Abstract
Purpose of Review
In this review, we aim to summarize the evolution of care for the solid organ transplant recipient (SOTR) with COVID-19 disease, based on the current published guidelines and our center’s experience.
Recent Findings
Oral antiviral medications and monoclonal antibodies are now used with the goal to prevent severe disease. Immunomodulating drugs in addition to antivirals have been used in the treatment of severe COVID-19.
Summary
With the ongoing pandemic and unique challenges posed by the SOTR, understanding the risk and advancing management and treatment of COVID-19 infections are imperative to the successful care of a transplant recipient. There are many ongoing clinical trials being conducted in hopes of developing novel therapeutics towards COVID-19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic is now entering its third year, treatment and prevention methods have evolved and multiplied. Numerous medications for the treatment of coronavirus disease 19 (COVID-19) have been studied, and some have received emergency use authorization (EUA) and Food and Drug Administration (FDA) approval, allowing for improved outcomes in the fight against this infection [1, 2•]. Solid organ transplant recipients (SOTRs) are at greater risk for severe COVID-19, with worse outcomes and higher mortality rates than immunocompetent patients [3]. In general, SOTRs were not specifically included in many of the large clinical trials of COVID-19 therapeutics, thus making associations in this population difficult. A majority of the evidence for the use of these novel therapeutics in SOTR comes from retrospective studies. It is crucial to perform more large-scale studies investigating COVID-19 treatment options in SOTR to improve outcomes in this population.
Prevention options for SOTR have become a priority to stop the spread of COVID-19 [4•]. With the advent of COVID-19 vaccinations in late 2020, multiple studies have attempted to evaluate their effectiveness. Demonstrating SOTRs’ inability to mount a strong antibody response to vaccination led to recommendations for a third dose [5••]. Unfortunately, breakthrough rates of COVID-19 after vaccination in SOTR are higher than in immunocompetent patients [6•]. In a large multicenter study of 18,215 fully vaccinated SOTR, breakthrough COVID-19 infections occurred in 0.23–2.52%, compared to 0.01% in the healthy vaccinated hosts [6•]. Therefore, investigations into medications as primary COVID-19 prevention are also important in SOTR, in addition to ongoing vaccination and booster studies.
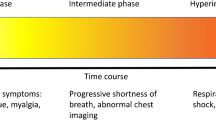
This review will highlight the evolution of clinical developments in the treatment of COVID-19, particularly in infected transplant recipients. It will include discussions on prevention techniques and treatment options. Throughout this review, when discussing severity of COVID-19 disease, definitions will be consistent with the National Institutes of Health (NIH) COVID-19 Panel guidelines on the treatment of COVID-19 [7••]. It should be noted the information is based on the medical literature available as of February 15, 2022.
COVID-19 Therapeutics
Remdesivir
Early in the pandemic, remdesivir, an adenosine nucleotide pro-drug, was seen to be effective against COVID-19 [8]. In April 2020, the National Institutes of Health (NIH) released encouraging data based on the Adaptive COVID-19 Treatment Trial 1 (ACTT-1) on remdesivir. ACTT-1 revealed that among hospitalized patients with COVID-19 who required supplemental oxygen or ventilatory support, treatment with remdesivir decreased time to recovery compared to placebo [9••]. Early treatment was also better. The greatest benefit of remdesivir occurred when patients were randomized during the first 10 days after symptom onset [9••]. Likewise, in the DisCoVeRy randomized controlled trial (RCT), patients randomized to the remdesivir arm did not benefit from the treatment if they were symptomatic for more than 7 days [10••].
Treatment duration with remdesivir was investigated in two large open-label trials. The SIMPLE Trial randomized hospitalized patients on supplemental oxygen to either 5- or 10-day courses of remdesivir and found that a 5-day course of treatment was equally beneficial to a longer course by day 15 [2•, 7••, 11•]. In the second RCT, hospitalized patients with moderate COVID-19 were randomized to 5-day remdesivir, 10-day remdesivir, or standard of care; on day 11, patients in the 5-day arm had better outcomes than those receiving standard of care [12•]. The open-label nature of this trial allowed for a variety of concomitant medications used in all treatment arms, potentially affecting interpretation. However, 5-day treatment courses of remdesivir quickly became the drug regimen of choice to treat hospitalized patients with moderate COVID-19.
Based on preliminary early data, the FDA granted emergency use authorization (EUA) for remdesivir as of May 1, 2020 [13]. Furthermore, the FDA granted full approval for remdesivir for the treatment of moderate COVID-19 in hospitalized patients in October of 2020 with final data from the ACTT-1 and SIMPLE trials as well as other RCTs, as they showed decreased length of stay and reduced oxygen need [11•, 12•, 14]. Lately, the PINETREE study evaluated the use of remdesivir in mild to moderate COVID-19 treated in the outpatient setting [15••]. This study found that 3 days of remdesivir treatment reduced the risk of hospitalization or death by 87% compared to placebo among patients with mild COVID-19 symptoms for less than 7 days.[15••] Thus, as of January 21, 2022, the FDA expanded the EUA for remdesivir to include outpatient treatment for mild to moderate COVID-19 in patients over 12 years old [16].
It should be noted that benefits of remdesivir were not definitive in many trials, and no trial revealed a mortality benefit. In the ACTT-1 trial, patients who required high-flow oxygen, mechanical ventilation, or ECMO saw no difference in time to recovery.[9••] The Solidarity Trial by the World Health Organization (WHO) randomized hospitalized patients with COVID-19 of any severity to 5 arms, including 5 or 10 days of remdesivir and placebo. Compared to their control group, remdesivir did not reduce in-hospital mortality, the need for mechanical ventilation, or duration of hospitalization [17•]. This study was open-label and may have limited the ability to assess time to recovery. It was not cited in the FDA’s approval of remdesivir. The study did not include data on time from symptom onset to enrollment [7••]. In these trials, remdesivir appears to be most effective in hospitalized patients with moderate COVID-19 on supplemental oxygen [9••, 10••, 17•].
SOTRs were not explicitly excluded from the major trials of remdesivir. While transplant medications may have represented a contraindication to treatment arms, SOTR enrollment in these trials is not explicitly stated. The ACTT-1 trial did not specify how many SOTR were included; however, it is noted that of the 1062 participants, 6.9% had some type of immune deficiency, either acquired or innate [9••]. Studies for the use of remdesivir in SOTR include retrospective case series, most of which were conducted earlier in the pandemic [18, 19]. As remdesivir was still investigational at the time, these studies had low numbers of recruited patients and utilized additional medications that likely led to confounding [20].
