Abstract
Skin wound healing is a crucial process for regenerating healthy skin and avoiding the undesired consequences associated with open skin wounds. For epidermolysis bullosa (EB), a debilitating group of fragile skin disorders currently without a cure, skin blistering can often be severe and heal poorly, increasing susceptibility to life-threatening complications. To prevent these, investigational therapies have been exploring the use of tissue-engineered skin substitutes (TESSs) aimed at replacing damaged skin and promoting long-term wound closure. These products have either been developed in house or commercially sourced and are composed of allogeneic or autologous human skin cells, often with some form of bioscaffolding. They can be broadly classified based on their cellular composition: keratinocytes (epidermal substitutes), fibroblasts (dermal substitutes) or a combination of both (composite substitutes). Encouraging long-term wound healing has been achieved with epidermal substitutes. However, these substitutes have not demonstrated the same efficacy for all patients, which may be due to the molecular heterogeneity observed between EB subtypes. Autologous composite TESSs, which more closely resemble native human skin, are therefore being investigated and may hold promise for treating an extended range of patients. Additionally, future TESSs for EB are focused on using gene-corrected patient skin cells, which have already demonstrated remarkable long-term wound healing capabilities. In this review, we provide an overview of the different TESSs that have been investigated in clinical studies to treat patients with EB, as well as their long-term wound healing results. Where available, we describe the methods used to develop these products to inform future efforts in this field.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Epidermolysis bullosa is a debilitating skin blistering disease currently without a cure. Severe disease subtypes such as junctional epidermolysis bullosa and recessive dystrophic epidermolysis bullosa often cause grievous and poorly healing blisters that increase susceptibility to life-threatening complications. |
Tissue-engineered skin substitutes comprising human skin cells (dermal fibroblasts and/or epidermal keratinocytes) are currently being investigated as potential curative therapies in clinical studies to promote long-term wound healing. |
Epidermal tissue-engineered skin substitutes comprising autologous keratinocytes, especially those using genetically corrected autologous patient cells, have demonstrated the most promising long-term wound healing benefits for junctional epidermolysis bullosa. For recessive dystrophic epidermolysis bullosa, which has a different molecular pathology, tissue-engineered skin substitutes comprising both fibroblasts and keratinocytes may prove more effective for promoting long-term wound closure. |
1 Introduction
Epidermolysis bullosa (EB) comprises a group of rare skin fragility disorders characterised by mutations in basement membrane zone (BMZ) structural proteins in the skin [1]. To date, 16 different genes have been implicated across the four classical EB types, EB simplex (EBS), junctional EB (JEB), dystrophic EB (DEB) and Kindler EB [2]. These types and their underlying subtypes are classified based on the affected protein, plane of blister formation and molecular aetiology (Fig. 1) [3]. The unifying diagnostic characteristic of EB is cutaneous and/or mucosal blistering following minor mechanical trauma or friction. For severe subtypes including recessive dystrophic EB (RDEB) and JEB, which involve a deeper plane of skin detachment, congenital blistering can be severe and heal poorly, increasing susceptibility to life-threatening complications including sepsis, infection and aggressive squamous cell carcinomas [2]. A curative therapy to treat these cutaneous symptoms is therefore urgently required to replace the current palliative treatment measures, which include the prevention of infection, pain management and protective bandaging [3].

Adapted from reference [4] with Copyright permission from Elsevier
A diagrammatic representation of the basement membrane zone (BMZ) of the skin. The different layers of the BMZ and important attachment complexes required for dermal-epidermal skin adhesion are shown on the left. These complexes, which include hemidesmosomes, anchoring filaments, and anchoring fibrils, provide adhesion between basal keratinocytes, the lamina densa, and the papillary dermis. The causative EB protein components that make up these complexes within the different levels of the BMZ and the EB type they are associated with is depicted on the right.
Autologous skin grafts, either full or split thickness, have long been used to cover a range of skin injuries and are currently the gold standard for treating thermal injuries and chronic wounds [5]. However, as the availability of native skin is limited, treatment with autologous grafts can be difficult when a large proportion of skin is affected [5]. To bypass this issue, tissue-engineered skin substitutes (TESSs) were developed as an alternative to autologous grafts and have shown tremendous promise for treating a variety of dermatoses [6]. A TESS comprises human skin cells cultured with or without some form of bioscaffolding into a safe product that can replace damaged skin and restore its basic functional and structural properties. This includes the prevention of water loss, high tensile strength and serving as an immunological barrier against pathogens [6]. Upon grafting onto damaged skin, these products are designed to accelerate wound healing and ultimately provide long-term therapeutic benefit by regenerating mechanically stable skin.
The methods and materials used to develop TESSs capable of promoting permanent wound closure is a growing area of research. For EB, TESSs have only been approved for clinical use in Japan [1]. However, a variety have shown encouraging long-term wound healing results in clinical studies, with some rapidly approaching clinical translation. In this review, we summarise the efficacy of the various TESSs investigated so far to treat patients with EB. Where available, we include an overview of the methods used for manufacture to inform future efforts in this field.
2 EB Wound Healing
The skin is a multilayered organ composed of two major cell types. The outermost layer, the epidermis, is avascular and primarily comprises sheets of keratinocytes that continually regenerate [7]. The epidermis is reinforced by the underlying vascular dermis that is primarily composed of fibroblasts embedded within a stromal scaffolding of extracellular matrix (ECM) structural proteins including elastin fibres, collagens and glycosaminoglycans. Adhesion between the dermis and epidermis is achieved by the collection of structural macromolecules located at the BMZ at the interface between these layers [7]. In the case of EB, aberrant BMZ proteins often lead to skin detachment between dermal and epidermal compartments, resulting in blister formation (Fig. 2). Following the induction of blistering, a complex but highly organised wound repair process involving a well-defined sequence of events (inflammation, cellular proliferation, tissue remodeling) is activated and usually acts to repair the wound and regenerate healthy skin [6]. During the inflammatory stage immediately following wounding, fibrin is activated and forms a clot that serves as a transient wound matrix to seal the wound and prevent bleeding. This matrix is subsequently invaded by immune cells that help control infection and remove necrotic tissue. During the proliferative phase, fibroblasts migrate into the wound matrix to promote angiogenesis and secrete ECM components to generate granulation tissue. Epithelialisation begins at the wound edges as epidermal stem cells (EpiSCs) proliferate to cover the wound. Lastly, the wound matrix is remodeled following the secretion of structural ECM components and matrix metalloproteinases by keratinocytes and fibroblasts [6]. Imbalances across all phases of this process have been observed in EB wounds, which can lead to the formation of chronic wounds and hypertrophic scarring [1, 8,9,10].

Adapted from Reference [8] with permission from Elsevier
Blister formation for junctional epidermolysis bullosa (JEB) and recessive dystrophic epidermolysis bullosa (RDEB). For RDEB (top), mutations in type VII collagen (C7), the main constituent of anchoring fibrils, results in blister formation and skin detachment within the papillary dermis. These mutations can alter the deposition of laminin 332 and integrin α6β4 at the BMZ and disrupt downstream signalling pathways, resulting in defects in keratinocyte migration and epithelialisation. For JEB (bottom), blister formation, most commonly caused by mutations in laminin 332, results in skin detachment at the level of the lamina lucida. In both cases, epithelialisation can be compromised due to an impaired ability of the regenerated epidermis to attach to the granulation tissue underneath. This can lead to a protracted wound healing process that can exacerbate inflammation, and in the long term, lead to the formation of chronic wounding, fibrosis and scarring.
