Abstract
Introduction
To the best of our knowledge, no comprehensive meta-analysis has been carried out to investigate the effect of different approaches of fasting and calorie restriction on blood pressure.
Aim
Thus, the present systematic review and meta-analysis was designed to examine the effect of fasting and energy restricting diets on blood pressure in adult subjects.
Methods
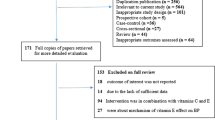
We searched PubMed/Medline, Scopus, the Cochrane Library, and Google Scholar up to June 2019. The clinical trials that examined the effects of fasting and energy restricting diets on Blood Pressure was identified using MESH and non-MESH terms.
Results
23 studies, including a total of 1397 participants, reported SBP and DBP as an outcome measure. Overall results from the random-effects model indicated that fasting and energy restricting administration elicited significant changes in SBP (weight mean difference (WMD): − 1.88 mmHg, 95% CI − 2.50, − 1.25) and DBP (WMD − 1.32 mmHg, 95% CI − 1.81, − 0.84, p = 0.000). Subgroup analyses displayed that intervention duration ≤ 12 weeks more effectively reduced SBP (WMD: -3.26 mmHg) and DBP (WMD − 1.32 mmHg). In addition, these analyses showed that fasting regimens (WMD − 3.26 mmHg) more effectively reduced SBP than energy restricting diets (WMD − 1.09 mmHg).
Conclusion
The principal finding of this study was that fasting and energy restricting diets elicited, overall, significant reductions in SBP and DBP. Subsequent subgroup analyses revealed that intervention duration ≤ 12 weeks and fasting regimens more effectively reduced SBP and DBP.




Similar content being viewed by others
References
World Health Organization. A global brief on hypertension: silent killer, global public health crisis: World Health Day 2013. Geneva: World Health Organization; 2013.
Cicero AFG, Fogacci F, Borghi C. Cost-effectiveness analysis of different hypertension management strategies. Intern Emerg Med. 2019. https://doi.org/10.1007/s11739-019-02153-w.
Cicero AFG, Fogacci F, Tocci G, et al. Awareness of major cardiovascular risk factors and its relationship with markers of vascular aging: data from the Brisighella Heart Study. Nutr Metab Cardiovasc Dis. 2020. https://doi.org/10.1016/j.numecd.2020.03.005.
Appel LJ, Brands MW, Daniels SR, et al. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension. 2006;47:296–308.
Charakida M, Khan T, Johnson W, et al. Lifelong patterns of BMI and cardiovascular phenotype in individuals aged 60–64 years in the 1946 British birth cohort study: an epidemiological study. Lancet Diabetes Endocrinol. 2014;2:648–54.
Fantin F, Giani A, Zoico E, et al. Weight loss and hypertension in obese subjects. Nutrients. 2019;11:1667.
Franz MJ, Vanwormer JJ, Crain AL, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755–67.
Moroshko I, Brennan L, O'Brien P. Predictors of dropout in weight loss interventions: a systematic review of the literature. Obes Rev. 2011;12:912–34.
Longo VD, Mattson MP. Fasting: molecular mechanisms and clinical applications. Cell Metab. 2014;19:181–92.
Harris L, Hamilton S, Azevedo LB, et al. Intermittent fasting interventions for treatment of overweight and obesity in adults: a systematic review and meta-analysis. JBI Database Syst Rev Implement Rep. 2018;16:507–47.
Headland M, Clifton PM, Carter S, et al. Weight-loss outcomes: a systematic review and meta-analysis of intermittent energy restriction trials lasting a minimum of 6 months. Nutrients. 2016;8:354.
Horne BD, Muhlestein JB, Anderson JL. Health effects of intermittent fasting: hormesis or harm? A systematic review. Am J Clin Nutr. 2015;102:464–70.
St-Onge M-P, Ard J, Baskin ML, et al. (2017) Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2017;135:e96–e121.
Johnson JB, Summer W, Cutler RG, et al. Alternate day calorie restriction improves clinical findings and reduces markers of oxidative stress and inflammation in overweight adults with moderate asthma. Free Radic Biol Med. 2007;42:665–74.
