Abstract
Purpose
This study aimed to explore the factorial structure of the Italian Weight Self-Stigma Questionnaire (WSSQ) (Study1); and to test structural validity, internal consistency, test–retest reliability, and measurement invariance of the questionnaire across gender, Body Mass Index (BMI), age and occurrence of previous hospitalization for obesity (Study2).
Methods
At admission into a hospital-based program for weight reduction and rehabilitation, 150 inpatients with overweight/obesity (68% females) completed the WSSQ (Study1). In Study2, in addition to the WSSQ, 446 inpatients (61.9% females) completed the Weight Bias Internalization Scale (WBIS), the Body Uneasiness Test (BUT), and the Center for Epidemiologic Studies Depression Scale (CES-D). A subsample of 40 patients also re-completed the WSSQ at discharge from the hospital.
Results
The Italian WSSQ showed good overlap with the original factorial structure (Study1) and results were confirmed in Study2. Test–retest reliability and convergent validity showed adequate values. Measurement invariance revealed that WSSQ was perfectly invariant across both BMI and the occurrence of previous hospitalizations for obesity. In both studies, the internal consistency of the questionnaire was deemed acceptable.
Conclusions
The Italian WSSQ is a valid, reliable, and invariant tool for the assessment of weight-related self-stigma among patients with overweight/obesity. Future studies should assess its longitudinal invariance as well as its responsiveness to weight reduction treatments.
Level of evidence
V, descriptive study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overweight and obesity are chronic conditions [1] that affect over 600 million people worldwide [2,3,4,5]—including the elderly population [6,7,8,9].
Besides these alarming rates, several studies showed that the prevalence of weight stigmatization has rapidly increased during the last 20 years [10,11,12,13,14]. Indeed, people with overweight and obesity are regularly exposed to weight-related negative bias and discrimination in everyday life [12, 15] such as workplace, educational, and health care settings, in the media as well as in interpersonal relationships [16]. As a consequence of this continuous exposure to weight stigma, people with overweight and obesity tend to internalize these biases [17,18,19].
The internalization of weight sigma (IWS) leads individuals with overweight and/or obesity to self-stigmatize themselves, thus confirming main negative weight stereotypes [13, 18]—such as failure to keep self-control [20], blame, incompetence [21], and lack of self-discipline—further increasing their risk of being socially devaluated and/or rejected [12, 15, 16]. Moreover, IWS plays a fundamental role in non-adherence to weight loss programs [22]—which in turn contributes to increasing stigma and further promotes weight gain—as is was also observed in patients undergoing bariatric surgery [23]. IWS is also associated with adverse health outcomes including cardiovascular diseases, hypertension, osteoarthritis, and diabetes [24, 25], and it is also strongly related to poor quality of life as well as psychological/psychiatric disorders, such as depression, anxiety, distress, somatization, and eating problems [17, 18, 26,27,28,29].
Despite multidisciplinary interventions have been developed to improve weight loss and to reduce IWS [30,31,32,33,34], the extent to which weight self-stigma affects health outcomes is still unclear [26, 27]. To fill the knowledge gaps in the particular field, the Weight Self-Stigma Questionnaire (WSSQ), was shown to be a reliable and valid tool to assess IWS and to detect the impact of effective interventions targeting weight-related stigma [17].
The WSSQ was first developed and validated in two American samples (n = 169) of participants with overweight/obesity (non-treatment-seeking and treatment-seeking). The resulting two main factors (“self-devaluation” and “fear of enacted stigma”) described by the WSSQ showed good reliability and validity indices as well as an adequate sensitivity to change in subjects seeking treatment for IWS reduction, as well as a good sensitivity to change and temporal stability. Good psychometric proprieties of the WSSQ—such as convergent validity, reliability, and predictive values for psychological variables—were confirmed in a later study [13] Moreover, the scale showed associations with clinical and/or subclinical conditions such as anxiety, depression, Quality of Life (QoL) and self-esteem [17].
The WSSQ was adapted in German [19], Arabic [35], and French [36] language. The German version [19] was validated in a sample of 94 adult outpatients with severe obesity demonstrating good psychometrical proprieties. Hain and colleagues also showed the impact of feelings of guilt (related to body image), BMI (≥ 50), and dissociative symptoms in the prediction of IWS [19]. The Arabic version [35] was validated on a sample of 170 Iranian women with overweight/obesity and showed good validity and internal consistency indices. Moreover, the authors evaluated the association between IWS, QoL, and psychological distress. Results confirmed the negative impact of IWS on both psychological distress and QoL, suggesting that IWS might represent a barrier for subjects with obesity to undertake health-promoting attitudes and behaviors. However, neither for the German study nor for the Arabic validation of the WSSQ any factor analysis (exploratory or confirmatory) was conducted to assess the factorial structure of the questionnaire. Instead, a confirmatory factor analysis (CFA) approach was employed to validate the French version of WSSQ [36]. The authors tested the factorial structure of the questionnaire in a sample of 156 adolescents with overweight/obesity, and findings revealed a good of model fit indices and reliability. Maïano and colleagues also assessed the correlation (convergent validity) between IWS, self‑esteem, anxiety, depression, fear of appearance evaluation, and tendency to eating‑related pathology. Results revealed an association between IWS and all the above psychological constructs. In addition, the authors tested the measurement invariance of the tool across gender using a MIMIC-based (Multiple Indicators Multiple Causes) approach, which revealed an influence of participant gender on WSSQ response. Notably, in line with the literature, none of the above validation studies showed associations between IWS and BMI, suggesting that IWS is complex phenomenon that goes beyond the mere individuals’ BMI [18]. Given that the IWS is a well-known risk-factor among those negatively influencing the individuals’ psychological health [37] in individuals with overweight and obesity, it is important to assess it both in the clinical and research fields.
Since there is no standardized validated version of the WSSQ available for the Italian population, the present study aimed to explore the factorial structure of the Italian version of the WSSQ (Study1), and to assess its structural validity, internal consistency, test–retest reliability, and measurement invariance across main socio-demographics characteristics (Study2).
Study1
Methods
Translation and cross-cultural adaptation
The WSSQ was independently translated by two Italian experts in the field and back-translated into English by an independent translator—to guarantee conceptual equivalency [38]. The questionnaire was also administered to 10 subjects with overweight/obesity—who did not enter the analysis—to assess whether the items were understandable by the target population. No adjustments were needed.