Research into wound healing of EB blisters has been limited to the most severe subtypes, JEB and RDEB [1]. In both cases, the lack of functional BMZ proteins can compromise the epithelialisation of new wounds due to the detachment of the newly regenerated epidermis from the granulation tissue underneath (Fig. 2). Additionally for RDEB, a lack of type VII collagen (C7) has been shown to alter the deposition of the BMZ proteins laminin 332 and integrin α6β4, leading to changes in downstream signalling pathways that cause defects in keratinocyte migration [10]. The resulting delay in wound repair can promote inflammation by (1) favouring colonisation and infection by microbes and (2) continuously activating the skin repair process in skin regions that are prone to friction and recurrent blistering [1, 8]. The subsequent increase in pro-inflammatory molecules (e.g., interleukin-6, interleukin receptors, defensins, antimicrobial peptides) can impair cell migration at the wound site and promote cellular senescence [8]. Over time, successive rounds of blistering and impaired wound healing can deplete skin appendage EpiSC reservoirs that are crucial for skin repair [9], inducing chronic wounding and fibrosis [1]. In RDEB blisters, fibrosis is commonly observed and is a result of low C7 levels that impair maturation of granulation tissue and migration of fibroblasts [10]. These defects are associated with a variety of molecular alterations, most notably an upregulation of transforming growth factor beta-1 (TGF-β1), which promotes the deposition of various ECM proteins and matrix metalloproteinase inhibitors, ultimately leading to defects in tissue remodeling, the formation of a fibrotic microenvironment and scarring [8, 10].
3 TESSs for EB
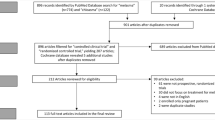
A variety of TESSs developed in house or commercially sourced have been tested on patients with EB. For TESSs developed in house, cell-based investigational therapies have used human skin cells with wild type BMZ genes, while gene-based strategies have used genetically corrected autologous skin cells derived from patients with EB [1]. Classification of TESSs for EB is broadly based on the cellular composition: keratinocytes (epidermal substitutes), dermal fibroblasts (dermal substitutes) or a combination of both (composite substitutes) (Fig. 3). Depending on the source of these cells, they can be further classified as autografts (using autologous skin cells) or allografts (using allogeneic skin cells). Various natural and synthetic materials have been used as scaffolding to provide structural or functional support for the cells (Fig. 3). However, biomaterials derived from the dermis such as type I collagen [11,12,13,14,15,16,17,18,19] and hyaluronic acid (HA) [16, 20] have been most prevalent. These natural polymers provide low toxicity and good biodegradability, and carry a low chance of immunological rejection. Additionally, they possess natural epitopes that allow them to promote normal physiological function of the ECM by binding to cells via adhesion or cell receptor proteins [21].
Schematic overview of the different components and types of tissue-engineered skin substitutes (TESSs) assessed for epidermolysis bullosa (EB) in clinical studies. To generate TESSs, human skin cells (fibroblasts and/or keratinocytes) are enzymatically isolated from skin biopsies, expanded under different cell culture conditions, and used in conjunction with or without some form of scaffolding material. TESSs have either been developed in house or commercially sourced and can be broadly categorised based on their cellular composition. Epidermal substitutes consist of an epidermal layer of stratified keratinocyte sheets with or without an underlying acellular dermal layer containing scaffolding. Dermal substitutes contain fibroblasts embedded within a scaffolded dermal matrix. Composite substitutes are composed of an epidermal layer of stratified keratinocyte sheets and an underlying scaffolded dermal layer containing fibroblasts. Three commercially sourced TESSs assessed in clinical studies for EB are also shown. Kaloderm® is an epidermal substitute composed of allogeneic keratinocyte sheets. Dermagraft® is a dermal substitute composed of allogeneic fibroblasts cultured within a polyglactin mesh scaffold. Apligraf® is a composite substitute composed of an allogeneic epidermal layer of keratinocytes and an underlying dermal layer consisting of allogeneic fibroblasts. Created with BioRender.com
3.1 Allografts: A Viable Strategy for EB?
The choice between using allogeneic or autologous cells to generate TESSs can significantly influence clinical outcomes. Allogeneic cells are (1) more quickly available as they bypass the downtime required for cell expansion, (2) avoid the need for skin harvesting operations, which can be burdensome for patients with EB, and (3) can be used in cases when autologous cells are unavailable [22, 23]. However, allografts carry a high risk of graft rejection and infection because of immunogenicity from the host, and consequently, allograft survival for burns, deep dermal lesions and venous leg ulcers has been reported to persist only for several weeks following transplantation [24,25,26,27,28]. Allografts have therefore been used as temporary dressings in burn patients to prepare wound beds for autologous cells [29, 30], or in conjunction with autografts to stimulate epithelialisation of EB wounds [31, 32]. When used alone for EB, however, allografts have generally not permitted the long-term wound closure that has been achieved with autologous-based TESSs [33,34,35]. Theoretically, allografts could instead be used to transiently cover and prepare wound beds on severely affected EB patients while they wait for autologous TESSs to be prepared. Allografts may also be required in severe circumstances when no viable autologous cells are available. To increase the chance of graft acceptance and persistence in these cases, one potential solution is to first establish immune tolerance via infusions of human leukocyte antigen-matched haematopoietic stem cells. Although this strategy has not been attempted with TESSs for EB, it has been successfully demonstrated using split-thickness allografts to treat JEB [36] and harvested epidermal allografts to treat RDEB [37]. In the latter case, 100% wound closure was reported for most of the 35 allografted sites across eight patients with RDEB after one year, with C7 and anchoring fibrils detected in the one analysed allograft site [37]. However, this approach is more cumbersome and can significantly delay the time to treatment for patients.
3.2 Epidermal Skin Substitutes
The first cell type from the skin to be isolated and investigated was keratinocytes [38], and consequently epidermal TESSs have been extensively studied for treating a range of dermatoses including burns [6]. As the stratified sheets of keratinocytes within the epidermis are sustained by EpiSCs confined to the basal layer [1], a sufficient population of EpiSCs should ideally be incorporated into epidermal substitutes to provide a permanent source of grafted keratinocytes for long-term wound closure.
For EB, epidermal substitutes have been the most widely explored as keratinocytes express the majority of BMZ proteins implicated across all subtypes. However, more attention has been given to JEB as most of the causative proteins associated with this subtype are predominantly expressed by keratinocytes [1]. In most cases, these products have been developed based on a method pioneered by Rheinwald and Green who discovered a technique for isolating keratinocytes from 2cm2 patches of harvested skin and expanding them into approximately 200 80cm2 keratinocyte sheets [38, 39]. In brief, disaggregated epidermal cell suspensions are plated on a feeder layer of lethally irradiated 3T3 murine fibroblasts and cultured over a few weeks to form a stratified epidermis. Dispase is then used to detach the final keratinocyte sheets from cell culture surfaces. Upon grafting onto wounds, these products can promote wound healing via keratinocyte proliferation and migration, as well as through the release of cytokines and growth factors [40]. However, as the sheets of keratinocytes are fragile, handling and immobilising the grafts onto wound beds can be challenging [41,42,43]. Supportive dressings or delivery systems have therefore been required to support the vulnerable epithelia during transplantation. Additionally, some groups have generated more robust final products by culturing keratinocytes on acellular matrices composed of biomaterials from the dermis [11, 20, 33]. These dermal components can also contribute to wound healing by stimulating keratinocyte growth, which in turn can reduce the lead time associated with keratinocyte culture [44].
3.2.1 Cultured Epidermal Autografts
Epidermal substitutes engineered using autologous patient skin cells were among the first TESSs assessed for EB (Table 1) [11, 20, 41]. Initial efforts used autologous keratinocytes from unblistered areas of skin. While the causative mutations were not corrected in these cases, keratinocytes were cultured on acellular dermal matrices to promote epithelialisation. The first report was by Carter and colleagues who treated severe facial ulcers in three patients with JEB [11]. Autologous keratinocytes were plated on type I collagen sponges and grown for three weeks into multilayered keratinocyte sheets measuring 7cm in diameter. Following transplantation of the collagen sponge-based cultured epidermal autografts (CEAs), full epithelialisation was reported in two patients after 7 and 10 months, respectively, while for the third patient only partial epithelialisation was achieved [11]. In a second case study, Wollina and colleagues used CEAs with HA scaffolding to treat chronic ulcers on the upper trunk and head of a patient with RDEB [20]. Autologous keratinocytes were seeded onto flexible 20mm thick esterified HA membranes with a perforated structure and cultured for three weeks. Membranes included small pores to promote multilayered growth and larger pores to facilitate wound drainage. The final grafts were transplanted onto three skin ulcers, resulting in complete stabilisation of the two wounds on the trunk and > 50% closure of the wound on the head after 12 months [20].