Castello L, Froio T, Maina M, et al. Alternate-day fasting protects the rat heart against age-induced inflammation and fibrosis by inhibiting oxidative damage and NF-kB activation. Free Radic Biol Med. 2010;48:47–544.
Wan R, Ahmet I, Brown M, et al. Cardioprotective effect of intermittent fasting is associated with an elevation of adiponectin levels in rats. J Nutr Biochem. 2010;21:413–7.
Wan R, Camandola S, Mattson MP. Intermittent fasting and dietary supplementation with 2-deoxy-d-glucose improve functional and metabolic cardiovascular risk factors in rats. FASEB J. 2003;17:1133–4.
Li C, Sadraie B, Steckhan N, et al. Effects of a one-week fasting therapy in patients with type-2 diabetes mellitus and metabolic syndrome—a randomized controlled explorative study. Exp Clin Endocrinol Diabetes. 2017;125:618–24.
Harris L, McGarty A, Hutchison L, et al. Short-term intermittent energy restriction interventions for weight management: a systematic review and meta-analysis. Obes Rev. 2018;19:1–13.
Cioffi I, Evangelista A, Ponzo V, et al. Intermittent versus continuous energy restriction on weight loss and cardiometabolic outcomes: a systematic review and meta-analysis of randomized controlled trials. J Transl Med. 2018;16:371.
Barnosky AR, Hoddy KK, Unterman TG, et al. Intermittent fasting vs daily calorie restriction for type 2 diabetes prevention: a review of human findings. Transl Res. 2014;164:302–11.
Seimon RV, Roekenes JA, Zibellini J, et al. Do intermittent diets provide physiological benefits over continuous diets for weight loss? A systematic review of clinical trials. Mol Cell Endocrinol. 2015;418:153–72.
Davis C, Clarke R, Coulter S, et al. Intermittent energy restriction and weight loss: a systematic review. Eur J Clin Nutr. 2016;70:292.
Alhamdan B, Garcia-Alvarez A, Alzahrnai A, et al. Alternate-day versus daily energy restriction diets: which is more effective for weight loss? A systematic review and meta-analysis. Obes Sci Pract. 2016;2:293–302.
Moher D, Liberati A, Tetzlaff J, et al. Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89:873–80.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated. March 2011). The Cochrane Collaboration; 2011. http://www.training.cochrane.org/handbook.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2015;5:13.
Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Palmer TM, Peters JL, Sutton AJ, et al. Contour-enhanced funnel plots for meta-analysis. Stata J. 2008;8:242.
Hirsh SP, Pons M, Joyal SV, et al. Avoiding holiday seasonal weight gain with nutrient-supported intermittent energy restriction: a pilot study. J Nutr Sci. 2019;8:e11. https://doi.org/10.1017/jns.2019.8.
Trepanowski JF, Kroeger CM, Barnosky A, et al. Effects of alternate-day fasting or daily calorie restriction on body composition, fat distribution, and circulating adipokines: secondary analysis of a randomized controlled trial. Clin Nutr. 2018;37:1871–8.
Wei M, Brandhorst S, Shelehchi M, et al. Fasting-mimicking diet and markers/risk factors for aging, diabetes, cancer, and cardiovascular disease. Sci Transl Med. 2017. https://doi.org/10.1126/scitranslmed.aai8700.
Zuo L, He F, Tinsley GM, et al. Comparison of high-protein, intermittent fasting low-calorie diet and heart healthy diet for vascular health of the obese. Front Physiol. 2016;7:350.
Varady KA, Bhutani S, Klempel MC, et al. (2013) Alternate day fasting for weight loss in normal weight and overweight subjects: a randomized controlled trial. Nutr J. 2013;12:146. https://doi.org/10.1186/1475-2891-12-146.
Bhutani S, Klempel MC, Kroeger CM, et al. Alternate day fasting with or without exercise: effects on endothelial function and adipokines in obese humans. e-SPEN J. 2013;8:e205–e209209.
