Abstract
Objectives
To describe the extrapolation approaches used to support intravenous (IV) golimumab for polyarticular juvenile idiopathic arthritis (pJIA) and juvenile psoriatic arthritis (jPsA) and subcutaneous (SC) ustekinumab for jPsA.
Methods
Pharmacokinetic, clinical response, and safety data from trials of IV golimumab and SC ustekinumab in polyarticular-course JIA (pc-JIA) (GO-VIVA) or pediatric psoriasis (PsO) (CADMUS and CADMUS Jr) and data from pivotal, phase 3 trials of these agents in adults with similar diseases were used to support extrapolation in pJIA and jPsA. In the phase 3 GO-VIVA trial, patients with pc-JIA aged 2 to < 18 years received IV golimumab 80 mg/m2 at weeks 0, 4, then every 8 weeks (Q8W). In the phase 3, randomized, placebo-controlled CADMUS trial, patients with PsO aged ≥ 12 to < 18 years received ustekinumab at weeks 0, 4, then Q12W. In the phase 3 CADMUS Jr trial, patients with PsO aged ≥ 6 to < 12 years received ustekinumab at weeks 0, 4, then Q12W. The ustekinumab analyses used data only from patients who received the standard ustekinumab dosing regimen (≤ 60 kg: 0.75 mg/kg; > 60 to ≤ 100 kg: 45 mg; > 100 kg: 90 mg).
Results
In the 127 patients with pc-JIA treated with IV golimumab (GO-VIVA), pharmacokinetic and exposure-response results were similar to those in adults with rheumatoid arthritis treated with IV golimumab. Additionally, pharmacokinetic and clinical response data from five patients with jPsA in GO-VIVA were comparable to those in adults with PsA treated with IV golimumab. No new safety signals were observed in GO-VIVA. Pharmacokinetic and clinical response data observed in the four pediatric patients with PsO and jPsA treated with ustekinumab in CADMUS and CADMUS Jr were similar to those in the 91 pediatric patients with PsO without jPsA in these trials and to those in adults with PsA treated with ustekinumab. Safety was extrapolated from CADMUS or CADMUS Jr; no new signals were observed.
Conclusions
These three sets of analyses corroborate similar exposure and efficacy of IV golimumab in pediatric patients with pc-JIA or jPsA and SC ustekinumab in patients with jPsA to support extrapolation of established adult efficacy. The overall safety profiles of IV golimumab in pediatric patients with pc-JIA or jPsA and SC ustekinumab in pediatric patients with PsO with or without jPsA were consistent with the safety profiles of these agents in the context of their clinical programs and cumulative use. Based on these analyses, the US Food and Drug Administration approved IV golimumab for polyarticular JIA and active PsA in patients 2 years and older and SC ustekinumab for pediatric PsA in patients 6 years and older, highlighting how use of an extrapolation approach can help streamline drug development for pediatric patient populations in whom larger clinical trials are not feasible.
Clinical Trial Registration
GO-VIVA (NCT02277444) was registered at clinicaltrials.gov on 29 October 2014; CADMUS (NCT01090427) was registered on 22 March 2010; and CADMUS Jr (NCT02698475) was registered on 3 March 2016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pharmacokinetic (PK) exposure and clinical response analyses utilizing observed data from an open-label, phase 3 study in pediatric patients with active polyarticular-course juvenile idiopathic arthritis (pc-JIA) including juvenile psoriatic arthritis (jPsA) corroborated intravenous (IV) golimumab efficacy by extrapolating data from phase 3 randomized controlled trials of IV golimumab in adults with rheumatoid arthritis or PsA. |
The extrapolation analyses described here were used to support the approval in September 2020 of IV golimumab by the US Food and Drug Administration (FDA) for the treatment of polyarticular JIA and active PsA in patients 2 years of age and older. |
Similar PK exposure and clinical response analyses were conducted to support subcutaneous (SC) ustekinumab efficacy in pediatric patients with jPsA observed in phase 3 studies of pediatric psoriasis (PsO), including a subgroup of patients with jPsA, by extrapolating data from pediatric patients with PsO in these studies and from phase 3 randomized controlled trials of ustekinumab in adults with PsO or PsA. These analyses supported FDA approval in July 2022 of SC ustekinumab for the treatment of pediatric PsA in patients 6 years and older. |
1 Introduction
Under the United States (US) Pediatric Research Equity Act (PREA), first passed in 2003, the US Food and Drug Administration (FDA) requires all applications for new treatments to contain an assessment of the product in the relevant pediatric population unless the applicant has obtained a waiver or deferral [1]. Pediatric drug studies pose unique challenges including small patient numbers and ethical restrictions for placebo-controlled trial designs. Extrapolation can address these challenges by utilizing the premise that the diseases and treatment responses are sufficiently similar in the populations being considered [2]. If this can be established, descriptive comparisons between observed pharmacokinetic (PK) and/or model-based exposure data from pediatric patients and data from adults can be conducted to support extrapolation. Exposure-response (ER) and clinical response data can also be compared, typically for a single-dose regimen in pediatric patients with data observed over a range of doses evaluated in adults.