One early retrospective cohort of SOTR include 90 patients, but remdesivir was utilized in only two patients, one with severe disease and one with moderate disease [21]. This initial survey of SOTR with COVID-19 demonstrated that SOTR had more severe disease than immunocompetent counterparts, making comparison of treatment outcomes difficult. Evidence for use of remdesivir in SOTR in published trials is limited, with the total number of patients less than 50, and study design limited by available patients [18, 19, 22,23,24,25]. The large randomized controlled trials (RCTs) conducted on remdesivir did not include sub-group analysis of transplant recipients or, in some cases such as the Solidarity Trial, did not include immunocompromised patients at all.
However, now that remdesivir has been extensively used in this pandemic, practitioners have developed an anecdotal body of evidence to comfortably implement its frequent use in SOTR. Prior to extensive use of remdesivir, early caution for liver and kidney donors was advised due to remdesivir adverse effects. Indeed, in Wang et al. as well as in the ACTT-1 trial, elevations in transaminases more than five times the upper limit of normal as well as renal impairment with glomerular filtration rate (GFR < 30 mL/min) or renal replacement therapy were exclusion criteria for the trials [9••, 26]. Further case–control studies have found that remdesivir is safe to use, even in patients with impaired renal function [27]. See Table 1 for authorization status, mechanism of action, administration guidelines, and important interactions for remdesivir.
Oral Antivirals
As of the end of 2021, the FDA granted EUAs for two different oral antivirals, nirmatrelvir/ritonavir (Paxlovid, Pfizer), and molnupiravir (Lagevrio, Merck) [28, 29]. Due to limited options, the appeal of these medications is for the use in the outpatient setting. Paxlovid, as a potent inhibitor of CYP3A, will have significant drug-drug interactions with calcineurin inhibitors, mTOR inhibitors, and azole antifungals, which will significantly limit its use in SOTR [30]. Additionally, molnupiravir will likely require extremely high doses to achieve effect without increasing viral resistance [31]. Therefore, the American Society of Transplantation (AST) currently does not recommend use of either of these medications as first-line agents to treat mild COVID-19 in SOTR [32]. See Table 1 for details on for Paxlovid and molnupiravir.
Corticosteroids
Corticosteroids were not initially recommended in the treatment of SARS-CoV-2 due to the theoretical concern regarding delayed viral clearance [33]. However, the RECOVERY Trial, a controlled, open-label trial that randomized over 2000 patients to receive steroids, demonstrated hospitalized patients with COVID had significantly lower 28-day mortality with 6 mg of dexamethasone for up to 10 days [34••]. This finding was borne out in participants requiring supplemental oxygen only. The trial did not provide information on SOTR [34••]. The CoDEX trial of dexamethasone also displayed more ventilator-free days than placebo in patients with moderate to severe acute respiratory distress syndrome (ARDS) [35•]. These studies are in contrast to the CAPE COVID study, which was stopped once RECOVERY results were available, that demonstrated no difference in mortality among patients on low-dose hydrocortisone versus placebo [36•]. This trial included less than 10 patients with immunosuppressive conditions or on immunosuppression and evaluated hydrocortisone, rather than dexamethasone [36•]. This decreased mortality rate in critically ill patients with COVID-19 was also noted in a WHO meta-analysis of these numerous RCTs [37, 38].
Given these findings, the type of steroid and dose of steroids have been examined in a few large trials. Hydrocortisone did not reduce treatment failure at day 21; however, this study was terminated early, leading to an underpowered study [36•]. Likewise, the REMAP-CAP randomized open-label trial of hydrocortisone did not increase support-free days, regardless of the dose of hydrocortisone [39]. Dexamethasone dosing was studied in the COVID STEROID 2 trial, which was a multinational blinded randomized controlled trial of dexamethasone 12 mg compared to 6 mg in adults with severe hypoxemia due to COVID-19. This study found that there was no difference in life support-free days when comparing the doses, though the duration was variable in the treatment group [40•].
SOTRs were not specifically evaluated in sub-group analyses of these trials. Early case studies of transplant recipients noted that patients were already on low-dose steroids for immunosuppression and had similar outcomes of COVID-19 [41]. As the pandemic has progressed, extensive use of steroids in hypoxic and critically ill patients has proven beneficial to decrease hyperinflammation related to COVID-19 [2•, 42]. Risk of secondary opportunistic infections in already immunosuppressed patients is an ongoing concern. In our experience, SOTRs who are hypoxic or crucially ill may still benefit from the use of dexamethasone. In SOTR already on a steroid, it is likely safe to continue.
Immunomodulators
IL-6 inhibitors, specifically tocilizumab and sarilumab, have been examined in large, randomized controlled trials and have exhibited a beneficial effect among patients with progressive moderate to severe COVID-19 who are not yet on mechanical ventilation [43•, 46]. The RECOVERY trial compared tocilizumab and standard of care arms in hospitalized patients with oxygen saturation (SpO2) less than 92% and CRP equal to or greater than 75 mg/L. The tocilizumab arm was associated with reduced all-cause mortality in this specific population [47••]. Both tocilizumab and sarilumab were evaluated in the REMAP-CAP trial, and both treatment arms had higher rate of in-hospital survival and shorter duration of organ support than standard of care. This effect was strongest in those with the highest CRP and enrolled patients within 24 h of ICU admission [48, 49]. While both RECOVERY and REMAP trials confirmed benefit of both tocilizumab and sarilumab among the sickest patients with COVID-19, it is important to note that patients were receiving dexamethasone concomitantly in these trials. Additionally, other studies of tocilizumab have not been as overwhelmingly positive. The COVACTA double-blind RCT of tocilizumab in hospitalized patients showed no survival benefit; however, the median times for recovery and ICU length of stay was shorter in the tocilizumab group than placebo [43]. The EMPACTA double-blind RCT of tocilizumab determined that it lowered rates of mechanical ventilation, ECMO, or death by day 28 but provided no benefit for all-cause mortality at that time [45].
Despite these trials demonstrating advantages of tocilizumab, the REMDACTA double-blind RCT of tocilizumab and remdesivir in hospitalized patients with severe COVID-19 pneumonia found that the combination of remdesivir plus tocilizumab did not shorten time to discharge and there was no difference in mortality between arms [50]. Nevertheless, tocilizumab was given FDA EUA in June of 2021 [51].
