed these constructs.
Perceived fitness tracker reactivity was defined as the degree to which wearing a fitness tracker influenced overall PA or maladaptive PA engagement. The primary question asked to assess perceived fitness tracker reactivity was the following: “Did the fitness tracker motivate you to engage in physical activity this week?” If participants responded yes, they were prompted with two follow-up questions: 1) “If yes, did the fitness tracker motivate you to engage in exercise that was driven or compelled?” and 2) “If yes, did the fitness tracker motivate you to engage in exercise that was to compensate or make up for a binge eating episode?” Perceived fitness tracker reactivity was measured weekly via the patient’s pre-session questionnaire, at both mid-treatment assessments, and post-treatment assessment.
Perception of fitness tracker influence on ED symptoms was defined as the degree to which participants perceived wearing a fitness tracker influenced whether they engage in ED symptoms. The perception of the fitness trackers influence on ED symptoms was assessed using two questions: (1) “Over the last 4 weeks, did the fitness tracker influence you to binge eat or not to binge eat?” and (2) “Over the last 4 weeks, did the fitness tracker influence you to restrict or not restrict your food intake?” Participants had three response options for each question: (1) “Yes, the fitness tracker influenced me to engage in the ED behavior,” (2) “Yes, the fitness tracker influenced me to not engage in the ED behavior,” and (3) “No, the fitness tracker did not influence me to engage or not engage in the ED behavior.” Perceived influence on ED symptoms was only measured at the two mid-treatment assessments and post-treatment assessment, not at the baseline assessment or during the weekly pre-session questionnaires.
Statistical analyses
Results were summarized in graphs to demonstrate the percentage of individuals that perceived the fitness tracker influenced them to engage in PA and ED behaviors on a session-by-session basis. Three 2-way repeated measures ANOVAs were run to demonstrate the perceived impact that fitness trackers had on (1) PA, (2) binge eating, and (3) dietary restriction at three-time points across treatment (e.g., session four, session eight, and session (12) between individuals in the maladaptive and non-maladaptive exercise groups. For all repeated measures ANOVAs, we used partial η2 cutoffs to determine small (0.01–0.05), medium (0.06–0.13), and large (≥ 0.14) effect sizes. Effect sizes were used to interpret statistical analyses due to the small sample size and lack of statistical power.
Results
Sample characteristics
Sample characteristics are presented in Table 1. For all results, participants were divided into two groups: (1) those that engaged maladaptive PA at the start of treatment and (2) those that only engaged in non-maladaptive PA or no PA at pre-treatment. No participant reported a serious injury or illness that limited their ability to engage in PA during treatment. In the maladaptive exercise group, participants reported engaging in an average frequency of 18.12 (SD = 17.17) maladaptive exercise episodes for an average duration of 53.18 (SD = 39.69) minutes and an average frequency of 10.06 (SD = 2.29) adaptive exercise episodes for an average duration of 24.85 (SD = 24.07) minutes over the 12 weeks leading up to the pre-treatment assessment. In the non-maladaptive exercise group, participants reported engaging in an average frequency of 13.00 (SD = 13.06) adaptive exercise episodes for an average duration of 33.29 (SD = 31.57) minutes over the 12 weeks leading up to the pre-treatment assessment.
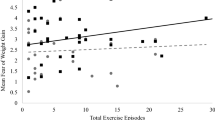
Aim 1a: characterization of session-by-session perception of fitness tracker influence on PA engagement
Figure 1 demonstrates the percentage of individuals that reported the fitness tracker motivated them to engage in PA on a session-by-session basis. Both the maladaptive and non-maladaptive exercise groups demonstrated similar patterns for the percentage of individuals that reported feeling like the fitness tracker motivated them to engage in PA during treatment. There was also considerable variability in both the maladaptive and non-maladaptive exercise groups from session to session with the percentage of individuals that reported feeling like the fitness tracker motivated them to engage in PA during treatment. From visual inspection, both the maladaptive and non-maladaptive exercise groups demonstrated reduction trends in the percentage of individuals that reported feeling like the fitness tracker motivated them to engage in PA during treatment.