Astbury NM, Aveyard P, Nickless A, et al. Doctor Referral of Overweight People to Low Energy total diet replacement Treatment (DROPLET): pragmatic randomised controlled trial. BMJ (Online). 2018. https://doi.org/10.1136/bmj.k3760.
Lee S, Norheim F, Langleite TM, et al. Effect of energy restriction and physical exercise intervention on phenotypic flexibility as examined by transcriptomics analyses of mRNA from adipose tissue and whole-body magnetic resonance imaging. Physiol Rep. 2016;4:e13019.
Bowen J, Brindal E, James-Martin G, et al. Randomized trial of a high protein, partial meal replacement program with or without alternate day fasting: similar effects on weight loss, retention status, nutritional, metabolic, and behavioral outcomes. Nutrients. 2018;10:E1145.
Venchiarutti RL, Byth K, Marks JL, et al. Comparing the effectiveness of general dietary advice versus a very low energy diet in an obese outpatient population in Australia. Eat Weight Disord. 2019;24:739–47.
Lambert EA, Sari CI, Eikelis N, et al. Effects of moxonidine and low-calorie diet: cardiometabolic benefits from combination of both therapies. Obesity. 2017;25:1894–902.
Izadi V, Haghighatdoost F, Moosavian P, et al. Effect of low-energy-dense diet rich in multiple functional foods on weight-loss maintenance, inflammation, and cardiovascular risk factors: a randomized controlled trial. J Am Coll Nutr. 2018;37:399–405.
Karimi G, Azadbakht L, Haghighatdoost F, et al. Low energy density diet, weight loss maintenance, and risk of cardiovascular disease following a recent weight reduction program: a randomized control trial. J Res Med Sci. 2016;21:32.
Kessler CS, Stange R, Schlenkermann M, et al. A nonrandomized controlled clinical pilot trial on 8 wk of intermittent fasting (24 h/wk). Nutrition. 2018;46:143–152.e2.
Ismail S, Shamsuddin K, Latiff KA, et al. Voluntary fasting to control post-Ramadan weight gain among overweight and obese women. Sultan Qaboos Univ Med J. 2015;15:98–104.
Teng NIMF, Shahar S, Rajab NF, et al. Improvement of metabolic parameters in healthy older adult men following a fasting calorie restriction intervention. Aging Male. 2013;16:177–83.
Harder-Lauridsen NM, Rosenberg A, Benatti FB, et al. Ramadan model of intermittent fasting for 28 d had no major effect on body composition, glucose metabolism, or cognitive functions in healthy lean men. Nutrition. 2017;37:92–103.
Fernandes JFR, Da Silva AL, Kaiser SE, et al. The effects of moderate energy restriction on apnoea severity and CVD risk factors in obese patients with obstructive sleep apnoea. Br J Nutr. 2015;114:2022–31.
Harrison DG, Gongora MC. Oxidative stress and hypertension. Med Clin. 2009;93:621–35.
Kizhakekuttu TJ, Widlansky ME. Natural antioxidants and hypertension: promise and challenges. Cardiovasc Ther. 2010;28:e20–e32.
Widlansky ME, Gokce N, Keaney JF, et al. The clinical implications of endothelial dysfunction. J Am Coll Cardiol. 2003;42:1149–60.
Rebrin I, Forster MJ, Sohal RS. Association between life-span extension by caloric restriction and thiol redox state in two different strains of mice. Free Radic Biol Med. 2011;51:225–33.
Zainal TA, Oberley TD, Allison DB, et al. Caloric restriction of rhesus monkeys lowers oxidative damage in skeletal muscle. FASEB J. 2000;14:1825–36.
Lane M, Ingram D, Roth G. Calorie restriction in nonhuman primates: effects on diabetes and cardiovascular disease risk. Toxicol Sci. 1999;52:41–8.
Burt VL, Whelton P, Roccella EJ, et al. Prevalence of hypertension in the US adult population: results from the Third National Health and Nutrition Examination Survey, 1988–1991. Hypertension. 1995;25:305–13.