Participants and procedure
According to the most commons rule-of-thumb for Exploratory Factor Analysis (EFA) [39], the sample was composed by 150 adult inpatients [48 males (32%) and 102 females (68%)] with overweight/obesity—aged from 18 to 78 years (mean = 50.34, SD = 14.457). Participants were recruited from the IRCCS Istituto Auxologico Italiano, San Giuseppe Hospital, Verbania (Italy), during their first week of a 1-month hospital-based program for weight reduction and rehabilitation. Inclusion criteria were: (A) being a native Italian speaker; (B) being over 18 years; (C) signing written and informed consent. Exclusion criteria were: (D) illiteracy; (E) inability to complete the assessment due to vision and/or cognitive impairments. All participants completed a self-report demographic and anthropometric measures form and the Italian WSSQ. Sample descriptive statistics are displayed in Table 1.
Measures
Demographic and anthropometric measures
Participants were asked for demographic information (Table 1) including gender, civil status, educational level, work status, and the occurrence of previous hospitalization(s) for obesity and weight reduction, as well as to provide anthropometric measures, such as age, height, and weight (used to calculate their BMI).
Weight Self‑Stigma Questionnaire
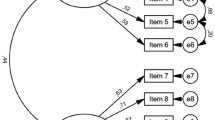
Participants completed the Italian version of the Weight Self-Stigma Questionnaire (WSSQ) [17]. It consists of 12 items rated on a five-point Likert scale (from 1 = strongly disagree to 5 = strongly agree) and provides scores in two domains (self-devaluation and fear of enacted domains). The first six items measure self-devaluation (Self-D), which is the continuous tendency to self-depreciating by attributing negative stigmatizing characteristics to his/her own [17]. An example of a representative item is: “I became overweight because I’m a weak person” (item#4) and “I don’t have enough self-control to maintain a healthy weight” (item#6). The following six items measure the fear of enacted stigma (FES), which refers to self-stigmatized thoughts [17, 40]. Representative items are: “People discriminate against me because I’ve had weight problems” (item#8) and “Others will think I lack self-control because of my weight problems” (item#10). Coefficient alphas of the original WSSQ were: Self-D = 0.812; FES = 0.869; total score = 0.878.
Statistical analysis
Statistical analyses were performed with the R statistical software [41] with the following packages: psych [42] and MplusAutomation [43].
Item analysis was performed to check normality. Due to acceptable deviation from normality, Maximum Likelihood estimator (ML) has been used to perform the EFA [39, 44,45,46], with a Direct Oblimin rotation due to an expected correlation between factors. Factors were retained according to the 95th percentile of Parallel Analysis (PA) with 10,000 random correlation matrices—used to compute random data eigenvalues. The size of these random data eigenvalues was compared with the ones from the original observations. The best factor solution was determined by the number of eigenvalues that exceeded the corresponding values from the random dataset [47,48,49]. The factorability of the correlation matrix was evaluated with Bartlett’s Test of Sphericity and with Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy. For the EFA to be considered appropriate, the above tests had to show significant results (p < 0.05) and values higher than 0.7–—respectively [39]. Lastly, Cronbach’s alpha was computed as measure of internal consistency with values higher than 0.7 deemed acceptable [39].
Results
Exploratory factor analysis of WSSQ
Item analysis reveals a univariate almost-normal distribution of all the indicators (Table 2). Absolute skewness ranged from |0.007| for item#11 to |1.033| for item#2: meansk = 0.03; SDsk = 0.52. Absolute kurtosis ranged from |0.025| for item#2 to |1.313| for item#11: meank = − 0.96; SDk = 0.38.
Sample correlation matrix reveals two eigenvalues higher than 1 (i.e., I = 4.659; II = 1.945; III = 0.956) that were compared with PA’s random data eigenvalues (i.e., I = 1.622; II = 1.443; III = 1.326) allowing the extraction of two factors that explained the 55.04% of the overall variance. The first factor accounted for 38.83% of the variance, while the second one explained 16.21% of the variance. In line with the Kaiser–Meyer–Olkin’s test [KMO = 0.797], the Bartlett’s Test of Sphericity reached statistical significance: [χ2 (66) = 733.4, p < 0.001]—thus supporting the factorability of the correlation matrix.
As depicted in Table 2, the first six items—reflecting the original Self-D factor—loaded significantly on the first factor (p < 0.001): meanloadings = 0.635; SDloadings = 0.161, ranging from 0.389 (item#1) to 0.784 (item#3). However, item#2 and item#4 showed significant cross-loadings (respectively: λ = − 0.241; λ = − 0.156), albeit lower than 0.3. The last six items—reproducing the original FES—loaded significantly on the second factor (p < 0.001): meanloadings = 0.631; SDloadings = 0.07; ranging from 0.556 (item#10) to 0.746 (item#9). Still, four items (item#7, item#9, item#10 and item#11) showed significant cross-loadings (respectively: λ = 0.276; λ = − 0.170; λ = 0.233; λ = 0.213), although lower than 0.3. Furthermore, EFA revealed a significant correlation between the two factors: r = 0.444; p < 0.001. Cronbach’s alpha exhibited an acceptable internal consistency: Self-D: α = 0.815; FES: α = 0.827; total score: α = 0.852.
Study2
Methods
Participants and procedure
According to (A) Monte Carlo study simulation [50] and (B) the ratio of subjects-to-variables rule-of-thumb [45, 46], the sample was composed by 446 adult inpatients with overweight and obesity (BMI ≥ 35) [170 males (38.1%) and 276 females (61.9%)] aged from 18 to 81 years (mean = 51.69, SD = 13.09). Patients were enrolled at the IRCCS Istituto Auxologico Italiano, San Giuseppe Hospital, Verbania (Italy) and tested within 3 days from their admission into the 1-month hospital-based program for weight reduction and rehabilitation. Inclusion/exclusion criteria described in Study1 were applied. Complete descriptive statistics are presented in Table 1. Participants completed: (A) the demographic and anthropometric measures form—described in Study1; (B) the WSSQ; (C) the Weight Bias Internalization Scale (WBIS); (D) the Body Uneasiness Test (BUT); and (E) the Center for Epidemiologic Studies Depression Scale (CES-D). To assess test–retest reliability, a random subsample of 40 subjects was also retested at discharge from the hospital (after ± 28 days)—to ensure no memory effect [51]. During the hospitalization period, none of the patients received psychological interventions focused on the reduction of IWS.