Juvenile idiopathic arthritis (JIA) is an umbrella term encompassing several inflammatory arthritides of unknown etiology with symptom onset prior to 16 years of age and lasting for ≥ 6 weeks [3]. It has an estimated prevalence of 0.04–4 per 1000 children worldwide [4,5,6,7]. Available treatments for JIA include nonsteroidal anti-inflammatory drugs, systemic and intra-articular glucocorticoids, and conventional synthetic and biologic disease-modifying antirheumatic drugs (csDMARDs and bDMARDs, respectively) [4]. Registry data show that 45–52% of patients treated with ≥ two bDMARDs continue to have chronically uncontrolled JIA [8], highlighting the continued unmet need in these patients.
JIA categories were developed to identify clinically distinct groups for research purposes, and do not reflect emerging understanding of the disease [9, 10]; validation of an updated JIA classification system is underway [11]. The current International League of Associations for Rheumatology JIA classification system identifies seven JIA categories: systemic JIA, polyarticular JIA (pJIA) rheumatoid factor (RF)-negative, pJIA RF-positive, oligoarticular (persistent: ≤ four joints; extended: > four joints after the first 6 months of disease), juvenile psoriatic arthritis (jPsA), enthesitis-related arthritis, and undifferentiated arthritis [3]. Polyarticular-course JIA (pc-JIA) affects ≥ five joints cumulatively throughout the course of the disease and can occur within each JIA category. Many of the underlying pathological immune mechanisms that have been identified in rheumatoid arthritis (RA) have also been identified in pJIA (Fig. 1) [5, 6, 8, 10, 12]. Thus, PREA requires that bDMARDs approved for RA also be studied in JIA [8]. Given the relative rarity of JIA and the jPsA JIA subtype (5% of patients with JIA) [13, 14], the FDA previously granted waivers for studies of jPsA following approvals of treatments for adult psoriatic arthritis (PsA).
Relationships among polyarticular JIA, adult RA, adult and juvenile PsA, and adult and pediatric PsO. Vertical purple arrows and solid lines indicate similarity of the pediatric and adult forms of each disease; blue solid and dotted boxes and arrows indicate adjacent pediatric (polyarticular JIA and jPsA) and adult (RA and PsA) diseases; green solid and dotted boxes and arrows indicate adjacent pediatric (jPsA and pediatric PsO) and adult (PsA and PsO) diseases. JIA juvenile idiopathic arthritis, jPsA, juvenile psoriatic arthritis, PsA psoriatic arthritis, PsO psoriasis, RA rheumatoid arthritis
In the context of the aforementioned challenges in pediatric drug development and substantial unmet need in JIA, the use of extrapolation approaches for well-established classes of drugs has been considered, including utilization of open-label PK studies to demonstrate similarity to adult exposures and extrapolation of efficacy and safety observed in adults [15,16,17]. In addition, after a 2019 FDA/Center for Excellence in Regulatory Science and Innovation workshop entitled “Accelerating Drug Development for Polyarticular Juvenile Idiopathic Arthritis (pJIA),” the FDA advised that PREA requirements for pJIA can be addressed with PK studies to support the extrapolation of efficacy data from adults with RA [15, 16]. Subsequently, the FDA advised that, as the underlying mechanisms, comorbidities, and clinical presentations for PsA may overlap with RA and psoriasis (PsO), data from studies conducted in pc-JIA and RA and in pediatric and adult PsO and adult PsA populations can be used to support extrapolation for jPsA without a PK study [18]. The assessment of safety could also be supplemented by results from other relevant pediatric and adult populations.