3.2.2 Genetically Revertant CEAs
The primary concern with using autologous patient cells to generate TESSs is the presence of causative EB mutations. Therefore, more recent CEAs have been generated using autologous cells isolated from patches of unblistered skin that are known to contain genetically revertant cells that have spontaneously corrected their germline mutation (Table 1) [45]. This phenomenon is known as revertant mosaicism (RM) and has been reported for several genes (KRT14, LAMB3, COL17A1, FERMT1, COL7A1) across all four classical EB types. Although usually an uncommon occurrence, a remarkably high incidence of 36% and 33% has been reported for JEB patients with COL17A1 and LAMB3 mutations, respectively [45, 46].
The first report of RM-based CEAs for EB was by Gostynski and colleagues who cultured autologous keratinocytes derived from clinically identified revertant skin for five weeks into keratinocyte sheets (6cm × 7cm) for grafting onto a JEB patient’s leg [47]. The wound bed was prepared using a polyacrylate adhesive plaster to remove the interfollicular epidermis covering an 84cm2 region, exposing the lamina densa at the BMZ. Although the graft appeared healthy and free of scarring four months after transplantation, the adhesive plaster test induced skin loosening. Retrospective analysis of the keratinocytes from the graft site revealed that <3% of the cells had revertant type XVII collagen (the causative JEB protein for this patient) despite the donor skin containing ~30% revertant cells, explaining the lack of functional repair [47]. Although there is not a clear explanation for the loss of revertant cells at the graft site, it is possible that resident C7-mutant EpiSCs from the wound edges or skin appendage stem cell reservoirs colonised the grafted wound bed during healing and outcompeted the revertant stem cells.
For RDEB, Shinkuma and colleagues isolated autologous keratinocytes from unblistered skin on a patient’s back to generate keratinocyte sheets to treat ulcers on a patient’s knee, right shoulder, abdomen and axilla [42]. Mechanical displacement of the vulnerable keratinocyte sheets was an issue and resulted in poor wound healing for grafts on the axilla, abdomen and shoulder. However, the grafted site on the right knee completely epithelialised after two weeks and remained closed for over 10 years [42]. In a 16-year follow-up study, analysis of synthesised C7 complementary DNA from the preserved graft site revealed genetically revertant sequences, confirming that RM was an important key to the closure of the ulcer [48]. These findings paved the way for an investigator-initiated clinical trial in Japan using the same method to assess the therapeutic benefit of CEAs from clinically identified revertant skin [48]. Eight refractory ulcers on each of three patients with RDEB were grafted with RM-based CEAs. Rapid epithelialisation was reported for two patients, with 100% of the treated ulcers completely epithelialised after 76 weeks. For the third patient, re-transplantation was required because of renewed blistering. However, 52.6% of ulcerated sites still showed complete epithelialisation at 76 weeks, achieving the study’s primary endpoint (>50%) [48]. Following this trial in 2019, RM-based CEAs were approved in Japan as a therapy for DEB and JEB and are now covered under the public healthcare system [48]. Since approval, at least 20 patients in Japan have been treated with this therapy [1].
3.2.3 Genetically Modified CEAs
As highlighted by Gostynski and colleagues [47], successfully identifying patches of skin with a sufficient population of genetically revertant cells can pose a challenge for RM-based CEAs. To bypass this issue,ex vivo gene-based strategies have genetically corrected EB patient keratinocytes before use in CEA generation with remarkable results (Table 1). In each case, keratinocytes have been transduced with retroviral vectors carrying full-length copies of wild type BMZ genes. Following integration into genomic DNA, the transgenes can be stably expressed and compensate for the lack of function of the mutant gene [33,34,35].
The first clinical demonstration of gene-modified CEAs was described by Mavilio and colleagues in a phase I/II clinical trial [35]. Autologous keratinocytes derived from a JEB patient with mutations in LAMB3 (encoding the β3 subunit of laminin 332) were transduced with retroviral vectors containing full-length LAMB3 complementary DNA and subsequently grown into keratinocyte sheets. Final CEAs were grafted onto nine sites on the patient’s legs, which either had a fragile epidermis or poorly healing and infected ulcers. Epidermal adhesion in the absence of blistering, inflammation, or infection was reported after one year, with the clinical benefits persisting for over 16 years as reported at a later follow-up [49, 50]. Another successful case was later reported using the same method, this time to treat a larger (80cm2) refractory ulcer on the leg of another LAMB3-deficient patient with JEB [34]. The grafted area remained healed for the duration of the two-year follow-up, with histological analysis confirming a healthy BMZ and epidermis [34, 50].
Despite the success achieved in the two JEB clinical studies, one criticism was the small total area grafted (~0.06m2), which did not have a significant impact on the patients’ quality of life [34, 35, 50]. To assess the suitability of this treatment to treat large skin lesions, a compassionate use study used gene-modified CEAs to cover widespread blistering on a LAMB3-deficient boy with severe JEB [33]. Most of the keratinocyte sheets used in this trial were generated on a fibrin substrate, resulting in more robust final grafts. This method is routinely used for treating ocular and massive skin burns and prevents contraction of the keratinocyte sheets, enabling the same number of EpiSCs to generate larger CEAs [33]. Remarkably, transplantation of the final fibrin-based CEAs resulted in the regeneration of approximately 80% of the patient’s epidermis, which remained stable even after the application of mechanical force five years later [51]. A phase II/III clinical trial using this same method is currently underway and aims to treat at least six patients with JEB [50].
Success in all three JEB trials was believed to be a result of successful EpiSC targeting. In each case, subconfluent keratinocyte cultures were monitored for holoclone-forming stem cells [52], providing an indirect estimate of EpiSC-targeting efficiency, and therefore, graft durability [33,34,35]. Data from these trials demonstrated that only a small population of holoclone-forming stem cells corresponding to approximately 5% of the total grafted cells were responsible for the long-term maintenance of a functioning transgenic epidermis [50]. This equated to the transplantation of approximately 1.8 × 103 EpiSCs per cm2 to regenerate and maintain nearly the entire epidermis of the severely affected boy [33].
For RDEB, gene-modified CEAs were assessed in a phase I/II clinical trial to treat seven patients with severe cutaneous symptoms [43]. Autologous keratinocytes transduced with modified Moloney murine leukaemia retroviral vectors (LZRSE) harbouring full-length C7 complementary DNA were grown into keratinocyte sheets. The keratinocyte sheets measuring 35cm2 each were transplanted onto six wounds on each patient. All wound beds were cauterised to reduce the number of resident C7-mutant EpiSCs that could potentially outcompete the grafted stem cells. Although encouraging wound healing was reported for some of the patients after two years, significant variability was observed. Overall, wound healing generally declined from 83% of wounds showing >75% closure after three months to 46% of wounds after two years [53]. A phase III clinical trial is currently underway to further assess the efficacy of this treatment in 15 patients with RDEB (ClinicalTrials.gov identifier NCT04227106).
The differences in wound healing between the JEB and RDEB trials is not well understood. Difficulty to successfully immobilise some of the grafts for a few days after transplantation was thought to contribute to the overall wound healing variability in the RDEB trial. In addition, this trial did not monitor holoclone-forming stem cells, which may not have been sufficiently targeted to enable long-term therapeutic benefit. A third possible explanation relates to the different plane of skin blistering between the two subtypes. Blistering in RDEB occurs within the papillary dermis and consequently produces wound beds without a discernible basement membrane. For JEB, the higher level of skin blistering within the lamina lucida results in wound beds with an intact basement membrane, which may help facilitate adhesion of grafted keratinocyte sheets to the underlying dermis.