Measures
Weight Bias Internalization Scale (WBIS)
The WBIS [18, 52] is an 11-item—single-factor—self-report scale. Developed for people with overweight/obesity, the WBIS measures the agreement with self-directed negative statements about negative weight-related stereotypes. Higher scores are indicative of a higher weight-related bias own perception. In this study, the WBIS Cronbach’s alpha was 0.840.
Body Uneasiness Test (BUT)
The BUT [53] is a 34-item self-report questionnaire evaluating body uneasiness and concerns for physical appearance. Not designed for a specific target population, the BUT comprises a Global Severity Index (GSI) and 5 subscales: (I) fear regarding the body’s weight (Weight Phobia: WP), (II) over-concern related to physical appearance (Body Image Concerns: BICons), (III) body image-related avoidance behavior (Avoidance: A), (IV) compulsive checking of physical appearance (Compulsive Self-Monitoring: CSM), (V) estrangement feelings toward his/her own body (Depersonalization: Dep). In the present study, the BUT Cronbach’s alphas were: GSI = 0.960; WP = 0.849; BICons = 0.911; A = 0.873; CSM = 0.723; Dep = 0.867.
Center for Epidemiologic Studies Depression Scale (CES-D)
The CES-D [54, 55] is a self-report scale that assesses psychological and behavioral symptoms of depression. Developed for the general population, the CES-D is composed of 20-item loading on a single factor. Higher scores reflect greater depressive symptomatology. In the current study, the CES-D Cronbach’s alpha was 0.903.
Statistical analysis
All statistical analyses were carried out with R statistical software [41] and the following packages: psych [42], MplusAutomation [43], lme4 [56], and irr [57].
Item analysis was performed to check normality. Due to a non-perfect normal distribution, Robust Maximum Likelihood estimator (MLR) was used to confirm the factorial structure of the Italian WSSQ. The MLR is a ‘robust’ variant of Maximum likelihood—which has many advantages over other estimators; i.e., computational efficiency [58]—providing robust standard errors and mean-adjusted χ2 statistics that are robust to non-normality and the violation of independence-of-observation assumption [45, 46, 58,59,60,61]. Model fit was tested using the χ2 statistic and the goodness-of-fit indices [45, 46, 62]: (A) the Root-Mean Square Error of Approximation (RMSEA) [63], (B) the Comparative Fit Index (CFI) [64] and (C) the Standard Root Mean square Residual (SRMR) [65]. A non-significant χ2 was desirable as indicating a better model fit [45, 46, 62]. The RMSEA expresses fit per degrees of freedom of the model, and values lower than 0.08 suggest an acceptable model fit [66, 67]. The CFI designates the amount of variance and covariance accounted by the model compared with a baseline, with values higher than 0.90 considered adequate [66, 67]. The SRMR represents the average discrepancy between the correlations observed in the input matrix and those predicted by the model [45, 65], and values lower than 0.08 are considered good [46, 66].
Multi-group CFAs were performed to test MI across (1) gender (male vs. female), (2) BMI (Class II obesity class vs. Class III obesity), (3) age (younger vs. older: grouped by the median split technique), and (4) previous hospitalization for obesity (occurrence vs. non-occurrence). MI entailed a series of hierarchical (nested) CFAs in which models parameters were consecutively constraint to be equals (invariants) across groups in a logically ordered and increasingly restrictive mode [45, 46, 67,68,69,70]. Nested model comparisons were conducted using (I) the Log-likelihood rescaled difference test (− 2ΔLL), (II) the test differences in absolute goodness-of-fit indices: CFI (ΔCFI > 0.01), RMSEA (ΔRMSEA > 0.015), and SRMR (ΔSRMR > 0.03) [71, 72]. The first step was to test the goodness-of-fit in the two groups, separately. The second step was to test the equivalence of the models (configural invariance). The third step (metric invariance) constrained the factor loadings to be equal across groups. The fourth step (scalar invariance) forced the equivalence of factor loadings and item’s intercepts across groups [45, 46, 67,68,69,70].
Moreover, items must provide information regarding the respondents: in other words, the item should be able to discriminate subjects with or without IWS. Therefore, following recommended guidelines [73], a series of independent sample t-tests were computed, and the Cohen’s d coefficient [74] was calculated to determine item discriminating power (IDP). These statistics refer to the magnitude to which the item discriminates the respondent’s level of the measured trait (low vs. high). A highly discriminating item divides clearly the respondents (d ≥ 0.80), a moderate discriminant item reveals regions of ambiguity (0.21 ≤ d ≤ 0.79) and a poorly discriminating item shows very small magnitude (d ≤ 0.20).
Moreover, since none of the participants received a psychological intervention to reduce IWS, temporal stability was assessed using a mixed-model repeated measure regression analysis accounting for random variability within individuals: a non-significant p value was expected.
Test–retest reliability was estimated using the two-way mixed intraclass correlation coefficient (ICCconsistency) [39, 51, 75,76,77]
Pearson’s correlation was also computed to assess the convergent validity between internalized self-stigma (WSSQ), weight bias (WBIS), depressive symptomatology (CES-D), body uneasiness (BUT), and the individuals’ BMI.
Results
Model’s fit and psychometric proprieties: structural validity
Item analysis revealed a non-perfect univariate normal distribution of some indicators (Table 3). Absolute skewness ranged from |0.004| for item5 to |1.410| for item12: meansk = 0.29; SDsk = 0.61. Absolute kurtosis ranged from |0.017| for item9 to |1.343| for item11: meank = -0.74; SDk = 0.74.
Results from the CFA suggested a non-adequate two-related-factors solution for the Italian WSSQ: the χ2 was statistically significant [SBχ2 (53) = 231.219; p < 0.001] and both the RMSEA and the CFI did not meet the recommended threshold suggesting a non-ideal fit: RMSEA = 0.087; CFI = 0.887, despite an acceptable SRMR (0.066).