Figure 2 displays the percentage of individuals in the maladaptive exercise group that reported the fitness tracker motivated them to engage in driven or compensatory PA on a session-by-session basis. No individuals in the non-maladaptive exercise group reported they perceived the fitness tracker influenced them to engage in maladaptive exercise. In session one, 18% of individuals in the maladaptive exercise group reported they perceived the fitness tracker influenced them to engage in driven exercise but in session 12, 0% of individuals in the maladaptive exercise group they perceived the fitness tracker influenced them to engage in driven exercise. A similar pattern existed with compensatory exercise; 24% of individuals in the maladaptive exercise group reported they perceived the fitness tracker influenced them to engage in compensatory exercise at session 1 but at session 12, 0% of individuals in the maladaptive exercise group they perceived the fitness tracker influenced them to engage in compensatory exercise.
Aim 1b: the moderating role of pre-treatment maladaptive exercise engagement on the perceived influence of the fitness tracker on overall PA engagement across treatment
Although not significant, there was a moderate interaction effect demonstrating there was a greater reduction in the number of individuals in the maladaptive exercise group that perceived the fitness tracker influenced them to engage in PA during treatment compared to the non-maladaptive exercise group (F(2) = 1.76, p = 0.18, η2 = 0.07).
Aim 2a: characterization of fitness tracker influence on ED behaviors across treatment
Figure 3 demonstrates the percentage of individuals that reported the fitness tracker influenced them to not binge eat. Across both groups, no participants reported the fitness tracker influenced them to binge eat, therefore, the results shown in Fig. 3 only demonstrate the percentage of individuals that responded the fitness tracker influenced them to not binge eat. The percentage of individuals that responded to the fitness tracker influenced them to not binge eat at the two mid-treatment and post-treatment assessments for the maladaptive exercise group was 13%, 7%, and 18%, respectively, and 8%, 0% and 0%, respectively, for the non-maladaptive exercise group.
Figure 4 demonstrates the percentage of individuals that reported the fitness tracker influenced them to restrict or not restrict their eating. The percentage of individuals that responded to the fitness tracker influenced them to not restrict at the session 4, 8, and 12 assessments for the maladaptive exercise group was 0%, 7%, and 9%, respectively, and 8%, 0% and 0%, respectively, for the non-maladaptive exercise group. Only individuals in the maladaptive exercise group reported perceiving that the fitness tracker influenced them to restrict. The percentage of individuals that responded to the fitness tracker influenced them to restrict at the 2 mid-treatment and post-treatment assessments for the maladaptive exercise group were 12%, 0%, and 9%, respectively.
Aim 2b: the moderating role of pre-treatment maladaptive exercise engagement on the perceived influence of the fitness tracker on ED symptoms across treatment
There were no significant results when comparing the influence of the fitness tracker on binge eating between the maladaptive and non-maladaptive exercise groups across treatment (F(2) = 0.97, p = 0.39, η2 = 0.04). Although not significant, there was a moderate interaction effect demonstrating more individuals in the maladaptive exercise group perceived the fitness tracker influenced them to not restrict their food intake compared to the non-maladaptive exercise group across treatment (F(2) = 2.00, p = 0.15, η2 = 0.09).
Discussion
The current study assessed the perceived influence wearable fitness trackers have on PA and ED symptoms in 30 treatment-seeking individuals with an ED characterized by recurrent binge eating and restrictive eating over a 12-week CBT treatment. About half of the total sample reported they perceived the fitness tracker influenced them to engage in PA, which is comparable to what similar studies in non-clinical ED samples have found [10]. Patterns of responses seemed to demonstrate the perceived influence the fitness tracker had on motivating individuals to engage in PA varied session-to-session and seemed to have similar variation patterns for both the maladaptive and non-maladaptive exercise groups. It is possible the introduction of specific session content (e.g., introduction to weighing, overvaluation of weight and shape) influenced some of the session-to-session variability. Specifically, certain session content (e.g., addressing shape and weight concerns during sessions nine and 10) may have explained why the percentages were low for both groups in 1 week and high for both groups the next week.