Walford RL, Mock D, Verdery R, et al. Calorie restriction in biosphere 2: alterations in physiologic, hematologic, hormonal, and biochemical parameters in humans restricted for a 2-year period. J Gerontol Ser A Biol Sci Med Sci. 2002;57:B211–B224224.
Dolinsky VW, Dyck JR. Calorie restriction and resveratrol in cardiovascular health and disease. Biochim Biophys Acta (BBA). 2011;1812:1477–89.
Fontana L, Meyer TE, Klein S, et al. Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. Proc Natl Acad Sci. 2004;101:6659–63.
Rahmani J, Varkaneh HK, Clark C, et al. The influence of fasting and energy restricting diets on IGF-1 levels in humans: a systematic review and meta-analysis. Ageing Res Rev. 2019;53:100910.
Dharmashankar K, Widlansky ME. Vascular endothelial function and hypertension: insights and directions. Curr Hypertens Rep. 2010;12:448–55.
Klempel MC, Kroeger CM, Varady KA. Alternate day fasting (ADF) with a high-fat diet produces similar weight loss and cardio-protection as ADF with a low-fat diet. Metabolism. 2013;62:137–43.
Ryan AS, Nicklas BJ. Reductions in plasma cytokine levels with weight loss improve insulin sensitivity in overweight and obese postmenopausal women. Diabetes Care. 2004;27:1699–705.
Jae SY, Fernhall B, Heffernan KS, et al. Effects of lifestyle modifications on C-reactive protein: contribution of weight loss and improved aerobic capacity. Metabolism. 2006;55:825–31.
Scagliusi FB, Ferriolli E, Pfrimer K, et al. Characteristics of women who frequently under report their energy intake: a doubly labelled water study. Eur J Clin Nutr. 2009;63:1192.
Schwingshackl L, Hoffmann G. Low-carbohydrate diets and cardiovascular risk factors. Obes Rev. 2013;14:183–4.
Nielsen BM, Nielsen MM, Toubro S, et al. Past and current body size affect validity of reported energy intake among middle-aged Danish men. J Nutr. 2009;139:2337–433.
Kris-Etherton P, Eckel RH, Howard BV, et al. Lyon diet heart study: benefits of a Mediterranean-Style, National Cholesterol Education Program/American Heart Association Step I dietary pattern on cardiovascular disease. Circulation. 2001;103:1823–5.
Fontana L, Weiss EP, Villareal DT, et al. Long-term effects of calorie or protein restriction on serum IGF-1 and IGFBP-3 concentration in humans. Aging Cell. 2008;7:681–7.
Tam CS, Frost EA, Xie W, et al. No effect of caloric restriction on salivary cortisol levels in overweight men and women. Metabolism. 2014;63:194–8.
Fontana L, Villareal DT, Das SK, et al. Effects of 2-year calorie restriction on circulating levels of IGF-1, IGF-binding proteins and cortisol in nonobese men and women: a randomized clinical trial. Aging Cell. 2016;15:22–7.
Barnosky A, Kroeger CM, Trepanowski JF, et al. Effect of alternate day fasting on markers of bone metabolism: an exploratory analysis of a 6-month randomized controlled trial. Nutr Healthy Aging. 2017;4:255–63.
Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54:1046–55.
Brandhorst S, Choi IY, Wei M, et al. A periodic diet that mimics fasting promotes multi-system regeneration, enhanced cognitive performance, and health span. Cell Metab. 2015;22:86–99.
Funding
The authors sincerely thank Shahid Beheshti University of Medical Sciences for all moral and material supports. This study was supported by grants from the Student Research Committee Shahid Beheshti University of Medical Sciences (SBMU), Tehran, Iran (Grant’s ID: (19388) IR.SBMU.RETECH.REC.1398.665).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kord-Varkaneh, H., Nazary-Vannani, A., Mokhtari, Z. et al. The Influence of Fasting and Energy Restricting Diets on Blood Pressure in Humans: A Systematic Review and Meta-Analysis. High Blood Press Cardiovasc Prev 27, 271–280 (2020). https://doi.org/10.1007/s40292-020-00391-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-020-00391-0