Here, we describe three sets of analyses that support pediatric extrapolation for the use of two bDMARDs, approved in adult rheumatologic and psoriatic indications (i.e., RA, PsA, and PsO), in similar pediatric indications (i.e., pJIA and jPsA). First, intravenous (IV) golimumab, a tumor necrosis factor-α inhibitor (TNFi) FDA approved for adults with active RA, PsA, or ankylosing spondylitis, was studied for use in pc-JIA. Per FDA request, an initial set of PK exposure and ER analyses was conducted using observed data from an open-label, phase 3 study in pediatric patients with active pc-JIA [19] to determine if extrapolation of data from pivotal, phase 3 studies of IV golimumab in adults with RA was appropriate [20, 21]. As several patients in this study also had jPsA, a second set of analyses assessed data from the jPsA and pc-JIA populations as well as data from adults with PsA [22]. These analyses were the basis of FDA approval of IV golimumab for pJIA and active PsA in patients 2 years of age and older. As a result of these analyses, an extrapolation approach was applied to support the use of ustekinumab for jPsA. Ustekinumab is an interleukin (IL)-12/IL-23 inhibitor that is FDA approved for adults with active PsA, PsO, Crohn’s disease, or ulcerative colitis and for pediatric patients ≥ 6 years of age with moderate-to-severe PsO. This third set of analyses evaluated data from studies of ustekinumab in pediatric patients with PsO, including a small number of patients with PsO and jPsA [23, 24], and in adults with PsA [25]. These analyses were the basis of FDA approval of SC ustekinumab for pediatric PsA in patients 6 years and older.
2 Methods
2.1 Clinical Trials
As detailed in Online Supplemental Material (OSM) Table S1 and OSM Table S2, data employed in these analyses were derived from several clinical trials. Studies of IV golimumab were: (1) GO-VIVA (NCT02277444; phase 3, open-label, PK, efficacy, and safety trial), which evaluated IV golimumab (80 mg/m2 at weeks 0, 4, then every 8 weeks (Q8W)) in 127 patients aged 2 to < 18 years with pc-JIA, including patients with jPsA [19]; (2) GO-FURTHER (NCT00973479; phase 3, randomized, placebo-controlled trial), which evaluated IV golimumab (2 mg/kg at weeks 0, 4, then Q8W) in 592 adults with RA [20]; (3) GO-LIVE (NCT00361335; phase 3, randomized, placebo-controlled trial), which evaluated IV golimumab (2 or 4 mg/kg Q12W) in 643 adults with RA [21]; and (4) GO-VIBRANT (NCT02181673; phase 3, randomized, placebo-controlled trial), which evaluated IV golimumab (2 mg/kg at weeks 0, 4, then Q8W) in 480 adults with PsA [22]. The analyses for IV golimumab utilized data only from patients who received concomitant methotrexate and had available PK samples at the required timepoints.