Within the maladaptive exercise group, a relatively small percentage of individuals reported perceiving the fitness trackers influenced them to engage in maladaptive PA. Response patterns demonstrated there was variability session-to-session for the perceived impact on both compensatory and driven exercise but, ultimately, by the end of treatment no individuals reported perceiving the fitness tracker was motivating them to engage in maladaptive exercise. It is possible the participants’ relationship with the fitness tracker changed or they did not feel impacted because the maladaptive exercise was no longer an ED symptom by the end of treatment. More specifically, 12 of the 17 individuals in the maladaptive exercise group were not engaging in maladaptive exercise by the end of the treatment. This suggests fitness trackers may not interfere with one’s ability to stop engaging in maladaptive exercise during an ED treatment.
In line with our hypothesis, the maladaptive exercise group demonstrated a larger decrease in the perceived impact of the fitness tracker on PA engagement compared to the non-maladaptive group. This result may be due to the maladaptive exercise group reducing their amount of maladaptive PA over treatment, which would impact their amount of overall PA. If they were engaging in less overall PA as treatment continued, then there may have been less opportunities where they felt the watch was influencing PA engagement.
Given some individuals with EDs seem to experience positive effects while others experience negative effects from fitness trackers on overall PA engagement and maladaptive PA, it is difficult to draw conclusions on whether fitness trackers are beneficial or harmful for individuals with EDs, which is in line with the mixed literature on the impact of fitness trackers in non-clinical ED populations [6, 8, 10, 18]. It seems possible that with caution and proper psychoeducation, fitness trackers may be able to benefit some individuals with EDs and help promote individuals receiving CBT-E to engage in greater levels of overall adaptive PA. Further, general trends demonstrated the individuals perceived the fitness trackers influenced them to engage in physical activity more towards the beginning of treatment and gradually decreased over the 12-week treatment. This trend may show that treatment had no impact on perceptions of the influence of the fitness tracker but rather participants habituated to wearing the fitness tracker and felt less influenced by it as time progressed. Future research should assess habituation to fitness trackers in an ED sample over an extended period (i.e., < 12 weeks), replicate these findings, and assess the perceived impact of fitness trackers on maladaptive PA, adaptive PA, and overall PA separately across treatment.
Additionally, a small proportion of individuals reported they perceived the fitness tracker had a positive impact on ED symptoms (i.e., influenced them not to engage in ED behaviors) while another small proportion of individuals reported they perceived the fitness tracker had a negative impact on ED symptoms (i.e., influenced them to engage in ED behaviors). It is possible that for a small number of individuals, the fitness trackers were helpful in encouraging adaptive behavior change, like limiting binge eating. This supports previous work in a non-clinical ED sample, which found users of fitness trackers were less likely to report engagement in ED behaviors compared to individuals who did not use fitness trackers [6]. On the other hand, for a small number of individuals in the maladaptive exercise group, they continued to perceive the fitness tracker influenced them to restrict their intake even though they were no longer reporting that they perceived the fitness tracker influenced them to engage in maladaptive exercise. One possible explanation for this finding is that even though individuals were not instructed to look at their watch's metrics, they had access to the watch's metrics and may have chosen to disregard or forgot this instruction. Thus they may have used general physical activity metrics like step count on their watch to determine how much they should restrict that day (i.e., the more steps I have taken, the less I need to restrict). Given these varying findings, future research should aim to replicate these findings in a larger study as well as explore the prevalence rate of individuals with EDs that wear fitness trackers during treatment. Doing so may help the field the proportion of individuals with EDs that could benefit or be in harm from wearing fitness trackers during treatment and better understand if there are certain factors that can help us predict whether an individual with an ED will experience positive or negative effects from a fitness tracker.
Overall, some individuals with EDs perceive fitness trackers have an impact on PA engagement or ED symptoms. Although preliminary, the findings suggest there are mixed perceptions on the impact fitness trackers have on individuals with EDs. For a small number of individuals with EDs, it appears they perceive the fitness trackers influence them at times to engage in ED behaviors. Contrarily, for some, fitness trackers may be beneficial in promoting PA that is adaptive, minimizing maladaptive exercise, and reducing binge eating and dietary restriction. Given these results are preliminary, continuing to use objective measurements of PA via wearable fitness trackers is necessary to further our understanding of the positive and negative effects of fitness trackers on clinical ED samples.