In STOR, use of tocilizumab has been evaluated in observational studies, calling into question the safety and efficacy of additional immunosuppression in this population [52]. In an observational cohort of 80 kidney transplant recipients with severe COVID-19 by Perez-Saez et al., in patients who received tocilizumab, the mortality rate was noted to be 32.5%, significantly higher than early studies that reported mortality in SOTR up to 28% [21, 52, 53]. This finding correlated with higher inflammatory markers at baseline in the treated SOTR [52]. Additionally, in a matched cohort study of 117 SOTR, 29 patients received tocilizumab compared to matched controls and no benefit in mortality was found [54]. This study noted that secondary infections occurred frequently in the tocilizumab treatment group, 34% versus 24% in the control group, but it was not statistically significant. The study concluded that tocilizumab is safe to use in SOTR with minimal impact on the net state of immunosuppression [54]. Tocilizumab may be beneficial in SOTR with severe COVID-19 and elevated inflammatory markers.
Kinase inhibitors
Of the kinase inhibitors currently in use, there are randomized clinical data only for baricitinib and ruxolitinib in COVID-19. The ACTT-2 trial randomized over 1000 hospitalized patients to receive remdesivir plus baricitinib or remdesivir plus placebo [55••]. The time to recovery was significantly reduced with combination treatment, predominantly in the patients on high-flow oxygen or noninvasive ventilation. Secondary outcomes showed combination therapy was associated with better clinical status at day 15 in this same subgroup [55••]. Patients who were already getting corticosteroids were excluded from this trial, minimizing confounding. Similar observations were found in the COV-BARRIER study, which compared baricitinib alone with placebo. However, nearly 80% of patients in this trial were on concomitant dexamethasone [56••]. Based on these data, the NIH recommends either baricitinib or tocilizumab in combination with dexamethasone or dexamethasone plus remdesivir for hospitalized patients with rapidly worsening oxygen requirement on high-flow or noninvasive ventilation and high inflammatory markers [7••]. The FDA EUA for baricitinib expands the use to include patients who are mechanically ventilated or on ECMO [57]. Ruxolitinib, an alternate kinase inhibitor, was not associated with faster clinical improvement [58].
Data on baricitinib in SOTR is sparse. Bodro et al. discuss use of baricitinib in 33 kidney transplant recipients (KTR) admitted to the hospital in the early stages of the pandemic [59]. This study found that KTR had better subjective outcomes when treated with anticytokine therapy. Despite the lack of specific studies in SOTR, the NIH still recommends use of baricitinib for patients with severe or critical COVID-19 disease with rapid progression [60]. While Marconi et al. did not find a statistically significant difference in rates of adverse effects, including secondary infection, in the treatment versus control arms, monitoring for secondary infections remains a key concern for patients already on immunosuppression [56••]. The American Society for Transplantation concludes that baricitinib is a useful treatment for severe COVID-19 in patients who progress despite remdesivir and dexamethasone and advises that SOTR who receive baricitinib should be monitored closely for secondary infections [42]. In our experience, baricitinib has been well tolerated when used in patients without proven secondary infection.
Monoclonal Antibodies (MABs)
In randomized controlled trials of the various monoclonal antibodies, outcomes were not stratified by organ transplant recipients specifically. Yet all of them were able to demonstrate improved outcomes among patients with risk factors for more severe COVID-19 disease and hospitalization, namely, reducing hospitalization rates [61].
Bamlanivimab was studied in the Blocking Viral Attachment and Cell Entry with SARS-CoV-2 Neutralizing Antibodies (BLAZE-1) trials, double-blind RCT with three phases. The first phase compared bamlanivimab versus placebo, with a post hoc analysis of high-risk patients revealing lower hospitalizations in the study drug arm [62]. Phase 2, however, did not demonstrate a difference between placebo and bamlanivimab alone, only the combination of bamlanivimab plus etesevimab resulted in decreased viral load. All study arms had fewer hospitalizations [63]. Studies in SOT of both bamlanivimab alone and bamlanivimab plus etesevimab showed that these monoclonal antibodies were safely used and helped prevent COVID-19 disease [64,65,66]. The EUA for bamlanivimab plus etesevimab was granted on February 2021 for high-risk patients with mild to moderate COVID-19 [67, 68]. As of August 2021, this combination was no longer recommended due to decreased susceptibility of Delta and Omicron variants [7••].
Casirivimab/imdevimab (brand name Regeneron) was studied in a three-phase RCT. Regeneron significantly decreased viral level from day 1 through day 7 when compared to placebo [61]. This effect was most notable among seronegative patients, those with no more than 7 days of symptomatic disease. The FDA issued an EUA for Regeneron for mild to moderate COVID-19 at high risk of progression in February 2021 [69]. In a study of 12 kidney transplant recipients, in patients with mild COVID-19 disease, casirivimab/imdevimab resulted in rapid resolution of symptoms and no one required repeat hospitalization [70]. With the latest Omicron variant wave, Regeneron is no longer recommended as it is ineffective against this variant [7••, 71].
Sotrovimab is currently being used against Omicron variant. Sotrovimab targets a portion of the receptor binding domain, which remains highly conserved in the Omicron variant [72]. Ongoing data from phase 3 trial shows lower hospitalization rates in outpatients given sotrovimab versus placebo [73]. Gupta et al. conducted a double-blind placebo controlled trial of sotrovimab that demonstrated an 85% reduction in hospitalization or death in patients who received sotrovimab compared to placebo [72]. Severely immunocompromised patients were excluded from this study [74]. However, we have used sotrovimab in SOTR during the latest Omicron surge with anecdotal success. As of February 2022, FDA EUA for sotrovimab remains active [75].
Bebtelovimab is the most recent monoclonal antibody available to treat COVID-19 and works by binding to the COVID-19 spike protein similar to other monoclonals. To date, bebtelovimab seems to retain activity against both the omicron variant and the BA.2 omicron subvariant [76, 77].
Vaccination and Prophylaxis
Vaccination against COVID-19 has helped limit the spread of the disease. Available vaccines in the USA include the mRNA vaccines, mRNA-1273 (Moderna) and BNT162b2 (Pfizer), and Ad26.COV2.S (J&J). Recommendations for SOTR are to prioritize the mRNA vaccine, as they appear to mount a stronger humoral response compared to adenovirus vector vaccines, such as the J&J vaccine [5••]. Current recommendations regarding vaccine schedules include three doses in the primary series of mRNA vaccines and a booster 3 months after [5••]. If the patient received Ad26.COV2.S (J&J), it is recommended they receive a booster with a mRNA COVID-19 vaccine at least 2 months after the 2nd dose [78].