A further possible explanation for the variable wound healing in the RDEB trial was the absence of functional C7 from dermal fibroblasts. Preclinical research has suggested that anchoring fibril formation and dermal-epidermal adhesion in composite TESSs is dependent on functional C7 from both major skin cell types [55]. However, in transgenic murine rescue experiments, it was reported that fibroblast or keratinocyte-specific re-expression of C7 in an RDEB mouse model was sufficient to produce anchoring fibrils and reverse all the cutaneous manifestations of RDEB [54]. In the murine rescue experiments, it is important to note that a retroviral expression vector was used to express C7 above normal physiological levels. Therefore, C7 overexpression in either skin cell type may have been sufficient to regenerate healthy skin by compensating for the lack of functional C7 from the other cell type. Although this discrepancy is yet to be resolved, it raises the possibility that composite TESSs composed of both keratinocytes and fibroblasts may be more effective for promoting long-term wound closure in patients with RDEB. This point may be clarified following the completion of the ongoing phase I/II clinical trial assessing composite substitutes for RDEB (ClinicalTrials.gov identifier NCT04186650). Additionally, the more robust nature of these products may help to avoid issues related to mechanical graft displacement that were reported in the RDEB trial.
3.2.4 Epidermal Allografts
Allogeneic keratinocytes expanded from a healthy donor have also been used to generate keratinocyte sheets for EB. However, their success has been limited by the lack of long-term stable engraftment. This issue has previously been noted in burn patients where epidermal allograft rejection has been reported after an average of two weeks due to high keratinocyte immunogenicity [24]. Epidermal allografts have consequently been investigated as temporary dressings in combination with split-thickness autografts to stimulate the proliferation and migration of resident keratinocytes in EB wounds via the release of cytokines and growth factors [31, 32]. In addition, they have also been assessed in cases when the use of autologous cells has been impractical (Table 2) [12, 22, 31, 56].
Epidermal allografts have provided some success for JEB; however, they have generally been limited by short follow-up times and, in some cases, multiple grafting procedures have been required for wound closure [23, 31, 56]. In one study, epidermal allografts were used to treat chronic facial ulcers on a five-year-old patient with JEB [56]. Allogeneic keratinocytes derived from the patient’s biological mother were cultured for up to 10 days to generate keratinocyte sheets [50]. Following four grafting procedures over a six-month period, the facial ulcers epithelialised and remained closed for the duration of the eight-month follow-up [56]. Graft versus host disease was not evident and may have been reduced owing to the use of keratinocytes from a related donor [57]. In another study, allogeneic keratinocyte sheets were used to treat a neonate with JEB [31]. Significant epithelialisation was observed across all wounds covering approximately 70% of the patient’s total body surface. However, graft rejection was evident at multiple sites where renewed blistering accompanied with infection was observed [31].
For RDEB, Schofield and colleagues generated allogeneic keratinocyte sheets to treat donor sites on six patients that were being used to harvest split-thickness autografts for surgical procedures [31, 58]. Although four out of the six allografted sites healed faster than control wounds after seven days, no difference in C7 was observed across any of the grafted sites compared to pre-grafted skin [31]. In a second study, McGrath and co-workers generated allogeneic keratinocyte sheets to treat 10 patients with severe RDEB [22]. Despite some pain alleviation, the treatment provided little clinical benefit [22]. In both cases, the lack of anchoring fibrils at the grafted sites suggested that the allogeneic donor cells were not being maintained.
For EBS, one group used the commercially available cultured epidermal substitute Kaloderm® (Tego Science, Seoul, Korea) engineered using keratinocytes derived from neonatal foreskin to cover three large skin lesions on the foot of a paediatric patient [23]. Twice-weekly grafting of Kaloderm® for three weeks resulted in a 50% reduction in wound surface area across the allografted sites [23]. No long-term follow-up was reported.
3.3 Dermal Skin Substitutes
Dermal fibroblasts play an important role in regenerating damaged epithelia and accelerating wound healing [59]. They secrete ECM components including collagens, glycoproteins and fibrin, which potently activate fibroblast and keratinocyte proliferation and migration, as well as provide structural integrity for the dermis [40, 59, 60]. Additionally, fibroblasts also deposit C7 at the BMZ, albeit to a lesser extent than keratinocytes [55]. Fibroblast cell therapy has therefore been evaluated for RDEB and has included intralesional injections of gene-corrected fibroblasts and cultured dermal allografts (CDAs) [1]. To engineer CDAs, various scaffolds have been investigated including amniotic membranes and type I collagen sponges (Table 3) [61,62,63,64]. However, besides increasing initial rates of wound healing, CDAs have not enhanced C7 expression in the long term and re-application has often been required to enable blister closure. Instead, these products may be more effective as temporary biological dressings by providing a source of growth factors for resident skin cells and by helping to regenerate the dermal bed for later engraftment with CEAs.
The first cultured dermal allografts (CDAs) used for RDEB were based on a method developed by Kubo and Kuroyanagi consisting of fibroblasts grown on a bilayered spongy matrix of atelo-collagen and HA [16, 64]. In brief, monolayered HA sponges cross-linked with ethylene glycol diglycidyl ether are perforated with 1mm2 holes. To obtain the final bilayered sponges, these pores are filled with an aqueous solution of atelo-collagen. Fibroblasts are then seeded onto the collagen side of the sponge and cultured for one week [16]. One group applied this method to cover intractable skin ulcers on the feet of two patients with RDEB [17]. New CDAs were applied twice weekly for the first fortnight and weekly after that. Complete epithelialisation after three weeks was reported for one patient, while partial epithelialisation was reported after four weeks for the other. However, electron microscopy and immunofluorescence failed to detect increases in C7 at the grafted sites, suggesting that wound healing was a consequence of cytokines and growth factors secreted by fibroblasts [17]. A second group used the same method to treat persistent blisters on the legs and forearms of three patients with RDEB [61]. Transplantation of CDAs twice weekly for two to six weeks increased wound granulation after one week, with epithelialisation appearing at the wound edges after four weeks [61]. No long-term follow-up was published for both clinical studies.
Amniotic membranes have also been used for scaffolding because of their beneficial anti-inflammatory and wound healing properties [65]. They have proven safe and easy to handle and have successfully treated venous ulcers and massive burns by promoting rapid epithelialisation [62]. For EB, a pilot study generated CDAs consisting of dermal fibroblasts cultured on amniotic membrane scaffolding derived from healthy neonates to treat three ulcers on each of seven patients with RDEB [62]. To prepare acellular scaffolds, the cells from the amniotic membranes were separated from the underlying basement membrane using a cell scraper. To construct CDAs, fibroblasts were seeded onto the acellular membranes where they were cultured on a non-adhesive plate for five days at the air–liquid interface. Twelve weeks after transplantation, only 28% of the treated wounds (six wounds) had reduced in size by at least 70%, with one wound (5%) healing completely [62].
The commercially available, cultured dermal substitute Dermagraft® (Organogenesis, Canton, MA, USA) has been assessed to treat RDEB. Dermagraft® is composed of allogeneic neonatal fibroblasts seeded within a bioabsorbable, three-dimensional polyglactin mesh scaffold [63]. During manufacture, the fibroblasts proliferate and fill the interstices within the scaffolding and release ECM proteins including collagen and glycosaminoglycans, as well as growth factors and cytokines. Together, these components form a three-dimensional bioscaffold comprised of metabolically active fibroblasts capable of regenerating the injured dermal bed and stimulating the keratinocytes above to epithelialise [63]. One group used this product to treat 55 persistent skin blisters across six patients with RDEB. Although 80–100% epidermal regeneration was noted for each blister two weeks post-grafting, some grafts broke down in the following weeks [63].
3.4 Composite Skin Substitutes
Composite TESSs are the most advanced products and consist of an epidermal layer of keratinocytes and an underlying dermal layer composed of fibroblasts embedded within a stromal scaffold. In addition to providing dermal-epidermal adhesion, these substitutes are more robust, more accurately resemble normal skin and combine the wound healing properties of both skin cell types [21]. They have been extensively used to treat burns, with type I collagen and glycosaminoglycans constituting the most common stromal scaffolding [6]. For EB, composite substitutes with fibrin stromal scaffolding engineered from genetically modified autologous patient cells have been routinely tested preclinically on mouse models with promising results [66,67,68,69,70,71]. However in clinical studies, experimentation with composite autografts is limited (Table 4) [72], although an ongoing phase I/II clinical trial is currently assessing autologous gene-modified composite substitutes to treat three patients with RDEB (ClinicalTrials.gov identifier NCT04186650). Instead, commercially available allogeneic products have been relied upon (Table 4) [13,14,15, 18, 19].