Ustekinumab trials were: (1) CADMUS (NCT01090427; phase 3, randomized, placebo-controlled), which evaluated ustekinumab (standard or half-standard dosing regimens subcutaneously at weeks 0, 4, then Q12W) in 110 patients ≥ 12 to < 18 years of age with PsO, including patients with jPsA [23]; (2) CADMUS Jr (NCT02698475; phase 3, open-label, PK, efficacy, and safety trial), which evaluated ustekinumab (standard dosing regimen subcutaneously at weeks 0, 4, then Q12W) in 44 patients ≥ 6 to < 12 years of age with PsO, including patients with jPsA [24]; (3) PSUMMIT-1 (NCT01009086) [25] and (4) PSUMMIT-2 (NCT01077362) [26], which were phase 3, randomized, placebo-controlled trials that evaluated ustekinumab (45 or 90 mg subcutaneously at weeks 0, 4, then Q12W for both) in 615 and 312 adults, respectively, with PsA; and (5) PSTELLAR (NCT01550744; phase 3, randomized, controlled trial), which evaluated ustekinumab (45 or 90 mg subcutaneously at weeks 0, 4, 16, then Q12W up to Q24W) in 478 adults with PsO [27]. The analyses for ustekinumab used data only from pediatric patients who received the standard ustekinumab dosing regimen (≤ 60 kg: 0.75 mg/kg; > 60 to ≤ 100 kg: 45 mg; > 100 kg: 90 mg), which demonstrated drug exposure in pediatric patients was comparable to that in adult patients who received ustekinumab 45 mg [23, 24].
All trials included in these analyses were conducted and reported in accordance with the ethical principles originating in the Declaration of Helsinki [28], International Council for Harmonisation (ICH) Good Clinical Practice guidelines [29], and applicable regulatory requirements and in compliance with the respective protocols. Data from relevant dose regimens that were analyzed with the same bioanalytical assays were included to assess the similarity of PK exposure and/or clinical response analyses among the different populations.
2.2 IV Golimumab for Polyarticular JIA
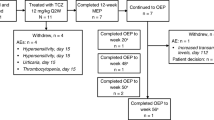
To support IV golimumab for pJIA, PK and ER data observed in 127 children and adolescents with pc-JIA (including all categories of JIA) from the overall GO-VIVA population were descriptively compared with data from adults with RA (GO-FURTHER, GO-LIVE) (Fig. 2a).
Comparisons among a adult RA, pc-JIA, adult PsA, and jPsA clinical trial populations to support extrapolation of IV golimumab data for polyarticular JIA and jPsA and b adolescent PsO, pediatric PsO, adult PsO, adult PsA, and jPsA clinical trial populations to support extrapolation of ustekinumab data for jPsA. *Data from GO-LIVE were used only for comparison of ER analyses. Filled boxes indicate clinical trial(s) dedicated to the patient population indicated. Boxes with black outline indicate clinical trial(s) where the patient population was a subset of the trial(s). The overall GO-VIVA population was used to support IV golimumab for polyarticular JIA. Solid lines and arrows indicate direct comparisons of data. ER exposure-response, IV intravenous, JIA juvenile idiopathic arthritis, jPsA juvenile psoriatic arthritis, pc-JIA polyarticular-course juvenile idiopathic arthritis, PK pharmacokinetics, PsA psoriatic arthritis, PsO psoriasis, RA rheumatoid arthritis, yrs years
2.2.1 Exposure Matching for IV Golimumab for Polyarticular JIA
Median observed steady-state trough golimumab concentrations (Ctrough,ss) and model-predicted, steady-state area under the concentration-time curves (AUCss) over the 8-week golimumab dosing interval at week 28 (overall and by age category) in patients with pc-JIA (GO-VIVA) were compared descriptively with golimumab Ctrough,ss and AUCss assessed at weeks 20 and 36 in adults with RA (GO-FURTHER). Week 20 and week 36 data from GO-FURTHER were used in the absence of a week 28 visit. Model-predicted AUCss was generated from GO-VIVA and GO-FURTHER data using similar population PK models established for pJIA and RA, respectively (see OSM Methods).