SOTR response to vaccination has been widely researched and variable in the literature. Antibody response in SOTR after receiving COVID-19 has evaluated spike protein IgG or receptor-binding domain IgG [79•, 80, 81, 82, 83]. These studies have looked at rates of detectable antibodies after two doses of mRNA vaccines, and response is extremely variable, ranging from 0 to 64% [79•, 84, 85]. Improved rates of antibody response have been noted with addition of third dose of mRNA vaccine [86]. T cell response ranges as well, but can be present despite absent antibody [84, 87, 88]. A few studies have gauged clinical effectiveness of the vaccines and show reduced severity of disease in symptomatic COVID-19 and reduced mortality [83, 89, 90]. One single-center study noted an almost 80% reduction in risk of symptomatic COVID-19 in vaccinated SOTR [90]. Notably, these studies were performed prior to the Omicron variant surge.
Pre-exposure prophylaxis is now a consideration with the arrival of tixagevimab + cilgavimab (Evusheld) [91]. Evusheld is indicated in adult and pediatric patients older than 12 years old who are not currently infected with COVID-19 nor have recent exposure to COVID-19 [92]. In the PROVENT trial, Evusheld was shown to decrease the likelihood of developing symptomatic COVID-19 by 77% in a 6-month follow-up period [93•]. Further data from the TACKLE study indicates that Evusheld may be used as prevention and possibly treatment in the future [94]. Patients considered for Evusheld should be moderately to severely immunocompromised and unlikely to mount an immune response to vaccination. Alternatively, recipients should have a contraindication to vaccination due to prior adverse reaction to mRNA vaccine. While this option provides recent SOTR with protection against COVID-19, AST still recommends prioritizing vaccination due to scarcity of Evusheld as it is distributed [42, 95].
Disproven and Not Recommended Medications
Notably, certain medications have been investigated as preventive measures from contracting COVID-19. Ivermectin, an anti-parasitic medication, inhibits replication of viruses in vitro. Meta-analysis of numerous trials does not show any benefit to ivermectin [96, 97].
Data on the use of chloroquine and hydroxychloroquine have not been shown to benefit COVID-19. The FDA EUA was revoked for both drugs due to ineffectiveness, and both have potential to prolong QTc and cause harm (see Fig. 1) [7••, 98].
Colchicine has also been investigated as a potential treatment for hyperinflammatory syndrome that accompanies COVID-19. No clinical benefit has been demonstrated, and colchicine is not currently recommended [42, 99].
Fluvoxamine is a selective serotonin reuptake inhibitor (SSRI) that may reduce cytokine production as demonstrated in mouse models [100]. In the STOP COVID trial, a double-blind RCT of non-hospitalized patients, the fluvoxamine treatment arm did have 0% clinical deterioration compared to 8.3% in placebo arm [101]. However, this study had a short follow-up period with a significant number of patients stopping responding prior to 15-day follow-up [42]. The TOGETHER trial also studied fluvoxamine in a RCT, but statistically showed no difference in primary outcome [102]. At this time, neither the NIH nor the IDSA guidelines recommend routine use of fluvoxamine in the treatment of COVID-19 [7••, 98].
Conclusion
COVID-19 therapeutics have gone through several iterations since the beginning of the pandemic in 2020. SOTRs have often been one of the populations most affected by this disease, and evidence on specific treatment in this population is limited. In our clinical practice, remdesivir remains the antiviral of choice for those hospitalized with moderate COVID-19. Additional treatments for moderate to severe disease include corticosteroids, tocilizumab, or baricitinib. Outpatient treatment for mild COVID-19 includes shorter courses of remdesivir, or oral antivirals, or monoclonal antibodies. As new therapeutics evolve for this virus, it is imperative that immunocompromised patients, specifically SOTRs, are included in studies. Providers should continue ongoing vaccination campaigns for those who remain unvaccinated or partially vaccinated. Prevention with pre-exposure prophylactic medications could provide protection for many who cannot mount an immune response to the vaccine. The progress in the treatment of COVID-19 should include SOTR as the medical community navigates the future of this pandemic.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bartelt L, van Duin D. An Overview of COVID-19 in solid organ transplantation. Clin Microbiol Infect. https://doi.org/10.1016/j.cmi.2022.02.005.
Buehrle DJ, Sutton RR, McCann EL, Lucas AE. A review of treatment and prevention of coronavirus disease 2019 among solid organ transplant recipients. Viruses. 2021;13(9):1706. Review of COVID-19 therapeutics and approved medications for treatmentundefined.
Michaels MG, La Hoz RM, Danziger-Isakov L, Blumberg EA, Kumar D, Green M, et al. Coronavirus disease 2019: Implications of emerging infections for transplantation. Am J Transplant. 2020;20(7):1768–72.
Danziger-Isakov L, Blumberg EA, Manuel O, Sester M. Impact of COVID-19 in solid organ transplant recipients. Am J Transplant. 2021;21(3):925–37. Update on the state of the pandemic as of the time of writing, and its impact on transplantation.
American Society for Transplantation. COVID-19 Vaccine FAQ Sheet 2022 [updated 1/28/2022]. Available from: https://www.myast.org/sites/default/files/012822%20AST%20Vaccine%20FAQ-FINAL%20PDF%20%281%29.pdf. Accessed February 2, 2022. Guidance from major transplant organization regarding COVID-19 vaccination in solid organ transplant recipients.
Qin CX, Moore LW, Anjan S, Rahamimov R, Sifri CD, Ali NM, et al. Risk of breakthrough SARS-CoV-2 infections in adult transplant recipients. Transplantation 2021;105(11):e265–e6. Research demonstrating the risk of acquiring COVID-19 after vaccination in solid organ transplant recipients.
Coronavirus Disease 2019 Treatment Guideline Panel. The COVID-19 treatment guidelines panel's statement on therapies for high-risk, nonhospitalized patients with mild to moderate COVID-19: National Institutes of Health; 2022 [cited 2022]. Available from: https://www.covid19treatmentguidelines.nih.gov/therapies/statement-on-therapies-for-high-risk-nonhospitalized-patients/. Accessed February 2, 2022. Guidelines from the NIH on treatment of COVID-19.
Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–71.
Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the treatment of covid-19 — final report. N Engl J Med. 2020;383(19):1813–26. ACTT-1 trial by the NIH of remdesivir that demonstrated decreased time to recovery
Ader F, Bouscambert-Duchamp M, Hites M, Peiffer-Smadja N, Poissy J, Belhadi D, et al. Remdesivir plus standard of care versus standard of care alone for the treatment of patients admitted to hospital with COVID-19 (DisCoVeRy): a phase 3, randomised, controlled, open-label trial. Lancet Infect Dis. 2022;22(2):209–21 DisCoVeRy randomized control trial of remdesivir, demonstrating effectiveness with early initiation.
Goldman JD, Lye DCB, Hui DS, Marks KM, Bruno R, Montejano R, et al. Remdesivir for 5 or 10 days in patients with severe Covid-19. N Engl J Med. 2020;383(19):1827–37. SIMPLE trial demonstrating effective short course of remdesivir.
Spinner CD, Gottlieb RL, Criner GJ, Arribas López JR, Cattelan AM, Soriano Viladomiu A, et al. Effect of remdesivir vs standard care on clinical status at 11 days in patients with moderate COVID-19: A randomized clinical trial. JAMA 2020;324(11):1048–57. Demonstrating clinical effectiveness of remdesivir for severe COVID-19.
FDA. Fact sheet for health care providers emergency use authorization of Veklury 2021. Available from: https://www.fda.gov/media/137566/download. Accessed February 2, 2022.
Gilead Sciences I. Prescribing Information for Remdesivir 2022. Available from: https://www.gilead.com/-/media/files/pdfs/medicines/covid-19/veklury/veklury_pi.pdf. Accessed February 2, 2022.
Gottlieb RL, Vaca CE, Paredes R, Mera J, Webb BJ, Perez G, et al. Early Remdesivir to prevent progression to severe Covid-19 in outpatients. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2116846. Effectiveness of outpatient use of remdesivir for mild COVID-19.
FDA. FDA Takes Actions to Expand Use of Treatment for Outpatients with Mild to Moderate COVID-29 2022. Available from: https://www.fda.gov/news-events/press-announcements/fda-takes-actions-expand-use-treatment-outpatients-mild-moderate-covid-19. Accessed February 2, 2022.
Consortium WHOST, Pan H, Peto R, Henao-Restrepo A-M, Preziosi M-P, Sathiyamoorthy V, et al. Repurposed antiviral drugs for Covid-19 - Interim WHO solidarity trial results. N Engl J Med. 2021;384(6):497–511 The Solidarity Trial did not demonstrate benefit of remdesivir, though had limatations of the study.
Raja MA, Mendoza MA, Villavicencio A, Anjan S, Reynolds JM, Kittipibul V, et al. COVID-19 in solid organ transplant recipients: A systematic review and meta-analysis of current literature. Transplant Rev (Orlando). 2021;35(1):100588-.
Kates OS, Haydel BM, Florman SS, Rana MM, Chaudhry ZS, Ramesh MS, et al. Coronavirus disease 2019 in solid organ transplant: a multicenter cohort study. Clin Infect Dis. 2021;73(11):e4090–e40e9.
Laracy JC, Verna EC, Pereira MR. Antivirals for COVID-19 in solid organ transplant recipients. Curr Transplant Rep. 2020;1–11. https://doi.org/10.1007/s40472-020-00304-z.
Pereira MR, Mohan S, Cohen DJ, Husain SA, Dube GK, Ratner LE, et al. COVID-19 in solid organ transplant recipients: Initial report from the US epicenter. Am J Transplant. 2020;20(7):1800–8.
Aversa M, Benvenuto L, Anderson M, Shah L, Robbins H, Pereira M, et al. COVID-19 in lung transplant recipients: A single center case series from New York City. Am J Transplant. 2020;20(11):3072–80.
Christensen J, Kumar D, Moinuddin I, Bryson A, Kashi Z, Kimball P, et al. Coronavirus disease 2019 viremia, serologies, and clinical course in a case series of transplant recipients. Transplant Proc. 2020;52(9):2637–41.
Colmenero J, Rodríguez-Perálvarez M, Salcedo M, Arias-Milla A, Muñoz-Serrano A, Graus J, et al. Epidemiological pattern, incidence, and outcomes of COVID-19 in liver transplant patients. J Hepatol. 2021;74(1):148–55.
Lima B, Gibson GT, Vullaganti S, Malhame K, Maybaum S, Hussain ST, et al. COVID-19 in recent heart transplant recipients: Clinicopathologic features and early outcomes. Transplant infectious disease : an official journal of the Transplantation Society 2020;22(5):e13382-e.
Wang Y, Zhang D, Du G, Du R, Zhao J, Jin Y, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. The Lancet. 2020;395(10236):1569–78.
Ackley TW, McManus D, Topal JE, Cicali B, Shah S. A valid warning or clinical lore: an evaluation of safety outcomes of remdesivir in patients with impaired renal function from a multicenter matched cohort. Antimicrob Agents Chemother. 2021;65(2):e02290–20.
Merck & Company. Fact sheet for health care providers Emergency Use Authorization (Eua) of Molnupiravir 2022. Available from: https://www.fda.gov/media/155054/download. Accessed February 2, 2022.
Pfizer. Fact Sheet For Health Care Providers Emergency Use Authorization (Eua) Of Paxlovid 2021. Available from: https://www.covid19oralrx-hcp.com/files/Fact_Sheet_HCP.pdf. Accessed February 2, 2022.
Zijp TR, Toren-Wielema ML, Nannan Panday PV, Kosterink JGW, Berger SP, Touw DJ. Important interactions of immunosuppressants with experimental therapies for novel coronavirus disease (COVID-19): how to act. Ther Drug Monit. 2020;42(4).
Deng X, StJohn SE, Osswald HL, O'Brien A, Banach BS, Sleeman K, et al. Coronaviruses resistant to a 3C-like protease inhibitor are attenuated for replication and pathogenesis, revealing a low genetic barrier but high fitness cost of resistance. J Virol. 2014;88(20):11886–98.
American Society for Transplantation. AST statement on oral antiviral therapy for COVID-19 for organ transplant recipients 2022 [updated Jan 4th, 2022]. Available from: https://www.myast.org/sites/default/files/AST%20Statement%20on%20Oral%20Antiviral%20Therapy%20for%20COVID%20Jan%204%20%282%29.pdf. Accessed February 2, 2022.