Exploration of modification indexes [45, 46, 49, 69] also revealed that the model could be improved by correlating residuals of item#10 and item#11 (Δχ2 = 41.345). More in detail, a deep examination of these items suggested a possible non-independence among these two indicators. After correlating these items’ residuals [45, 46, 49, 69], the model provided a better fit to the data (ritem#10-#11 = 0.396). Despite the Chi-square resulted statistically significant [SBχ2 (52) = 189.874; p < 0.001], the remaining fit indices overcame the threshold for good model fit: RMSEA = 0.077 [90% CI: 0.065–0.089], CFI = 0.913 and SRMR = 0.066.
As reported in Table 3, each item loaded significantly on its associated factor: meanloadings = 0.64; SDloadings = 0.15; ranging from 0.338 (item#1) to 0.856 (item#4). In addition, a moderate correlation between the two factors was found: r = 0.513, p < 0.001. Lastly, item’s explained variance (R2) ranged between 0.114 (item#1) and 0.733 (item#4) with a meanloadings of 0.43 and a SDloadings equal to 0.18.
Measurement invariance
Configural invariance. A configural invariance model was specified: the same two-factor model was estimated simultaneously within each group. A good model fit was found for: (A) gender, (B) BMI status, (C) age, and (D) previous hospitalization for obesity (Table 4). Achieved configural invariance suggests that the factor structure was similar across groups.
Metric invariance. Equality of item factor loadings across groups was examined in a metric invariance model: all factor loadings were constrained to be equal across conditions. The metric invariance model well fit the data (Table 4). Compared to the configural model, no significant decrease in fit indices was found for (A) gender [− 2ΔLL (10) = 12.604; p = 0.247; ΔRMSEA = 0.003; ΔCFI = 0.002; ΔSRMR = -0.005], (B) BMI [− 2ΔLL (10) = 13.530; p = 0.196; ΔRMSEA = 0.002; ΔCFI = 0.008; ΔSRMR = -0.006] and (D) previous hospitalization for obesity [− 2ΔLL (10) = 7.587; p = 0.669; ΔRMSEA = 0.004; ΔCFI = -0.001; ΔSRMR = -0.003]. Inversely, a significant loss of fit compared to the configural model was found for (C) age in the Log-likelihood rescaled difference test [− 2ΔLL (10) = 21.411; p = 0.018]. Achieved metric invariance indicated that the items were equivalently related to the latent factor in each group.
Scalar invariance. Equality of item intercepts was examined in a strict invariance model: all factor loadings and all item intercepts were constrained to be equal across groups. The model well fitted the data for each condition except for gender (CFI = 0.898). No decrease in fit indices compared to the metric invariance model was found for (B) BMI [− 2ΔLL (10) = 17.264; p = 0.069; ΔRMSEA = 0.001; ΔCFI = 0.005; ΔSRMR = − 0.002] and (D) previous hospitalization for obesity [− 2ΔLL (10) = 9.432; p = 0.492; ΔRMSEA = 0.002; ΔCFI = 0.001; ΔSRMR = − 0.002]. Conversely, a significant model decrease in fit was observed for (A) gender [− 2ΔLL (10) = 37.873; p < 0.001; ΔRMSEA = − 0.004; ΔCFI = 0.017; ΔSRMR = − 0.002]. As scalar invariance was achieved, it indicated that groups had the same expected item response at the same absolute level of the trait.
Psychometric properties
The analysis of IDP (reported in Table 3) revealed that each of the 12 items well discriminates between subjects without IWS from individuals with IWS—with a high magnitude (d) in all cases. More in detail, the absolute values of the discrimination parameter (t-test: ti) ranged from |8.57| (item#2) to |25.31| (item#7), with an associated effect size that ranged respectively from 1.00 (item#2) to 2.90 (item#7)—meant = -15.71; SDt = 5.21; meand = 1.82; SDd = 0.60. With no exception, all the discriminating values suggest a strong relationship between each of the WSSQ item and the underlying IWS construct.
Temporal stability and test–retest reliability provided good results: Self-D, ICC(T1,T2) = 0.883 (95% CI: from 0.779 to 0.938), p < 0.001; FES: ICC(T1,T2) = 0.852 (95% CI: from 0.721 to 0.922), p < 0.001; Total score: ICC(T1,T2) = 0.886 (95% CI: from 0.785 to 0.940), p < 0.001).
Moderate-to-large bivariate correlations indicated that both WSSQ factors and the WSSQ total score were positively and significantly associated with WBIS, CES-D, and BUT. A significant small correlation was also found between BMI and FES factor, whereas—in line with previous literature—no significant correlation was found between WSSQ and BMI for the Self-D subscale and the total score (Table 5).
Discussion
The alarming rates of obesity have brought widespread attention to the medical consequences of this public health problem [12, 15, 16, 32, 78, 79]. Stigmatization and discrimination are still experienced in different conditions [80,81,82], and in individuals with overweight/obesity these biases might lead to serious health consequences [17, 18, 26,27,28,29]. Interventions aimed to specifically address the IWS are urgently required, and more research is needed to support and improve them [23].
Across studies, languages and cultures [17, 19, 35, 36], the WSSQ was shown to be a valid and reliable tool measuring weight self-stigma [17].
The present study is the first aimed to explore and assess the psychometrical proprieties of the Italian version of the WSSQ in a sample of adult inpatients with overweight/obese. In addition, it is unique in examining the WSSQ measurement invariance across several conditions.
In line with previous researches [83, 84], the first study was aimed to explore the structure of the WSSQ. In line with its original validation study [17], the exploration of the factorial structure of the WSSQ (Study1) indicated the presence of two factors (“Self-devaluation” and “Fear of enhanced stigma”) accounting for 55.04% of variance Moreover, items’ significant cross-loadings were lower than the threshold of 0.3—confirming this factorial solution.
In Study2, the two-factor structure of the WSSQ was further confirmed: results of the CFA revealed that—after correlating residuals for item#10 and item#11—the questionnaire shows a good fit to the data. Moreover, the two-factor solution of the WSSQ—Italian version was in line with previous studies validating the tool in other languages (English [17], German [19], Arabic [35], and French [36]). Each subscale of the Italian WSSQ showed reliability indices over the cutoff value for adequate internal consistency [39]—both in Study1 and Study2—in particular, the Self-D’s alpha was higher than those reported for the German and the Arabic versions of the WSSQ (0.74 and 0.75, respectively), but lower than in its original validation study (0.87). The FES’s alpha showed an almost perfect overlap with the German version (0.83) and it was higher than those of the original and the Arabic versions of the tool (0.81 and 0.78, respectively). The Italian WSSQ also demonstrates good test–retest reliability, with slightly different values from the work of Lillis and colleagues [17].