2.2.2 Exposure-Response Analyses for IV Golimumab for Polyarticular JIA
The PK exposure metrics underpinning the ER analyses were the observed golimumab Ctrough,ss, calculated average golimumab concentrations at steady state (Cavg,ss), and cumulative AUC. Observed golimumab Ctrough,ss values below the lower limit of quantitation were set to 0. Cavg,ss was calculated as dose/clearance/tau, where tau was the dosing interval. Cumulative AUC was calculated using patient-specific PK parameters and their corresponding dosing and sampling timepoints per the final population PK models. The efficacy endpoints in these ER analyses were the proportions of patients achieving ≥ 20% improvement in the American College of Rheumatology response criteria (ACR20) [30] in GO-FURTHER and GO-LIVE or JIA ACR30 response (≥ 30% improvement from baseline in ≥ three components, without worsening of ≥ 30% in > one of the remaining JIA core measures) in GO-VIVA [31]. While numerically different, the ACR20 and JIA ACR30 responses are similar measures of efficacy in the adult RA and pJIA populations, respectively. The core components of the ACR and JIA ACR scores generally align, noting that the pediatric equivalent of the adult patient’s global assessment of disease activity is the parent/patient assessment of overall well-being [30,31,32]. Patients missing data for all components of the composite endpoint were considered nonresponders (i.e., nonresponder imputation (NRI)). Last observation carried forward was used to impute the composite endpoint when ≥ one of the component values was missing.
Week 20 PK data from GO-VIVA and GO-FURTHER and week 24 PK data from GO-LIVE were descriptively compared as the closest steady-state trough concentrations representing approximately 6 months of exposure because it was hypothesized that efficacy would be similar at these timepoints. Likewise, week 52 efficacy data from GO-VIVA and GO-FURTHER and week 48 efficacy data from GO-LIVE were compared in the same analyses. The proportions of adult RA patients in GO-FURTHER and GO-LIVE achieving ACR20 at weeks 20 and 24, respectively, versus corresponding golimumab Ctrough,ss quartiles were compared with the proportion of pc-JIA patients in GO-VIVA achieving JIA ACR30 at week 20 versus Ctrough,ss quartiles at week 20. Percent changes from baseline in the shared components of the ACR and JIA ACR composite endpoints (i.e., tender joints, swollen joints, patient assessment of disease activity, physician assessment of disease activity, and patient assessment of physical function) [30, 31] from GO-VIVA (at week 20), GO-FURTHER (at week 20), and GO-LIVE (at week 24) versus Ctrough,ss quartiles at these timepoints were also compared.
2.2.3 Safety Analyses for IV Golimumab for Polyarticular JIA
As previously reported, GO-VIVA adverse events (AEs) were monitored through week 52 [19]. Safety data from the overall population in GO-VIVA were evaluated in the context of the established, well-characterized safety profile of IV golimumab in adults with RA or PsA, the extensive safety data that have been collected in clinical trials to support multiple indications [33, 34], and the SC golimumab safety data that have accrued since the first approval in 2009. In company-sponsored interventional trials, > 13,000 individuals have been exposed to IV golimumab, including 1213 adults with RA in GO-FURTHER and GO-LIVE [20, 21], 460 adults with PsA in GO-VIBRANT [22], and 204 adults with ankylosing spondylitis (GO-ALIVE) [35]. The cumulative clinical trial exposure also includes 173 patients with pc-JIA aged 2–17 years who received SC golimumab in the GO-KIDS placebo-controlled, randomized-withdrawal trial [36]. Owing to interstudy variations and differences in sample size and duration of follow-up, safety comparisons focused on the types and patterns of AEs rather than on direct comparisons of AE frequency. An estimated 918,867 patients have been exposed to SC golimumab worldwide cumulatively, and 121,713 patients have been exposed to IV golimumab since approval.
2.3 IV Golimumab for jPsA
The GO-VIVA pc-JIA population included five patients with jPsA [19]. To support extrapolation of IV golimumab for jPsA, PK and clinical response data observed in the five patients with jPsA in GO-VIVA were descriptively compared with data from adults with PsA (GO-VIBRANT) (Fig. 2a).
2.3.1 Exposure Matching for IV Golimumab for jPsA
Golimumab Ctrough,ss at weeks 28 and 52 in patients with jPsA in GO-VIVA were descriptively compared with golimumab Ctrough,ss at weeks 28 and 52 in the overall GO-VIVA population and in the overall population excluding patients with jPsA, and golimumab Ctrough,ss at weeks 36 and 52 in adults with PsA in GO-VIBRANT.