3.4.1 Cultured Composite Autografts
To the best of our knowledge, cultured composite autografts have only been reported in one clinical study for EB [72]. In this case, Matriderm®, an acellular elastin-hydrolysate dermal substitute comprising collagen I, III, and V, was used to cover skin lesions on the hand of a patient with RDEB and prepare the wound bed. Upon complete dermal regeneration 10 days later, the resulting wound bed was covered by cultured composite autografts comprising fibroblasts and keratinocytes that had been co-cultivated for four days. Two years after grafting, complete wound healing was reported and the patient was able to use his hand for everyday activities including writing [72]. Although the patient’s causative mutations were not actively corrected in this case, the final grafts may have contained revertant cells to enable long-term wound closure; however, this was not specified.
3.4.2 Cultured Composite Allografts
The commercially available composite allograft Apligraf® (Organogenesis) has been assessed for treating a range of EB subtypes [13,14,15, 18, 19]. Apligraf® is a culture-derived TESS comprising a dermal layer of neonatal fibroblasts embedded within a bovine type I collagen gel and an epidermal layer of neonatal keratinocytes [13]. Its success in treating diabetic foot ulcers, venous leg ulcers and mild-to-severe burns has been attributed to the similar morphologic, metabolic, and biochemical characteristics compared to normal human skin [73]. Apligraf® is thought to stimulate wound healing by providing cytokines, growth factors and ECM components [73].
The use of Apligraf® for EB was first reported by Falabella and colleagues who treated a newborn with the Dowling-Meara variant of EBS [13]. Before transplantation, grafts with incisions to allow exudate drainage were placed onto selected deep lesions. Rapid wound healing was reported after three days at all graft sites despite the development of widespread blistering elsewhere. Twenty days after grafting, approximately 40% of the patient’s body surface had been covered with Apligraf® and was mostly free of blistering apart from several minor blisters on the feet and left leg after 11 weeks [13]. These promising findings stimulated the launch of an open-label uncontrolled study by the same group assessing the safety and efficacy of Apligraf® in 15 patients with a range of EB subtypes (nine RDEB, five EBS, one JEB) [14]. A total of 78 wounds (69 acute and nine chronic, i.e., difficult to heal) were treated across all patients, although not all wounds were monitored as some patients did not return for clinical evaluations. At the final evaluation after 18 weeks, 11 out of the 14 (79%) followed-up acute wounds had healed. For the chronic wounds, four out of nine (44%) had healed after 12 weeks; however, after 18 weeks, only two of these wounds (22%) remained closed [14]. Overall, these results suggest that Apligraf® may be effective in encouraging faster healing of acute EB wounds and preventing the translation of these wounds into chronic wounds in the short term.
The longer term wound healing potential of Apligraf® has yielded variable results, with some research on venous ulcers [74] and deep dermal wounds [73] reporting only temporary graft persistence for up to eight weeks based on DNA analysis. Consequently, Apligraf® has been suggested to be suitable only as a temporary wound dressing to expedite the healing process [76]. For EB, several studies have provided longer term follow-ups of up to one year using Apligraf® to heal full-thickness skin lesions [18] and treat pseudosyndactyly [15, 19]. One group used a meshed form of Apligraf® to cover full-thickness lesions on the face of a 12-year-old patient with EB, which remained closed after one year [18]. In another study, 96 graft sites across nine children with various EB subtypes (five RDEB, three EBS, one JEB) were treated with Apligraf® that had been fenestrated to enable exudate drainage [15]. Overall, >90% of the wounds healed over the course of six months to a year. However, DNA analysis of biopsy samples showed that some patients contained no Apligraf® donor cells [15]. Therefore, it is unlikely that Apligraf® can provide a permanent source of allogeneic cells to enable lifelong wound closure for patients with EB. Additionally, the relatively high cost and brief five-to-ten-day shelf-life present further barriers to routine clinical use [77].
One group used cultured composite allografts involving a type I collagen matrix for the dermal layer [12]. Fibroblasts were seeded onto porous type I collagen sponges. Two days later, keratinocytes were seeded on a layer of non-porous collagen gel on the opposite surface of the sponge and cultured for one to two weeks. The final grafts were transplanted onto ulcers on the hands of seven patients with RDEB. Overall, these treatments were well tolerated, and increased the time to recurrence of pseudosyndactyly and joint contractures by approximately two-fold [12].
4 Conclusions and Future Perspectives
TESSs have shown tremendous promise as curative therapies for the acute and unremitting skin wounds characteristic of severe EB subtypes such as JEB and RDEB. While a variety of TESSs have been trialled in patients, epidermal substitutes have proven the most effective for restoring the expression of keratinocyte-specific BMZ proteins and enabling long-term wound closure for JEB. For RDEB, however, epidermal substitutes have not provided the same clinical benefit. Possible explanations for this discrepancy include the absence of functional C7 from dermal fibroblasts and the difference in pathophysiology between the two subtypes [55]. Therefore, composite substitutes may prove to be more efficacious alternatives for treating patients with RDEB. Although the use of composite substitutes for EB has not produced good clinical results to date, this is most likely due to the fact that in most cases allogeneic cells have been used. This point may be clarified following the completion of the ongoing phase I/II trial assessing autologous gene-modified composite substitutes for RDEB (ClinicalTrials.gov identifier NCT04186650).
A primary goal of skin engineering research is the development of TESSs that better resemble the structure, appearance and function of native human skin. For this reason, emerging types of TESSs incorporating additional cell types are being explored pre-clinically for a range of skin pathologies [6]. This includes other resident skin cells such as pigment-producing melanocytes, dendritic Langerhans cells to promote protective immunity following skin infection, and Merkel cells which play a critical role in the somatosensory system [6]. Moving beyond skin cells, human stem cells including mesenchymal stem cells and induced pluripotent stem cells are also being evaluated for their therapeutic potential to promote faster wound healing. As these cell types express alternative signalling pathways to skin cells, their addition may also enable the generation of anatomic skin structures [78]. One group assessed a biological dressing composed of ~30 million Wharton’s jelly-derived mesenchymal stem cells seeded onto an acellular human skin matrix of allogeneic origin to treat an EB wound [79]. An assessment 30 days after transplantation was promising and revealed that the dressing had been infiltrated by host cells and neovascularisation had occurred [79]. Finally, as immune cells such as macrophages and neutrophils play an important role as inflammatory effectors during wound healing, their addition could enhance the regeneration potential of future TESSs [6].
Gene therapy is beginning to revolutionise personalised medicine. This has been exemplified through the remarkable wound healing results achieved using epidermal TESSs generated by combinatorial gene and cell therapies [33,34,35]. Other gene-based investigational strategies are also being assessed for EB and may provide alternative curative therapies. A recent phase I/II clinical trial for RDEB consisting of topically applied herpes simplex virus type 1 harbouring wild type C7 demonstrated remarkable wound closure, and consequently, a phase III trial has been launched [80]. However, a big limitation of this approach is that it only enables transient C7 expression, and therefore repeated application will be required to maintain blister closure. Other strategies such as suspensions of gene-modified skin cells sprayed onto skin wounds or injections of gene-modified skin cells may provide simplified alternatives to TESSs and enable quicker treatment for patients [81, 82]. As the field of gene therapy continues to evolve, it is likely that these approaches will take over the clinical landscape for EB and provide lifesaving treatments for people experiencing this debilitating group of genodermatoses.
References
Natsuga K, Shinkuma S, Hsu CK, Fujita Y, Ishiko A, Tamai K, et al. Current topics in Epidermolysis bullosa: pathophysiology and therapeutic challenges. J Dermatol Sci. 2021;104(3):164–76. https://doi.org/10.1016/j.jdermsci.2021.11.004.
Hou PC, Wang HT, Abhee S, Tu WT, McGrath JA, Hsu CK. Investigational treatments for epidermolysis bullosa. Am J Clin Dermatol. 2021;22(6):801–17. https://doi.org/10.1007/s40257-021-00626-3.
Bardhan A, Bruckner-Tuderman L, Chapple ILC, Fine JD, Harper N, Has C, et al. Epidermolysis bullosa. Nat Rev Dis Primers. 2020;6(1):78. https://doi.org/10.1038/s41572-020-0210-0.