Strengths and limits
The current study was the first study to assess the perceived influence of wearable fitness trackers on both physical activity and ED behaviors in a clinical ED sample. Despite the important first step this study took in understanding how wearable fitness trackers may impact individuals with EDs, there are many limitations to note.
First, the sample was small, mostly White, and most individuals identified as female. Further, the study’s inclusion and exclusion criteria for binge eating and restrictive eating was a limiting factor. Notably, the non-maladaptive exercise group included a few individuals not engaging in any exercise, which makes it complicated to interpret the perceived influence of the fitness tracker on PA in both groups. We also did not assess whether participants used fitness trackers before the start of the study. Additionally, participants were instructed to not look at the app associated with the fitness tracker, so the results cannot be generalized to typical consumer fitness tracker use. If individuals had used fitness trackers and a corresponding app that was more invasive and sent notifications to the participant regularly, the results may have differed and may have given more insight to researchers and clinicians on when and how to integrate fitness trackers and apps into their work with ED patients. Finally, the data in the current study were collected during the COVID-19 pandemic, which may be a limitation as some research has suggested many adults did not engage in their typical PA routine (e.g., working out in fitness center, attending in-person fitness classes) (Alomari, Khabour, & Alzoubi, 2020; Zheng et al., 2020). Given these limitations, results should be interpreted with caution as the results may not be generalizable. Thus, future studies should replicate these findings when COVID 19 restrictions are limited or non-existent, in a larger sample with equal sample sizes, and in a more diverse and representative sample of race and sex.
What is already known on this subject?
In non-clinical ED samples, individuals have reported mixed results on whether individuals perceive wearable fitness trackers positively or negatively influence PA engagement or ED behaviors. To date, no study has assessed the perceived impact of fitness trackers on ED symptoms and PA engagement over an extended period (e.g., > 10 days) in a clinical ED population, nor throughout the course of an ED treatment.
What this study adds?
Some individuals with EDs perceive fitness trackers have an impact on PA engagement or ED symptoms. The preliminary findings suggest there are mixed perceptions on the impact fitness trackers have on individuals with EDs. For a small number of individuals with EDs, it appears they perceive the fitness trackers influence them at times to engage in ED behaviors while for others, fitness trackers may be beneficial in promoting PA that is adaptive, minimizing maladaptive exercise, and reducing binge eating and dietary restriction.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bezzina L, Touyz S, Young S, Foroughi N, Clemes S, Meyer C, Hay P (2019) Accuracy of self-reported physical activity in patients with anorexia nervosa: links with clinical features. J Eat Disord 7(1):28. https://doi.org/10.1186/s40337-019-0258-y
Carr MM, Lydecker JA, White MA, Grilo CM (2019) Examining physical activity and correlates in adults with healthy weight, overweight/obesity, or binge-eating disorder. Int J Eat Disord 52(2):159–165. https://doi.org/10.1002/eat.23003
Coniglio KA, Davis L, Sun J, Loureiro N, Selby EA (2021) Detecting pathological exercise in college men: an investigation using latent profile analysis. J Am Coll Health 20:1–5
Cooper Z, Fairburn C (1987) The eating disorder examination: a semi-structured interview for the assessment of the specific psychopathology of eating disorders. Int J Eat Disord 6(1):1–8
Dittmer N, Jacobi C, Voderholzer U (2018) Compulsive exercise in eating disorders: proposal for a definition and a clinical assessment. J Eat Disord 6(1):1–9
Gittus M, Fuller-Tyszkiewicz M, Brown HE, Richardson B, Fassnacht DB, Lennard GR, Krug I (2020) Are fitbits implicated in body image concerns and disordered eating in women? Health Psychol Official J Div Health Psychol Am Psychol Assoc. https://doi.org/10.1037/hea0000881