Roberts MB, Izzy S, Tahir Z, Al Jarrah A, Fishman JA, El Khoury J. COVID-19 in solid organ transplant recipients: Dynamics of disease progression and inflammatory markers in ICU and non-ICU admitted patients. Transplant infectious disease : an official journal of the Transplantation Society 2020;22(5):e13407-e.
Recovery Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693-704. Recovery trial shows lower mortality with dexamethasone treatment.
Tomazini BM, Maia IS, Cavalcanti AB, Berwanger O, Rosa RG, Veiga VC, et al. Effect of dexamethasone on days alive and ventilator-free in patients with moderate or severe acute respiratory distress syndrome and COVID-19: The CoDEX randomized clinical trial. JAMA. 2020;324(13):1307–16. CoDEX trial of dexamethasone treatment has lower mortality than placebo.
Dequin P-F, Heming N, Meziani F, Plantefève G, Voiriot G, Badié J, et al. Effect of hydrocortisone on 21-day mortality or respiratory support among critically ill patients with COVID-19: a randomized clinical trial. JAMA 2020;324(13):1298–306 CAPE COVID Study of hydrocortisone did not demonstrate benefit of low-dose hydrocortisone.
Pulakurthi YS, Pederson JM, Saravu K, Gupta N, Balasubramanian P, Kamrowski S, et al. Corticosteroid therapy for COVID-19: A systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2021;100(20):e25719.
Group TWREAfC-TW. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020;324(13):1330–41.
Angus DC, Derde L, Al-Beidh F, Annane D, Arabi Y, Beane A, et al. Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: The REMAP-CAP COVID-19 corticosteroid domain randomized clinical trial. Jama. 2020;324(13):1317–29.
The COVID STEROID 2 Trial Group. Effect of 12 mg vs 6 mg of dexamethasone on the number of days alive without life support in adults with COVID-19 and severe hypoxemia: The COVID STEROID 2 randomized trial. JAMA. 2021;326(18):1807–17. Dexamethasone dosing was equivocal between 6mg and 12mg.
Zhu L, Xu X, Ma K, Yang J, Guan H, Chen S, et al. Successful recovery of COVID-19 pneumonia in a renal transplant recipient with long-term immunosuppression. Am J Transplant. 2020;20(7):1859–1863.
Transplantation ASo. COVID-19: FAQs for Organ Transplantation 2022. Available from: https://www.myast.org/sites/default/files/2022_Jan_29.%20Clean_FAQ_COVIDUpdates.pdf.
Rosas IO, Bräu N, Waters M, Go RC, Hunter BD, Bhagani S, et al. Tocilizumab in hospitalized patients with severe Covid-19 pneumonia. N Engl J Med. 2021;384(16):1503–16. Accessed February 2, 2022. COVACTA duble blind RCT Of tocilizumab showed no survival benefit, but shorter median time to recovery.
Hermine O, Mariette X, Tharaux P-L, Resche-Rigon M, Porcher R, Ravaud P, et al. Effect of tocilizumab vs usual care in adults hospitalized with COVID-19 and moderate or severe pneumonia: a randomized clinical trial. JAMA Internal Medicine. 2021;181(1):32–40.
Salama C, Han J, Yau L, Reiss WG, Kramer B, Neidhart JD, et al. Tocilizumab in patients hospitalized with Covid-19 pneumonia. N Engl J Med. 2021;384(1):20–30.
Stone JH, Frigault MJ, Serling-Boyd NJ, Fernandes AD, Harvey L, Foulkes AS, et al. Efficacy of tocilizumab in patients hospitalized with Covid-19. N Engl J Med. 2020;383(24):2333–44.
Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021;397(10285):1637-645. Recovery trial study of tocilizumab versus placebo, which was associated with reduced mortality in patients with severe COVID-19.
The REMAP-CAP Investigators. Interleukin-6 receptor antagonists in critically Ill patients with Covid-19. N Engl J Med. 2021;384(16):1491–502.
Gordon AC, Mouncey PR, Al-Beidh F, Rowan KM, Nichol AD, Arabi YM, et al. Interleukin-6 receptor antagonists in critically Ill patients with Covid-19. N Engl J Med. 2021;384(16):1491–502. https://doi.org/10.1056/NEJMoa2100433.
Rosas IO, Diaz G, Gottlieb RL, Lobo SM, Robinson P, Hunter BD, et al. Tocilizumab and remdesivir in hospitalized patients with severe COVID-19 pneumonia: a randomized clinical trial. Intensive Care Med. 2021;47(11):1258–70.
Genentech I. Fact Sheet For Health Care Providers Emergency Use Authorization (Eua) Of Tocilizumab 2021. Available from: https://www.gene.com/download/pdf/actemra_eua_hcp_fact_sheet.pdf.
Pérez-Sáez MJ, Blasco M, Redondo-Pachón D, Ventura-Aguiar P, Bada-Bosch T, Pérez-Flores I, et al. Use of tocilizumab in kidney transplant recipients with COVID-19. Am J Transplant. 2020;20(11):3182–3190.
Muñoz Serrano A, Arias A, Moreno-Torres V, Calderón J, Vicente N, Cuervas-Mons V. Coronavirus disease 2019 (COVID-19) in solid organ transplant recipients: a case-control study. Ann Transplant. 2021;26:e933152.
Pereira MR, Aversa MM, Farr MA, Miko BA, Aaron JG, Mohan S, et al. Tocilizumab for severe COVID-19 in solid organ transplant recipients: a matched cohort study. Am J Transplant. 2020;20(11):3198–3205.
Kalil AC, Patterson TF, Mehta AK, Tomashek KM, Wolfe CR, Ghazaryan V, et al. Baricitinib plus remdesivir for hospitalized adults with Covid-19. N Engl J Med. 2020;384(9):795–807. ACTT-2 trial of barcitinib plus remdesivir, reduced time to recovery with combination treatment.
Marconi VC, Ramanan AV, de Bono S, Kartman CE, Krishnan V, Liao R, et al. Efficacy and safety of baricitinib for the treatment of hospitalised adults with COVID-19 (COV-BARRIER): a randomised, double-blind, parallel-group, placebo-controlled phase 3 trial. Lancet Respir Med. 2021;9(12):1407–18. COV-BARRIER study compared baricitinib alone versus placebo. Significant confounding due to most patients being on concomitant dexamethasone.
Eli Lilly and Company. Fact Sheet For Health Care Providers Emergency Use Authorization (Eua) Of Baricitinib 2021. Available from: https://www.fda.gov/media/143823/download.