Has C, Nyström A, Saeidian AH, Bruckner-Tuderman L, Uitto J. Epidermolysis bullosa: molecular pathology of connective tissue components in the cutaneous basement membrane zone. Matrix Biol. 2018;71–72:313–29. https://doi.org/10.1016/j.matbio.2018.04.001.
Nicholas MN, Jeschke MG, Amini-Nik S. Methodologies in creating skin substitutes. Cell Mol Life Sci. 2016;73(18):3453–72. https://doi.org/10.1007/s00018-016-2252-8.
Sierra-Sánchez Á, Kim KH, Blasco-Morente G, Arias-Santiago S. Cellular human tissue-engineered skin substitutes investigated for deep and difficult to heal injuries. NPJ Regen Med. 2021;6(1):35. https://doi.org/10.1038/s41536-021-00144-0.
Abdo JM, Sopko NA, Milner SM. The applied anatomy of human skin: a model for regeneration. Wound Med. 2020;28: 100179. https://doi.org/10.1016/j.wndm.2020.100179.
Cianfarani F, Zambruno G, Castiglia D, Odorisio T. Pathomechanisms of altered wound healing in recessive dystrophic epidermolysis bullosa. Am J Pathol. 2017;187(7):1445–53. https://doi.org/10.1016/j.ajpath.2017.03.003.
Fujimura Y, Watanabe M, Ohno K, Kobayashi Y, Takashima S, Nakamura H, et al. Hair follicle stem cell progeny heal blisters while pausing skin development. EMBO Rep. 2021;22(7): e50882. https://doi.org/10.15252/embr.202050882.
Nyström A, Velati D, Mittapalli VR, Fritsch A, Kern JS, Bruckner-Tuderman L. Collagen VII plays a dual role in wound healing. J Clin Invest. 2013;123(8):3498–509. https://doi.org/10.1172/JCI68127.
Carter DM, Lin AN, Varghese MC, Caldwell D, Pratt LA, Eisinger M. Treatment of junctional epidermolysis bullosa with epidermal autografts. J Am Acad Dermatol. 1987;17(2 Pt 1):246–50. https://doi.org/10.1016/s0190-9622(87)70199-6.
Eisenberg M, Llewelyn D. Surgical management of hands in children with recessive dystrophic epidermolysis bullosa: use of allogeneic composite cultured skin grafts. Br J Plast Surg. 1998;51(8):608–13. https://doi.org/10.1054/bjps.1998.9997.
Falabella AF, Schachner LA, Valencia IC, Eaglstein WH. The use of tissue-engineered skin (Apligraf) to treat a newborn with epidermolysis bullosa. Arch Dermatol. 1999;135(10):1219–22. https://doi.org/10.1001/archderm.135.10.1219.
Falabella AF, Valencia IC, Eaglstein WH, Schachner LA. Tissue-engineered skin (Apligraf) in the healing of patients with epidermolysis bullosa wounds. Arch Dermatol. 2000;136(10):1225–30. https://doi.org/10.1001/archderm.136.10.1225.
Fivenson DP, Scherschun L, Choucair M, Kukuruga D, Young J, Shwayder T. Graftskin therapy in epidermolysis bullosa. J Am Acad Dermatol. 2003;48(6):886–92. https://doi.org/10.1067/mjd.2003.502.
Kubo K, Kuroyanagi Y. Development of a cultured dermal substitute composed of a spongy matrix of hyaluronic acid and atelo-collagen combined with fibroblasts: fundamental evaluation. J Biomater Sci Polym Ed. 2003;14(7):625–41. https://doi.org/10.1163/156856203322274897.
Natsuga K, Sawamura D, Goto M, Homma E, Goto-Ohguchi Y, Aoyagi S, et al. Response of intractable skin ulcers in recessive dystrophic epidermolysis bullosa patients to an allogeneic cultured dermal substitute. Acta Derm Venereol. 2010;90(2):165–9. https://doi.org/10.2340/00015555-0776.
Ozerdem OR, Wolfe SA, Marshall D. Use of skin substitutes in pediatric patients. J Craniofac Surg. 2003;14(4):517–20. https://doi.org/10.1097/00001665-200307000-00023.
Phillips J, Rockwell WB. Surgical treatment of recessive dystrophic epidermolysis bullosa in the hand: use of tissue-engineered skin (Apligraf). Ann Plast Surg. 2003;50(4):441–2. https://doi.org/10.1097/01.SAP.0000048065.92291.CD.
Wollina U, Konrad H, Fischer T. Recessive epidermolysis bullosa dystrophicans (Hallopeau-Siemens): improvement of wound healing by autologous epidermal grafts on an esterified hyaluronic acid membrane. J Dermatol. 2001;28(4):217–20. https://doi.org/10.1111/j.1346-8138.2001.tb00120.x.
Przekora A. A concise review on tissue engineered artificial skin grafts for chronic wound treatment: can we reconstruct functional skin tissue in vitro? Cells. 2020;9(7):1622. https://doi.org/10.3390/cells9071622.
McGrath JA, Schofield OM, Ishida-Yamamoto A, O’Grady A, Mayou BJ, Navsaria H, et al. Cultured keratinocyte allografts and wound healing in severe recessive dystrophic epidermolysis bullosa. J Am Acad Dermatol. 1993;29(3):407–19. https://doi.org/10.1016/0190-9622(93)70203-6.
Shin KC, Park BY, Kim HK, Kim WS, Bae TH. The use of cultured allogenic keratinocyte grafting in a patient with epidermolysis bullosa simplex. Ann Dermatol. 2011;23(Suppl. 3):S393–7. https://doi.org/10.5021/ad.2011.23.S3.S393.
Auböck J, Irschick E, Romani N, Kompatscher P, Höpfl R, Herold M, et al. Rejection, after a slightly prolonged survival time, of Langerhans cell-free allogeneic cultured epidermis used for wound coverage in humans. Transplantation. 1988;45(4):730–7. https://doi.org/10.1097/00007890-198804000-00013.
Brain A, Purkis P, Coates P, Hackett M, Navsaria H, Leigh I. Survival of cultured allogeneic keratinocytes transplanted to deep dermal bed assessed with probe specific for Y chromosome. BMJ. 1989;298(6678):917–9. https://doi.org/10.1136/bmj.298.6678.917.
Burt AM, Pallett CD, Sloane JP, O’Hare MJ, Schafler KF, Yardeni P, et al. Survival of cultured allografts in patients with burns assessed with probe specific for Y chromosome. BMJ. 1989;298(6678):915–7. https://doi.org/10.1136/bmj.298.6678.915.
Oliver AM, Kaawach W, Mithoff EW, Watt A, Abramovich DR, Rayner CR. The differentiation and proliferation of newly formed epidermis on wounds treated with cultured epithelial allografts. Br J Dermatol. 1991;125(2):147–54. https://doi.org/10.1111/j.1365-2133.1991.tb06062.x.
Phillips TJ, Bhawan J, Leigh IM, Baum HJ, Gilchrest BA. Cultured epidermal autografts and allografts: a study of differentiation and allograft survival. J Am Acad Dermatol. 1990;23(2 Pt 1):189–98. https://doi.org/10.1016/0190-9622(90)70197-p.
Chua AWC, Khoo YC, Truong TTH, Woo E, Tan BK, Chong SJ. From skin allograft coverage to allograft-micrograft sandwich method: a retrospective review of severe burn patients who received conjunctive application of cultured epithelial autografts. Burns. 2018;44(5):1302–7. https://doi.org/10.1016/j.burns.2018.01.021.
Cuono C, Langdon R, McGuire J. Use of cultured epidermal autografts and dermal allografts as skin replacement after burn injury. Lancet. 1986;1(8490):1123–4. https://doi.org/10.1016/s0140-6736(86)91838-6.
Petrof G, Abdul-Wahab A, McGrath JA. Cell therapy in dermatology. Cold Spring Harb Perspect Med. 2014;4(6): a015156. https://doi.org/10.1101/cshperspect.a015156.