Moreover, in line with the existing literature, positive and statistically significant relationships were found between both factors of the WSSQ and the convergent measure of weight-related stigma (WBIS), the BUT-body image concerns subscales, and depressive symptomatology (CES-D). Although a non-significant association between Self-D and BMI was detected in the present as in previous research (i.e., German, Arabic, and French versions), it was not in its the WSSQ original validation study [17]. In addition, the correlation between FES and BMI was consistent with the study of Lillis and colleagues [17], but in contrast with other validation studies [19, 35, 36]. These results suggest a potential cross-cultural influence in the relationship between BMI and self-stigma interpretation.
To our knowledge, this is the first study examining the WSSQ measurement invariance across gender, BMI, age, and the occurrence of previous hospitalization(s) for obesity. Age was shown to affect item responses; indeed, only configural invariance was achieved. These results suggest that the factor structure of the WSSQ is the same for both age group, but also that they interpret the items differently and at a different absolute level of the trait. In line with the results of Maïano and colleagues [36], measurement invariance suggested a possible effect of gender on the WSSQ responses: only metric invariance was held, indicating that the same latent factors were measured in each group, but there was a non-equivalence of the trait’s level measured (items intercept).The WSSQ also demonstrated scalar invariance across BMI and the occurrence of previous hospitalization(s) for obesity, indicating the equivalence of the factor structure model, item factor loadings, and item intercepts across these groups. These results showed that—within these two variables—the observed differences in item means (between groups) are due to factor mean differences only.
Among, the limitations of the study we consider the self-report nature of selected measures—whose answers might have been influenced by social desirability and items’ comprehensibility. Moreover, a convenience sample of adult inpatients with overweight and obesity was recruited for this study—and future research should be conducted on outpatients or children/adolescents to confirm the reliability of this findings. Despite a WSSQ post-treatment measure, the small sample size (n = 40) prevented from assessing longitudinal MI—the collection of more data at the end of hospitalization could solve this issue.
Despite these limits, the present study is the first consistently increasing knowledge in the field since—compared to previous WSSQ validation studies—the invariance of the questionnaire was tested across several conditions, and the Italian WSSQ can, therefore, be considered a valid and reliable instrument for assessing weight self-stigma in adults with overweight and obesity.
Regarding the implications for the clinical and research field, the WSSQ represents a useful tool that—given its brief and agile administration—it is suitable both for hospital-based [85,86,87] and at-distance technology-based interventions [88,89,90] aimed at monitoring and promoting the individuals psychological health over time [91,92,93].
Conclusion
The Italian WSSQ is a solid tool for the measurement of IWS and can extend the research concerning stigma in obese people. This is of great importance for improving treatment outcomes in clinical practice, as individuals with high IWS are at greater risk for psychosocial impairments [17, 19, 35, 36, 94] and failure to weight loss/maintenance [23, 95]. The WSSQ can be used to properly identifying those subjects who would benefit from specialized interventions aimed at reducing IWG, also allowing the evaluation of the impact of such treatments.
What is already known on this subject?
Weight stigma is a widespread complex problem among individuals with overweight and obesity.
The Weight Self-Stigma Questionnaire (WSSQ), is a solid, valid and reliable tool for the measurement of weight-related bias in overweight and obese people.
The WSSQ was successfully translated and/or validated in several languages such as English, German Arabic, and French.
What does this study add?
The present study aimed to validate the Italian version of the WSSQ in a sample of inpatients with overweight and obesity.
This study for the first time aimed to test—psychometric properties of the WSSQ such as measurement invariance across gender, body mass index (BMI), age, and occurrence of previous hospitalization(s) for obesity.
The factorial structure of the WSSQ was successfully replicated across two independent studies (Study1 and Study2).
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gutierrez-Fisac JL, Angel Royo-Bordonada M, Rodriguez-Artalejo F (2006) Health-risks associated with Western diet and sedentariness: the obesity epidemia. Gac Sanit 20(Suppl 1):48–54
WHO (2006) Obesity and Overweight. www.who.int/mediacentre/factsheets/fs311/en/index.html.
Finkelstein EA, Ruhm CJ, Kosa KM (2005) Economic causes and consequences of obesity. Annu Rev Public Health 26:239–257. https://doi.org/10.1146/annurev.publhealth.26.021304.144628
Ogden CL, Carroll MD, Flegal KM (2014) Prevalence of obesity in the United States. JAMA 312(2):189–190. https://doi.org/10.1001/jama.2014.6228
Ogden CL, Carroll MD, Kit BK, Flegal KM (2014) Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 311(8):806–814. https://doi.org/10.1001/jama.2014.732
Bowman K, Delgado J, Henley WE, Masoli JA, Kos K, Brayne C, Thokala P, Lafortune L, Kuchel GA, Ble A, Melzer D (2017) Obesity in older people with and without conditions associated with weight loss: follow-up of 955,000 primary care patients. J Gerontol Ser A: Biomed Sci Med Sci 72(2):203–209
Batsis JA, Gill LE, Masutani R, Adachi-Mejia AM, Blunt HB, Bagley PJ, Lopez-Jimenez F, Bartels SJ (2017) Weight loss interventions in older adults with obesity: a systematic review of randomized controlled trials since 2005. J Am Geriatr Soc 65(2):257–268