Cao Y, Wei J, Zou L, Jiang T, Wang G, Chen L, et al. Ruxolitinib in treatment of severe coronavirus disease 2019 (COVID-19): A multicenter, single-blind, randomized controlled trial. J Allergy Clin Immunol. 2020;146(1):137–46.e3.
Bodro M, Cofan F, Ríos J, Herrera S, Linares L, Marcos MÁ, Moreno A, Diekmann F. Use of anti-cytokine therapy in kidney transplant recipients with COVID-19. J Clin Med. 2021;10(1551).
National Institutes of Health. Special considerations in solid organ transplant, hematopoietic stem cell transplant, and cellular immunotherapy candidates, donors, and recipients COVID-19 treatment guidelines. 2021.
Weinreich DM, Sivapalasingam S, Norton T, Ali S, Gao H, Bhore R, et al. REGN-COV2, a neutralizing antibody cocktail, in outpatients with Covid-19. N Engl J Med. 2021;384(3):238–251. https://doi.org/10.1056/NEJMoa2035002.
Chen P, Nirula A, Heller B, Gottlieb RL, Boscia J, Morris J, et al. SARS-CoV-2 neutralizing antibody LY-CoV555 in outpatients with Covid-19. N Engl J Med. 2021;384(3):229–37.
Gottlieb RL, Nirula A, Chen P, Boscia J, Heller B, Morris J, et al. Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral load in patients with mild to moderate COVID-19: a randomized clinical trial. JAMA. 2021;325(7):632–44.
Del Bello A, Marion O, Vellas C, Faguer S, Izopet J, Kamar N. Anti-SARS-CoV-2 monoclonal antibodies in solid-organ transplant patients. Transplantation. 2021;105(10):e146–e7.
Sarrell BA, Bloch K, El Chediak A, Kumm K, Tracy K, Forbes RC, et al. Monoclonal antibody treatment for COVID-19 in solid organ transplant recipients. Transplant infectious disease : an official journal of the Transplantation Society. 2022;24(1):e13759.
Kutzler HL, Kuzaro HA, Serrano OK, Feingold A, Morgan G, Cheema F. Initial experience of bamlanivimab monotherapy use in solid organ transplant recipients. Transpl Infect Dis. 2021;23(5):e13662.
Company ELa. Fact Sheet For Health Care Providers Emergency Use Authorization (Eua) Of Bamlanivimab fda.gov2021. Available from: https://www.fda.gov/media/143603/download.
Company ELa. Fact Sheet For Health Care Providers Emergency Use Authorization (Eua) Of Bamlanivimab-Etesevimab 2021. Available from: https://pi.lilly.com/eua/bam-and-ete-eua-factsheet-hcp.pdf.
Regeneron. Fact Sheet For Health Care Providers Emergency Use Authorization (Eua) Of Casirivimab-Imdevimab 2022. Available from: https://www.regeneron.com/downloads/treatment-covid19-eua-fact-sheet-for-hcp.pdf. Accessed February 2, 2022.
Fernandes G, Devresse A, Scohy A, Yombi JC, Belkhir L, De Greef J, et al. Monoclonal antibody therapy for SARS-CoV-2 infection in kidney transplant recipients: a case series from Belgium. Transplantation. 2022;106(1):e107–e8.
Aggarwal A, Stella AO, Walker G, Akerman A, Milogiannakis V, Brilot F et al. SARS-CoV-2 Omicron: evasion of potent humoral responses and resistance to clinical immunotherapeutics relative to viral variants of concern. medRxiv. 2021.12.14.21267772.
Gupta A, Gonzalez-Rojas Y, Juarez E, Crespo Casal M, Moya J, Falci DR, et al. Early treatment for Covid-19 with SARS-CoV-2 neutralizing antibody sotrovimab. N Engl J Med. 2021;385(21):1941–50. https://doi.org/10.1056/NEJMoa2107934.
FDA. Fact sheet for healthcare providers Emergency Use Authorization (EUA) of Sotrovimab 2021. Available from: https://www.fda.gov/media/149534/download.
Dhand A, Razonable RR. COVID-19 and solid organ transplantation: role of anti-SARS-CoV-2 monoclonal antibodies. Curr Transplant Rep. 2022.
GlaxoSmithKline. Fact Sheet For Health Care Providers Emergency Use Authorization (Eua) Of Sotrovimab 2022. Available from: https://gskpro.com/content/dam/global/hcpportal/en_US/Prescribing_Information/Sotrovimab/pdf/SOTROVIMAB-EUA.PDF#nameddest=HCPFS. Accessed February 2, 2022.
FDA. Coronavirus (COVID-19) Update: FDA Authorizes New Monoclonal Antibody for Treatment of COVID-19 that Retains Activity Against Omicron Variant 2022 [updated February 11, 2022]. Available from: https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-new-monoclonal-antibody-treatment-covid-19-retains.
Eli Lilly and Company. Fact Sheet for Healthcare Providers: Emergency Use Authorization for Bebtelovimab fda.gov2022. Available from: https://www.fda.gov/media/156152/download. Accessed February 2, 2022.
Centers for Disease Control and Prevention. COVID-19 Vaccines for Moderately or Severely Immunocompromised People CDC2022 [updated February 17th, 2022]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/immuno.html?s_cid=11707:covid%20booster%20immunocompromised:sem.ga:p:RG:GM:gen:PTN:FY22. Accessed March 1st, 2022.
Boyarsky BJ, Werbel WA, Avery RK, Tobian AAR, Massie AB, Segev DL, et al. Antibody response to 2-dose SARS-CoV-2 mRNA vaccine series in solid organ transplant recipients. JAMA. 2021;325(21):2204–2206 First study that showed SOTR may not mount protective immune response to COVID-19 vaccine.
Rozen-Zvi B, Yahav D, Agur T, Zingerman B, Ben-Zvi H, Atamna A, et al. Antibody response to SARS-CoV-2 mRNA vaccine among kidney transplant recipients: a prospective cohort study. Clin Microbiol Infect. 2021;27(8):1173.e1–e4.
Grupper A, Rabinowich L, Schwartz D, Schwartz IF, Ben-Yehoyada M, Shashar M, et al. Reduced humoral response to mRNA SARS-CoV-2 BNT162b2 vaccine in kidney transplant recipients without prior exposure to the virus. Am J Transplant. 2021;21(8):2719–26.