Beele H, Naeyaert JM, Monstrey S, Kint A. Ulcers in pretibial epidermolysis bullosa. Grafting with autologous meshed split-thickness skin and allogeneic cultured keratinocytes. Arch Dermatol. 1995;131(9):990–2. https://doi.org/10.1001/archderm.131.9.990.
Hirsch T, Rothoeft T, Teig N, Bauer JW, Pellegrini G, De Rosa L, et al. Regeneration of the entire human epidermis using transgenic stem cells. Nature. 2017;551(7680):327–32. https://doi.org/10.1038/nature24487.
Bauer JW, Koller J, Murauer EM, De Rosa L, Enzo E, Carulli S, et al. Closure of a large chronic wound through transplantation of gene-corrected epidermal stem cells. J Invest Dermatol. 2017;137(3):778–81. https://doi.org/10.1016/j.jid.2016.10.038.
Mavilio F, Pellegrini G, Ferrari S, Di Nunzio F, Di Iorio E, Recchia A, et al. Correction of junctional epidermolysis bullosa by transplantation of genetically modified epidermal stem cells. Nat Med. 2006;12(12):1397–402. https://doi.org/10.1038/nm1504.
Kopp J, Horch RE, Stachel KD, Holter W, Kandler MA, Hertzberg H, et al. Hematopoietic stem cell transplantation and subsequent 80% skin exchange by grafts from the same donor in a patient with Herlitz disease. Transplantation. 2005;79(2):255–6. https://doi.org/10.1097/01.tp.0000144325.01925.be.
Ebens CL, McGrath JA, Riedl JA, Keith AR, Lilja G, Rusch S, et al. Immune tolerance of allogeneic haematopoietic cell transplantation supports donor epidermal grafting of recessive dystrophic epidermolysis bullosa chronic wounds. Br J Dermatol. 2021;184(6):1161–9. https://doi.org/10.1111/bjd.19503.
Rheinwald JG, Green H. Serial cultivation of strains of human epidermal keratinocytes: the formation of keratinizing colonies from single cells. Cell. 1975;6(3):331–43. https://doi.org/10.1016/s0092-8674(75)80001-8.
Green H, Kehinde O, Thomas J. Growth of cultured human epidermal cells into multiple epithelia suitable for grafting. Proc Natl Acad Sci USA. 1979;76(11):5665–8. https://doi.org/10.1073/pnas.76.11.5665.
Spiekstra SW, Breetveld M, Rustemeyer T, Scheper RJ, Gibbs S. Wound-healing factors secreted by epidermal keratinocytes and dermal fibroblasts in skin substitutes. Wound Repair Regen. 2007;15(5):708–17. https://doi.org/10.1111/j.1524-475X.2007.00280.x.
Collin B, Balderson D, Papini R, Marsden J, Moss C. Cultured autologous keratinocyte grafting of chronic erosions in three patients with epidermolysis bullosa. Clin Exp Dermatol. 2006;31(5):718–9. https://doi.org/10.1111/j.1365-2230.2006.02200.x.
Shinkuma S, Sawamura D, Fujita Y, Kawasaki H, Nakamura H, Inoie M, et al. Long-term follow-up of cultured epidermal autograft in a patient with recessive dystrophic epidermolysis bullosa. Acta Derm Venereol. 2014;94(1):98–9. https://doi.org/10.2340/00015555-1592.
Siprashvili Z, Nguyen NT, Gorell ES, Loutit K, Khuu P, Furukawa LK, et al. Safety and wound outcomes following genetically corrected autologous epidermal grafts in patients with recessive dystrophic epidermolysis bullosa. JAMA. 2016;316(17):1808–17. https://doi.org/10.1001/jama.2016.15588.
Kaur A, Midha S, Giri S, Mohanty S. Functional skin grafts: where biomaterials meet stem cells. Stem Cells Int. 2019;2019:1286054. https://doi.org/10.1155/2019/1286054.
Lim YH, Fisher JM, Choate KA. Revertant mosaicism in genodermatoses. Cell Mol Life Sci. 2017;74(12):2229–38. https://doi.org/10.1007/s00018-017-2468-2.
Pasmooij AM, Garcia M, Escamez MJ, Nijenhuis AM, Azon A, Cuadrado-Corrales N, et al. Revertant mosaicism due to a second-site mutation in COL7A1 in a patient with recessive dystrophic epidermolysis bullosa. J Invest Dermatol. 2010;130(10):2407–11. https://doi.org/10.1038/jid.2010.163.
Gostynski A, Deviaene FC, Pasmooij AM, Pas HH, Jonkman MF. Adhesive stripping to remove epidermis in junctional epidermolysis bullosa for revertant cell therapy. Br J Dermatol. 2009;161(2):444–7. https://doi.org/10.1111/j.1365-2133.2009.09118.x.
Matsumura W, Fujita Y, Shinkuma S, Suzuki S, Yokoshiki S, Goto H, et al. Cultured epidermal autografts from clinically revertant skin as a potential wound treatment for recessive dystrophic epidermolysis bullosa. J Invest Dermatol. 2019;139(10):2115-2124.e11. https://doi.org/10.1016/j.jid.2019.03.1155.
De Rosa L, Carulli S, Cocchiarella F, Quaglino D, Enzo E, Franchini E, et al. Long-term stability and safety of transgenic cultured epidermal stem cells in gene therapy of junctional epidermolysis bullosa. Stem Cell Rep. 2013;2(1):1–8. https://doi.org/10.1016/j.stemcr.2013.11.001.
De Rosa L, Enzo E, Zardi G, Bodemer C, Magnoni C, Schneider H, et al. A phase II/III clinical trial of combined cell and gene therapy of junctional epidermolysis bullosa. Front Genet. 2021;12: 705019. https://doi.org/10.3389/fgene.2021.705019.
Kueckelhaus M, Rothoeft T, De Rosa L, Yeni B, Ohmann T, Maier C, et al. Transgenic epidermal cultures for junctional epidermolysis bullosa: 5-year outcomes. N Engl J Med. 2021;385(24):2264–70. https://doi.org/10.1056/NEJMoa2108544.
Barrandon Y, Green H. Three clonal types of keratinocyte with different capacities for multiplication. Proc Natl Acad Sci USA. 1987;84(8):2302–6. https://doi.org/10.1073/pnas.84.8.2302.
Eichstadt S, Barriga M, Ponakala A, Teng C, Nguyen NT, Siprashvili Z, et al. Phase 1/2a clinical trial of gene-corrected autologous cell therapy for recessive dystrophic epidermolysis bullosa. JCI Insight. 2019;4(19): e130554. https://doi.org/10.1172/jci.insight.130554.
Ito K, Sawamura D, Goto M, Nakamura H, Nishie W, Sakai K, et al. Keratinocyte-/fibroblast-targeted rescue of Col7a1-disrupted mice and generation of an exact dystrophic epidermolysis bullosa model using a human COL7A1 mutation. Am J Pathol. 2009;175(6):2508–17. https://doi.org/10.2353/ajpath.2009.090347.
Supp DM, Hahn JM, Combs KA, McFarland KL, Schwentker A, Boissy RE, et al. Collagen VII expression is required in both keratinocytes and fibroblasts for anchoring fibril formation in bilayer engineered skin substitutes. Cell Transplant. 2019;28(9–10):1242–56. https://doi.org/10.1177/0963689719857657.
Hill JC, Grimwood RE, Parsons DS. Treatment of chronic erosions of junctional epidermolysis bullosa with human epidermal allografts. J Dermatol Surg Oncol. 1992;18(5):396–400. https://doi.org/10.1111/j.1524-4725.1992.tb03692.x.
Kumar AJ, Kim S, Hemmer MT, Arora M, Spellman SR, Pidala JA, et al. Graft-versus-host disease in recipients of male unrelated donor compared with parous female sibling donor transplants. Blood Adv. 2018;2(9):1022–31. https://doi.org/10.1182/bloodadvances.2017013052.
Schofield OMV, Cassella JP, Navsaria HA, Leigh IM, Mayou BJ, Eady RAJ. Cultured keratinocyte allografts in dystrophic epidermolysis bullosa: Preliminary observations. Br J Dermatol. 1990;123: 66–67
Shams F, Rahimpour A, Vahidnezhad H, Hosseinzadeh S, Moravvej H, Kazemi B, et al. The utility of dermal fibroblasts in treatment of skin disorders: a paradigm of recessive dystrophic epidermolysis bullosa. Dermatol Ther. 2021;34(4): e15028. https://doi.org/10.1111/dth.15028.