Balestroni G, Panzeri A, Omarini P, Cerutti P, Sacco D, Giordano A, Pistono M, Komici K, Rossi Ferrario S (2020) Psychophysical health of elderly inpatients in cardiac rehabilitation: a retrospective cohort study. Eur J Phys Rehabil Med 56(2):197–205. https://doi.org/10.23736/s1973-9087.20.05970-5
Panzeri A, Komici K, Cerutti P, Sacco D, Pistono M, Ferrario SR (2021) Gender differences and long-term outcome of over 75 elderlies in cardiac rehabilitation: Highlighting the role of psychological and physical factors through a secondary analysis of a cohort study. Eur J Phys Rehabil Med 57(2):288–297. https://doi.org/10.23736/s1973-9087.21.06484-4
Andreyeva T, Puhl RM, Brownell KD (2008) Changes in perceived weight discrimination among Americans, 1995–1996 through 2004–2006. Obesity 16(5):1129–1134
Latner JD, Stunkard AJ (2003) Getting worse: the stigmatization of obese children. Obesity 11(3):452–456
Puhl RM, Heuer CA (2009) The stigma of obesity: a review and update. Obesity 17(5):941–964
Hübner C, Schmidt R, Selle J, Köhler H, Müller A, de Zwaan M, Hilbert A (2016) Comparing self-report measures of internalized weight stigma: the weight self-stigma questionnaire versus the weight bias internalization scale. PLoS ONE 11(10):e0165566
Faccio E, Belloni E, Cipolletta S, Iudici A, Castiglioni M, Mannarini S (2019) The power of weight and the weight of power in adolescence: a comparison between young and adult women. J Fam Stud 25(1):46–60. https://doi.org/10.1080/13229400.2016.1187660
Major B, O’brien LT (2005) The social psychology of stigma. Annu Rev Psychol 56:393–421
Alberga AS, Russell-Mayhew S, von Ranson KM, McLaren L (2016) Weight bias: a call to action. J Eat Disord 4:34. https://doi.org/10.1186/s40337-016-0112-4
Lillis J, Luoma JB, Levin ME, Hayes SC (2010) Measuring weight self-stigma: the Weight Self-Stigma Questionnaire. Obesity 18(5):971–976
Durso LE, Latner JD (2008) Understanding self-directed stigma: development of the weight bias internalization scale. Obesity 16(S2):S80–S86
Hain B, Langer L, Hünnemeyer K, Rudofsky G, Zech U, Wild B (2015) Translation and validation of the German version of the Weight Self-Stigma Questionnaire (WSSQ). Obes Surg 25(4):750–753
Sikorski C, Luppa M, Braehler E, Koenig HH, Riedel-Heller SG (2012) Obese children, adults and senior citizens in the eyes of the general public: results of a representative study on stigma and causation of obesity. PLoS ONE 7:e46924
Puhl RM, King KM (2013) Weight discrimination and bullying. Best Pract Res Clin Endocrinol Metab 27(2):117–127
Mensinger JL, Meadows A (2017) Internalized weight stigma mediates and moderates physical activity outcomes during a healthy living program for women with high body mass index. Psychol Sport Exerc. https://doi.org/10.1016/j.psychsport.2017.01.010
Lent MR, Napolitano MA, Wood GC, Argyropoulos G, Gerhard GS, Hayes S et al (2014) Internalized weight bias in weight-loss surgery patients: psychosocial correlates and weight loss outcomes. Obes Surg 24(12):2195
Bray GA (2004) Medical consequences of obesity. J Clin Endocrinol Metab 89(6):2583–2589. https://doi.org/10.1210/jc.2004-0535
Must A, Strauss RS (1999) Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord: J Int Assoc Study Obes 23(Suppl 2):S2–S11
Durso LE, Latner JD, White MA, Masheb RM, Blomquist KK, Morgan PT, Grilo CM (2012) Internalized weight bias in obese patients with binge eating disorder: associations with eating disturbances and psychological functioning. Int J Eat Disord 45(3):423–427
Hilbert A, Braehler E, Haeuser W, Zenger M (2014) Weight bias internalization, core self-evaluation, and health in overweight and obese persons. Obesity (Silver Spring) 22(1):79–85. https://doi.org/10.1002/oby.20561
Roberto CA, Sysko R, Bush J, Pearl R, Puhl RM, Schvey NA, Dovidio JF (2012) Clinical correlates of the weight bias internalization scale in a sample of obese adolescents seeking bariatric surgery. Obesity 20(3):533–539
Puhl RM, Moss-Racusin CA, Schwartz MB (2007) Internalization of weight bias: implications for binge eating and emotional well-being. Obesity 15(1):19–23
Pietrabissa G, Rossi A, Borrello M, Manzoni GM, Mannarini S, Castelnuovo G, Molinari E (2020) Development and validation of a self-determination theory-based measure of motivation to exercise and diet in children. Front Psychol. https://doi.org/10.3389/fpsyg.2020.01299
Pietrabissa G, Sorgente A, Rossi A, Simpson S, Riva G, Manzoni GM, Prochaska JO, Prochaska JM, Cattivelli R, Castelnuovo G (2017) Stages of change in obesity and weight management: factorial structure of the Italian version of the University of Rhode Island Change Assessment Scale. Eat Weight Disord 22(2):361–367. https://doi.org/10.1007/s40519-016-0289-1
Guerrini Usubini A, Cattivelli R, Giusti EM, Riboni FV, Varallo G, Pietrabissa G, Manzoni GM, Consoli S, Bastoni I, Granese V, Volpi C, Villa V, Caretti A, Bottacchi M, Castelnuovo G, Molinari E (2021) The ACTyourCHANGE study protocol: promoting a healthy lifestyle in patients with obesity with Acceptance and Commitment Therapy—a randomized controlled trial. Trials. https://doi.org/10.1186/s13063-021-05191-y
Cattivelli R, Usubini AG, Manzoni GM, Riboni FV, Pietrabissa G, Musetti A, Franceschini C, Varallo G, Spatola CAM, Giusti E, Castelnuovo G, Molinari E (2021) ACTonfood. Acceptance and commitment therapy-based group treatment compared to cognitive behavioral therapy-based group treatment for weight loss maintenance: an individually randomized group treatment trial. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph18189558
Mannarini S, Boffo M, Balottin L (2013) Beliefs about the patient’s role in the psychotherapeutic relationship: a latent trait perspective. TPM - Test Psychometr Methodol Appl Psychol 20(3):277–294. https://doi.org/10.4473/tpm20.3.6
Farhangi MA, Emam-Alizadeh M, Hamedi F, Jahangiry L (2016) Weight self-stigma and its association with quality of life and psychological distress among overweight and obese women. Eat Weight Disord. https://doi.org/10.1007/s40519-016-0288-2