Safety and immunogenicity of Anti–SARS-CoV-2 messenger RNA vaccines in recipients of solid organ transplants. Annals of Internal Medicine. 2021;174(9):1336–38.
Callaghan CJ, Mumford L, Curtis RMK, Williams SV, Whitaker H, Andrews N, et al. Real-world effectiveness of the Pfizer-BioNTech BNT162b2 and Oxford-AstraZeneca ChAdOx1-S vaccines against SARS-CoV-2 in solid organ and islet transplant recipients. Transplantation. 2022.
Havlin J, Svorcova M, Dvorackova E, Lastovicka J, Lischke R, Kalina T, et al. Immunogenicity of BNT162b2 mRNA COVID-19 vaccine and SARS-CoV-2 infection in lung transplant recipients. J Heart Lung Transplant. 2021;40(8):754–58. https://doi.org/10.1016/j.healun.2021.05.004.
Chavarot N, Ouedrani A, Marion O, Leruez-Ville M, Vilain E, Baaziz M, et al. Poor Anti-SARS-CoV-2 humoral and T-cell responses after 2 injections of mRNA vaccine in kidney transplant recipients treated with belatacept. Transplantation. 2021;105(9):e94–e5. https://doi.org/10.1097/tp.0000000000003784.
Peled Y, Ram E, Lavee J, Segev A, Matezki S, Wieder-Finesod A, et al (2021) Third dose of the BNT162b2 vaccine in heart transplant recipients: Immunogenicity and clinical experience. J Heart Lung Transplant.
Herrera S, Colmenero J, Pascal M, Escobedo M, Castel MA, Sole-González E, et al. Cellular and humoral immune response after mRNA-1273 SARS-CoV-2 vaccine in liver and heart transplant recipients. Am J Transplant. 2021;21(12):3971–9.
Hall VG, Ferreira VH, Ierullo M, Ku T, Marinelli T, Majchrzak-Kita B, et al. Humoral and cellular immune response and safety of two-dose SARS-CoV-2 mRNA-1273 vaccine in solid organ transplant recipients. Am J Transplant. 2021;21(12):3980–9. https://doi.org/10.1111/ajt.16766s.
Ravanan R, Mumford L, Ushiro-Lumb I, Callaghan C, Pettigrew G, Thorburn D, et al. Two doses of SARS-CoV-2 vaccines reduce risk of death due to COVID-19 in solid organ transplant recipients: preliminary outcomes from a UK registry linkage analysis. Transplantation. 2021;105(11):e263–e4.
Aslam S, Liu Jinyuan, Sigler Rachel, Syed Rehan, Tu Xin, Little Susan, De Gruttola Victor. COVID-19 vaccination is protective of clinical disease in solid organ transplant recipients. Transpl Infect Dis. Accepted for publication 2021.
Evusheld (formerly AZD7442) long-acting antibody combination authorised for emergency use in the US for pre-exposure prophylaxis (prevention) of COVID-19 AstraZeneca.com2021 [updated December 8th, 2021]. Available from: https://www.astrazeneca.com/media-centre/press-releases/2021/evusheld-long-acting-antibody-combination-authorised-for-emergency-use-in-the-us-for-pre-exposure-prophylaxis-prevention-of-covid-19.html.
AstraZeneca. Fact Sheet For Health Care Providers Emergency Use Authorization (Eua) Of Tixagevimab co-packaged with cilgavimab 2022. Available from: https://www.fda.gov/media/154701/download.
Levin MJ, Ustianowski A, De Wit S, Launay O, Avila M, Seegobin S, et al. LB5. PROVENT: Phase 3 study of efficacy and safety of AZD7442 (Tixagevimab/Cilgavimab) for pre-exposure prophylaxis of COVID-19 in adults. Open Forum Infect Dis 2021;8(Supplement_1):S810-S. Trial for pre-exposure prophylaxis with Evushield over 6 month follow up period.
AZD7442 reduced risk of developing severe COVID-19 or death in TACKLE Phase III outpatient treatment trial AstraZeneca.com2021. Available from: https://www.astrazeneca.com/media-centre/press-releases/2021/azd7442-phiii-trial-positive-in-covid-outpatients.html. Accessed February 2, 2022.
American Society for Transplantation. AST Statement on Use of Monoclonal Antibody for Pre-Exposure Prophylaxis 2021 [updated December 13, 2021]. Available from: https://www.myast.org/sites/default/files/AST%20Statement%20on%20Use%20of%20Monoclonal%20Antibody_Final_0.pdf.
Podder C, Chowdhury N, Sina M, Haque W. Outcome of ivermectin treated mild to moderate COVID-19 cases: a single-centre, open-label, randomised controlled study. IMC J Med Sci 2020;14.
Popp M, Stegemann M, Metzendorf MI, Gould S, Kranke P, Meybohm P, et al. Ivermectin for preventing and treating COVID-19. Cochrane Database Syst Rev. 2021;7.
IDSA. IDSA Guidelines on the Treatment and Management of Patients with COVID-19 2022. Available from: https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/#.
Tardif J-C, Bouabdallaoui N, L’Allier PL, Gaudet D, Shah B, Pillinger MH, et al. Efficacy of colchicine in non-hospitalized patients with COVID-19. medRxiv. 2021;2021.01.26.21250494. https://doi.org/10.1101/2021.01.26.21250494.
Rosen DA, Seki SM, Fernández-Castañeda A, Beiter RM, Eccles JD, Woodfolk JA, et al. Modulation of the sigma-1 receptor-IRE1 pathway is beneficial in preclinical models of inflammation and sepsis. Sci Transl Med. 2019;11(478):eaau5266.
Lenze EJ, Mattar C, Zorumski CF, Stevens A, Schweiger J, Nicol GE, et al. Fluvoxamine vs placebo and clinical deterioration in outpatients with symptomatic COVID-19: A randomized clinical trial. JAMA. 2020;324(22):2292–300. https://doi.org/10.1001/jama.2020.22760.
Reis G, Dos Santos Moreira-Silva EA, Silva DCM, Thabane L, Milagres AC, Ferreira TS, et al. Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial. Lancet Glob Health. 2022;10(1):e42–e51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare n competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sigler, R., Chen, V. & Law, N. Evolution of Clinical Care in COVID-Infected Solid Organ Transplant Recipients. Curr Transpl Rep 9, 185–198 (2022). https://doi.org/10.1007/s40472-022-00368-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-022-00368-z