Rennekampff HO, Kiessig V, Griffey S, Greenleaf G, Hansbrough JF. Acellular human dermis promotes cultured keratinocyte engraftment. J Burn Care Rehabil. 1997;18(6):535–44. https://doi.org/10.1097/00004630-199711000-00012.
Hasegawa T, Suga Y, Mizoguchi M, Ikeda S, Ogawa H, Kubo K, et al. Clinical trial of allogeneic cultured dermal substitute for the treatment of intractable skin ulcers in 3 patients with recessive dystrophic epidermolysis bullosa. J Am Acad Dermatol. 2004;50(5):803–4. https://doi.org/10.1016/j.jaad.2003.08.013.
Moravvej H, Abdollahimajd F, Naseh MH, Piravar Z, Abolhasani E, Mozafari N, et al. Cultured allogeneic fibroblast injection vs. fibroblasts cultured on amniotic membrane scaffold for dystrophic epidermolysis bullosa treatment. Br J Dermatol. 2018;179(1):72–9. https://doi.org/10.1111/bjd.16338.
Sibbald RG, Zuker R, Coutts P, Coelho S, Williamson D, Queen D. Using a dermal skin substitute in the treatment of chronic wounds secondary to recessive dystrophic epidermolysis bullosa: a case series. Ostomy Wound Manage. 2005;51(11):22–46.
Kubo K, Kuroyanagi Y. Spongy matrix of hyaluronic acid and collagen as a cultured dermal substitute: evaluation in an animal test. J Artif Organs. 2003;6(1):64–70. https://doi.org/10.1007/s100470300010.
Niknejad H, Peirovi H, Jorjani M, Ahmadiani A, Ghanavi J, Seifalian AM. Properties of the amniotic membrane for potential use in tissue engineering. Eur Cell Mater. 2008;15:88–99. https://doi.org/10.22203/ecm.v015a07.
Benati D, Miselli F, Cocchiarella F, Patrizi C, Carretero M, Baldassarri S, et al. CRISPR/Cas9-mediated in situ correction of LAMB3 gene in keratinocytes derived from a junctional epidermolysis bullosa patient. Mol Ther. 2018;26(11):2592–603. https://doi.org/10.1016/j.ymthe.2018.07.024.
Bonafont J, Mencía Á, García M, Torres R, Rodríguez S, Carretero M, et al. Clinically relevant correction of recessive dystrophic epidermolysis bullosa by dual sgRNA CRISPR/Cas9-mediated gene editing. Mol Ther. 2019;27(5):986–98. https://doi.org/10.1016/j.ymthe.2019.03.007.
Bonafont J, Mencía A, Chacón-Solano E, Srifa W, Vaidyanathan S, Romano R, et al. Correction of recessive dystrophic epidermolysis bullosa by homology-directed repair-mediated genome editing. Mol Ther. 2021;29(6):2008–18. https://doi.org/10.1016/j.ymthe.2021.02.019.
Izmiryan A, Ganier C, Bovolenta M, Schmitt A, Mavilio F, Hovnanian A. Ex vivo COL7A1 correction for recessive dystrophic epidermolysis bullosa using CRISPR/Cas9 and homology-directed repair. Mol Ther Nucleic Acids. 2018;12:554–67. https://doi.org/10.1016/j.omtn.2018.06.008.
Jacków J, Guo Z, Hansen C, Abaci HE, Doucet YS, Shin JU, et al. CRISPR/Cas9-based targeted genome editing for correction of recessive dystrophic epidermolysis bullosa using iPS cells. Proc Natl Acad Sci USA. 2019;116(52):26846–52. https://doi.org/10.1073/pnas.1907081116.
Kocher T, Bischof J, Haas SA, March OP, Liemberger B, Hainzl S, et al. A non-viral and selection-free COL7A1 HDR approach with improved safety profile for dystrophic epidermolysis bullosa. Mol Ther Nucleic Acids. 2021;25:237–50. https://doi.org/10.1016/j.omtn.2021.05.015.
Betsi EE, Kalbermatten DF, Raffoul W. Surgical management of dystrophic epidermolysis bullosa with autologous composite cultured skin grafts. J Hand Surg Eur. 2009;34(3):398–9. https://doi.org/10.1177/1753193408095879.
Dixit S, Baganizi DR, Sahu R, Dosunmu E, Chaudhari A, Vig K, et al. Immunological challenges associated with artificial skin grafts: available solutions and stem cells in future design of synthetic skin. J Biol Eng. 2017;11:49. https://doi.org/10.1186/s13036-017-0089-9.
Phillips TJ, Manzoor J, Rojas A, Isaacs C, Carson P, Sabolinski M, et al. The longevity of a bilayered skin substitute after application to venous ulcers. Arch Dermatol. 2002;138(8):1079–81. https://doi.org/10.1001/archderm.138.8.1079.
Griffiths M, Ojeh N, Livingstone R, Price R, Navsaria H. Survival of Apligraf in acute human wounds. Tissue Eng. 2004;10(7–8):1180–95. https://doi.org/10.1089/ten.2004.10.1180.
Hu S, Kirsner RS, Falanga V, Phillips T, Eaglstein WH. Evaluation of Apligraf persistence and basement membrane restoration in donor site wounds: a pilot study. Wound Repair Regen. 2006;14(4):427–33. https://doi.org/10.1111/j.1743-6109.2006.00148.x.
Shevchenko RV, James SL, James SE. A review of tissue-engineered skin bioconstructs available for skin reconstruction. J R Soc Interface. 2010;7(43):229–58. https://doi.org/10.1098/rsif.2009.0403.
Boyce ST, Lalley AL. Tissue engineering of skin and regenerative medicine for wound care. Burns Trauma. 2018;6:4. https://doi.org/10.1186/s41038-017-0103-y.
Nita M, Pliszczyński J, Kosieradzki M, Fiedor P. Review of the latest methods of epidermolysis bullosa and other chronic wounds treatment including BIOOPA dressing. Dermatol Ther (Heidelb). 2021;11(5):1469–80. https://doi.org/10.1007/s13555-021-00578-w.
Gurevich I, Agarwal P, Zhang P, Dolorito JA, Oliver S, Liu H, et al. In vivo topical gene therapy for recessive dystrophic epidermolysis bullosa: a phase 1 and 2 trial. Nat Med. 2022;28(4):780–8. https://doi.org/10.1038/s41591-022-01737-y.
Lwin SM, Syed F, Di WL, Kadiyirire T, Liu L, Guy A, et al. Safety and early efficacy outcomes for lentiviral fibroblast gene therapy in recessive dystrophic epidermolysis bullosa. JCI Insight. 2019;4(11): e126243. https://doi.org/10.1172/jci.insight.126243.
Sood R, Roggy DE, Zieger MJ, Nazim M, Hartman BC, Gibbs JT. A comparative study of spray keratinocytes and autologous meshed split-thickness skin graft in the treatment of acute burn injuries. Wounds. 2015;27(2):31–40.
Acknowledgements
We thank Dr. Diana Purvis from Starship Children’s Hospital, Auckland and Rebecca Girvan from the University of Auckland for assisting in the preparation of this article.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this article.
Conflicts of interest/competing interests
The authors declare no competing interests or conflicts of interest in relation to this article. None of Dr Feisst's patents are relevant or included in the manuscript.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
Alex du Rand performed the literature search and wrote the manuscript. Hilary M. Sheppard conceived the topic and critically revised the manuscript and John M. T. Hunt and Vaughan Feisst critically revised the manuscript. The new author (Vaughan Feisst) critically revised the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
du Rand, A., Hunt, J.M.T., Feisst, V. et al. Epidermolysis Bullosa: A Review of the Tissue-Engineered Skin Substitutes Used to Treat Wounds. Mol Diagn Ther 26, 627–643 (2022). https://doi.org/10.1007/s40291-022-00613-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-022-00613-2