Maiano C, Aime A, Lepage G, Morin AJ (2017) Psychometric properties of the Weight Self-Stigma Questionnaire (WSSQ) among a sample of overweight/obese French-speaking adolescents. Eat Weight Disord. https://doi.org/10.1007/s40519-017-0382-0
Panzeri A, Bertamini M, Butter S, Levita L, Gibson-Miller J, Vidotto G, Bentall RP, Bennett KM (2021) Factors impacting resilience as a result of exposure to COVID-19: The ecological resilience model. PLoS ONE. https://doi.org/10.1371/journal.pone.0256041
Beaton DE, Bombardier C, Guillemin F, Ferraz MB (2000) Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976) 25(24):3186–3191
Tabachnick BG, Fidell LS (2014) Using multivariate statistics, 6th edn. Pearson ed, Harlow
Link BG, Phelan JC (2001) Conceptualizing stigma. Ann Rev Sociol 27(1):363–385
R Core Team (2014) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria
Revelle W (2018) psych: procedures for personality and psychological research, 1.8.3. Evanston, Illinois
Hallquist MN, Wiley JF (2018) MplusAutomation: an R package for facilitating large-scale latent variable analyses in Mplus. Struct Equ Modeling: Multidiscip J 25(4):621–638. https://doi.org/10.1080/10705511.2017.1402334
Curran PJ, West SG, Finch J (1996) The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychol Methods 1:16–29. https://doi.org/10.1037/1082-989X.1.1.16
Brown TA (2015) Confirmatory factor analysis for applied research, 2nd edn. The Guilford Press, New York
Hoyle RH (2012) Handbook of strucural equation modeling. The Guilford Press, New York
Horn JL (1965) A rationale and test for the number of factors in factor analysis. Psychometrika 30:179–185
Hayton JC, Allen DG, Scarpello V (2004) Factor retention decisions in exploratory factor analysis: a tutorial on parallel analysis. Organ Res Methods 7:191–205
Muthén LK, Muthén BO (1998–2012) Mplus user’s guide. Seventh Edition edn., Los Angeles
Wolf EJ, Harrington KM, Clark SL, Miller MW (2013) Sample size requirements for structural equation models: an evaluation of power, bias, and solution propriety. Educ Psychol Meas 76(6):913–934. https://doi.org/10.1177/0013164413495237
Aday LA, Cornelius LJ (2006) Designing and conducting health surveys: a comprehensive guide. Jossey-Bass, San Francisco
Innamorati M, Imperatori C, Lamis DA, Contardi A, Castelnuovo G, Tamburello S, Manzoni GM, Fabbricatore M (2016) Weight Bias internalization scale discriminates obese and overweight patients with different severity levels of depression: the Italian Version of The WBIS. Curr Psychol 36:242–251. https://doi.org/10.1007/s12144-016-9406-6
Cuzzolaro M, Vetrone G, Marano G, Garfinkel PE (2006) The Body Uneasiness Test (BUT): development and validation of a new body image assessment scale. Eat Weight Disord 11(1):1–13
Radloff LS (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1:385–401
Fava GA (1983) Assessing depressive symptoms across cultures: Italian validation of the CES-D self-rating scale. J Clin Psychol 39(2):249–251
Bates D, Maechler M, Bolker B, Walker S (2015) Fitting linear mixed-effects models using lme4. J Stat Softw 67(1):1–48. https://doi.org/10.18637/jss.v067.i01
Gamer M, Lemon J, Fellows I, Singh P (2019) irr: Various Coefficients of Interrater Reliability and Agreement. 0.84.1
Muthén B, Asparouhov T (2011) Beyond multilevel regression modeling: multilevel analysis in a general latent variable framework. In: Hox J, Roberts JK (eds) Handbook of advanced multilevel analysis. Taylor & Francis, New York, pp 15–40
Yuan KH, Bentler PM (2000) Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociol Methodol 30(1):165–200
Pietrabissa G, Rossi A, Simpson S, Tagliagambe A, Bertuzzi V, Volpi C, Fava G, Manzoni GM, Gravina G, Castelnuovo G (2020) Evaluation of the reliability and validity of the Italian version of the schema mode inventory for eating disorders: short form for adults with dysfunctional eating behaviors. Eat Weight Disord 25(3):553–565. https://doi.org/10.1007/s40519-019-00644-5
Simpson S, Pietrabissa G, Rossi A, Seychell T, Manzoni GM, Munro C, Nesci JB, Castelnuovo G (2018) Factorial structure and preliminary validation of the schema mode inventory for eating disorders (SMI-ED). Front Psychol 9:600. https://doi.org/10.3389/fpsyg.2018.00600
Barrett P (2007) Structural equation modelling: adjudging model fit. Personality Individ Differ 42(5):815–824. https://doi.org/10.1016/j.paid.2006.09.018
Steiger JH, Lind JC (1980) Statistically-based test for the number of common factors. Paper presented at the Annual Meeting of the Psychometric Society, Iowa City, IA
Bentler PM (1990) Comparative fit indexes in structural models. Psychol Bull 107(2):238–246
Bentler PM (1995) EQS structural equation program manual. In: Multivariate Software. Encino, CA
Hu LT, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model 6:1–55
van de Schoot R, Lugtig P, Hox J (2012) A checklist for testing measurement invariance. Eur J Dev Psychol 9(4):486–492. https://doi.org/10.1080/17405629.2012.686740
Meredith W (1993) Measurement invariance, factor analysis and factorial invariance. Psychometrika 58:525–543
Byrne BM (2008) Testing for multigroup equivalence of a measuring instrument. A walk through the process. Psicothema 20:872–882
Millsap RE (2012) Statistical approaches to measurement invariance. Statistical Approaches to Measurement Invariance. Routledge, New York. https://doi.org/10.4324/9780203821961
Chen FF (2007) Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equ Model 14(3):464–504
Cheung GW, Rensvold RB (2002) Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Model 9:233–255. https://doi.org/10.1207/S15328007SEM0902_5
Ebel RL (1965) Measuring educational achievement. Prentice-Hall, Englewood Cliffs
Cohen J (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates
Berchtold A (2016) Test–retest: agreement or reliability? Methodol Innov 9:2059799116672875. https://doi.org/10.1177/2059799116672875
de Vet HC, Terwee CB, Knol DL, Bouter LM (2006) When to use agreement versus reliability measures. J Clin Epidemiol 59(10):1033–1039. https://doi.org/10.1016/j.jclinepi.2005.10.015