Grosser J, Hofmann T, Stengel A, Zeeck A, Winter S, Correll CU, Haas V (2020) Psychological and nutritional correlates of objectively assessed physical activity in patients with anorexia nervosa. Eur Eat Disord Rev 28(5):559–570. https://doi.org/10.1002/erv.2756
Honary M, Bell BT, Clinch S, Wild SE, McNaney R (2019) Understanding the role of healthy eating and fitness mobile apps in the formation of maladaptive eating and exercise behaviors in young people. JMIR Mhealth Uhealth 7(6):e14239
Lampe EW, Trainor C, Presseller EK, Michael ML, Payne-Reichert A, Juarascio AS, Manasse SM (2021) Characterizing reasons for exercise in binge-spectrum eating disorders. Eat Behav 43:101558. https://doi.org/10.1016/j.eatbeh.2021.101558
Laranjo L, Ding D, Heleno B, Kocaballi B, Quiroz JC, Tong HL, Bates DW (2021) Do smartphone applications and activity trackers increase physical activity in adults? Systematic review, meta-analysis and metaregression. Br J Sports Med 55(8):422. https://doi.org/10.1136/bjsports-2020-102892
Levallius J, Collin C, Birgegård A (2017) Now you see it, Now you don’t: compulsive exercise in adolescents with an eating disorder. J Eat Disord 5(1):1–9
Mathisen TF, Rosenvinge JH, Friborg O, Pettersen G, Stensrud T, Hansen BH, Sundgot-Borgen J (2018) Body composition and physical fitness in women with bulimia nervosa or binge-eating disorder. Int J Eat Disord 51(4):331–342. https://doi.org/10.1002/eat.22841
Mathisen TF, Sundgot-Borgen J, Bulik CM, Bratland-Sanda S (2021) The neurostructural and neurocognitive effects of physical activity: a potential benefit to promote eating disorder recovery. Int J Eat Disord 54(10):1766–1770
Mond J, Gorrell S (2021) “Excessive exercise” in eating disorders research: problems of definition and perspective, vol 26. Springer, New York
Monell E, Levallius J, Mantilla EF, Birgegård A (2018) Running on empty–a nationwide large-scale examination of compulsive exercise in eating disorders. J Eat Disord 6(1):1–10
Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M (2008) A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act 5:56. https://doi.org/10.1186/1479-5868-5-56
Shroff H, Reba L, Thornton LM, Tozzi F, Klump KL, Berrettini WH, Fichter MM (2006) Features associated with excessive exercise in women with eating disorders. Int J Eat Disord 39(6):454–461
Simpson CC, Mazzeo SE (2017) Calorie counting and fitness tracking technology: associations with eating disorder symptomatology. Eat Behav 26:89–92
Welch E, Birgegård A, Parling T, Ghaderi A (2011) Eating disorder examination questionnaire and clinical impairment assessment questionnaire: general population and clinical norms for young adult women in Sweden. Behav Res Ther 49(2):85–91
Acknowledgements
The authors have no acknowledgments.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute of Mental Health [Using Continuous Glucose Monitoring to Detect and Intervene on Maintenance Factors for Transdiagnostic Binge Eating Pathology (The Sense Support Project), ClinicalTrials.gov Identifier: NCT04126694; R43 MH121205]. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Olivia Wons, Elizabeth Lampe, Anna Gabrielle Patarinski, Katherine Schaumberg, Meghan Butryn, and Adrienne Juarascio declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants.
Consent for publications
The authors declare that they have no conflict of interest. This manuscript has not been previously published, and is not presently under consideration by another journal, and will not be submitted to another journal before a final editorial decision from Eating and Weight Disorders is rendered. The questionnaire and methodology for this study were approved by the Drexel University Institutional Review Board. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wons, O., Lampe, E., Patarinski, A.G. et al. Perceived influence of wearable fitness trackers on eating disorder symptoms in a clinical transdiagnostic binge eating and restrictive eating sample. Eat Weight Disord 27, 3367–3377 (2022). https://doi.org/10.1007/s40519-022-01466-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-022-01466-8