Koo TK, Li MY (2016) A Guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Manzoni GM, Rossi A, Pietrabissa G, Mannarini S, Fabbricatore M, Imperatori C, Innamorati M, Gearhardt AN, Castelnuovo G (2020) Structural validity, measurement invariance, reliability and diagnostic accuracy of the Italian version of the Yale Food Addiction Scale 2.0 in patients with severe obesity and the general population. Eat Weight Disord. https://doi.org/10.1007/s40519-020-00858-y
Cattivelli R, Castelnuovo G, Musetti A, Varallo G, Spatola CAM, Riboni FV, Usubini AG, Tosolin F, Manzoni GM, Capodaglio P, Rossi A, Pietrabissa G, Molinari E (2018) ACTonHEALTH study protocol: Promoting psychological flexibility with activity tracker and mHealth tools to foster healthful lifestyle for obesity and other chronic health conditions. Trials. https://doi.org/10.1186/s13063-018-2968-x
Mannarini S, Boffo M (2015) Anxiety, bulimia, drug and alcohol addiction, depression, and schizophrenia: what do you think about their aetiology, dangerousness, social distance, and treatment? A latent class analysis approach. Soc Psychiatry Psychiatr Epidemiol 50(1):27–37. https://doi.org/10.1007/s00127-014-0925-x
Mannarini S, Boffo M, Rossi A, Balottin L (2018) Etiological beliefs, treatments, stigmatizing attitudes toward schizophrenia. What do Italians and Israelis think? Front Psychol. https://doi.org/10.3389/fpsyg.2017.02289
Mannarini S, Rossi A, Munari C (2020) How do education and experience with mental illness interact with causal beliefs, eligible treatments and stigmatising attitudes towards schizophrenia? A comparison between mental health professionals, psychology students, relatives and patients. BMC Psychiatry 20(1):167. https://doi.org/10.1186/s12888-020-02580-6
Panzeri A, Rossi Ferrario S, Cerutti P (2021) Psychological differences among healthcare workers of a rehabilitation institute during the COVID-19 pandemic: a two-step study. Front Psychol. https://doi.org/10.3389/fpsyg.2021.636129
Parola A, Fusco L, Marcionetti J (2022) The parental career-related behaviors questionnaire (PCB): Psychometric properties in adolescents and young adults in the Italian context. Curr Psychol. https://doi.org/10.1007/s12144-022-02764-1
Rossi Ferrario S, Panzeri A, Cerutti P, Sacco D (2021) The psychological experience and intervention in post-acute COVID-19 inpatients. Neuropsychiatr Dis Treat 17:413–422. https://doi.org/10.2147/NDT.S283558
Pearl RL, Wadden TA, Bach C, Gruber K, Leonard S, Walsh OA, Tronieri JS, Berkowitz RI (2020) Effects of a cognitive-behavioral intervention targeting weight stigma: a randomized controlled trial. J Consult Clin Psychol 88(5):470–480. https://doi.org/10.1037/ccp0000480
Verhaak AMS, Ferrand J, Puhl RM, Tishler DS, Papasavas PK, Umashanker D (2022) Experienced weight stigma, internalized weight bias, and clinical attrition in a medical weight loss patient sample. Int J Obes. https://doi.org/10.1038/s41366-022-01087-2
Panzeri A, Rossi Ferrario S (2020) Supporting rehabilitation patients with COVID-19 during the pandemic: Experiences from a technologybased psychological approach. In: CEUR Workshop Proceedings
Welzel FD, Bär J, Stein J, Löbner M, Pabst A, Luppa M, Grochtdreis T, Kersting A, Blüher M, Luck-Sikorski C, König H-H, Riedel-Heller SG (2021) Using a brief web-based 5A intervention to improve weight management in primary care: results of a cluster-randomized controlled trial. BMC Fam Pract 22(1):61. https://doi.org/10.1186/s12875-021-01404-0
Ufholz K, Bhargava D (2021) A review of telemedicine interventions for weight loss. Curr Cardiovasc Risk Rep 15(9):17. https://doi.org/10.1007/s12170-021-00680-w
Rossi Ferrario S, Panzeri A, Pistono M (2021) Psychological difficulties of LVAD patients and caregivers: a follow up over 1 year from discharge. Artif Organs. https://doi.org/10.1111/aor.14071
Pearl RL, Wadden TA, Bach C, Tronieri JS, Berkowitz RI (2020) Six-month follow-up from a randomized controlled trial of the weight BIAS program. Obesity 28(10):1878–1888. https://doi.org/10.1002/oby.22931
Wu Y-K, Berry DC (2018) Impact of weight stigma on physiological and psychological health outcomes for overweight and obese adults: a systematic review. J Adv Nurs 74(5):1030–1042. https://doi.org/10.1111/jan.13511
Latner JD, Barile JP, Durso LE, O’Brien KS (2014) Weight and health-related quality of life: the moderating role of weight discrimination and internalized weight bias. Eat Behav 15(4):586–590. https://doi.org/10.1016/j.eatbeh.2014.08.014
Pearl RL, Puhl RM, Dovidio JF (2015) Differential effects of weight bias experiences and internalization on exercise among women with overweight and obesity. J Health Psychol 20(12):1626–1632. https://doi.org/10.1177/1359105313520338
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article. Open access funding provided by Università degli Studi di Padova within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
AAR conceived the study, wrote the manuscript, and performed the analysis. GMM contributed significantly to the study design. GMM collected the data and helped to interpret the results. GP helped to write the manuscript and also contributed to the data collection and results interpretation. SM, DDP, and GC revised the manuscript critically for important intellectual content. All the authors approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Ethical approval
All the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This research was approved by the Ethics Committee of Istituto Auxologico Italiano.
Informed consent
Written informed consent was obtained from all the participants. Informed consent was obtained from all participants included in the study before accessing the survey.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised to add missing OASIS funding note.
Daniele Di Pauli: Independent researcher, Italy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rossi, A.A., Manzoni, G.M., Pietrabissa, G. et al. Weight stigma in patients with overweight and obesity: validation of the Italian Weight Self-Stigma Questionnaire (WSSQ). Eat Weight Disord 27, 2459–2472 (2022). https://doi.org/10.1007/s40519-022-01385-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-022-01385-8