2.3.2 Response Analyses for IV Golimumab for jPsA
For these clinical response analyses, the proportions of patients with jPsA from GO-VIVA who achieved JIA ACR30/50/70/90 (≥ 30, ≥ 50, ≥ 70, and ≥ 90% improvement, respectively, in three components, with no more than one component worsening by > 30, > 50, > 70, and > 90%, respectively) [31] through week 52 were descriptively compared with the proportions of adult PsA patients from GO-VIBRANT who achieved ACR20/50/70/90 responses [30] through week 52. Proportions of JIA ACR and ACR responders were based on imputed data using last observation carried forward for any missing components, and NRI if all components were missing.
2.3.3 Safety Analyses for IV Golimumab for jPsA
Safety was assessed among the five patients with jPsA from GO-VIVA and evaluated in the context of the safety profile of the overall GO-VIVA population and the established IV golimumab and SC golimumab safety profile as described previously (see Sect. 2.2.3).
2.4 Ustekinumab for jPsA
In the CADMUS and CADMUS Jr trials of ustekinumab in adolescents and children, respectively, with PsO, seven patients also had jPsA [23, 24]. Given the availability of these data, and the successful prior extrapolation of adult PsA studies for IV golimumab for jPsA, extrapolation was then planned for ustekinumab in jPsA. To support this extrapolation, data from patients with pediatric PsO alone and from those with PsO and jPsA in CADMUS and CADMUS Jr were descriptively compared with data from adults with PsO (PSTELLAR) or PsA (PSUMMIT-1) (Fig. 2b).
2.4.1 Exposure Matching for Ustekinumab for jPsA
Ustekinumab Ctrough,ss through week 52 in adults with PsO from PSTELLAR were descriptively compared with ustekinumab Ctrough,ss through week 52 in adults with PsA from PSUMMIT-1 among patients who received the 45 mg dose, which is consistent with the standard approved adult dosage for PsA (45 mg at weeks 0, 4, then Q12W). In CADMUS and CADMUS Jr, four of the seven patients with jPsA received the standard dosage. The ustekinumab Ctrough,ss through week 52 in these four patients were compared with the overall population from CADMUS and CADMUS Jr who received the standard adult dosage, with the overall population excluding patients with jPsA, and with adults with PsA from PSUMMIT-1 who received the standard dosage.
2.4.2 Response Analyses for Ustekinumab for jPsA
Response rates for achievement of ≥ 75, ≥ 90, and 100% improvement in Psoriasis Area and Severity Index (PASI) score (PASI75, PASI90, and PASI100, respectively) [37] in patients with jPsA from CADMUS and CADMUS Jr who received the standard adult ustekinumab dosage were descriptively compared with those of adults with PsA from PSUMMIT-1 who received the standard dosage. PASI data from CADMUS and CADMUS Jr were imputed using last observation carried forward or NRI after treatment failure rules were applied (initiated therapies not allowed per protocol or discontinued study drugs due to inadequate efficacy or AE of worsening disease). Response data from PSUMMIT-1 were imputed using NRI after treatment failure rules were applied (initiated therapies not allowed per protocol or discontinued study drugs due to inadequate efficacy or AEs of worsening disease).
Imputed PASI and ACR response data from the adult ustekinumab PsA phase 3 studies (PSUMMIT-1 and PSUMMIT-2) were also pooled to evaluate the similarities of ustekinumab efficacy in PsA by age of disease onset: adult onset (PsA diagnosis ≥18 years of age) or pediatric onset (PsA diagnosis < 18 years of age). For PASI responses, only patients with ≥ 3% baseline body surface area with psoriatic involvement were included. Odds ratios based on Firth logistic regressions were calculated, and the difference in response rates was reported between each ustekinumab dose group (45 and 90 mg) and placebo. Firth logistic regression was used due to the small sample sizes in the pediatric-onset group, with adjustment for PsO and PsA disease durations. To avoid a convergence issue of the model due to partial separation in the pediatric-onset group, PsA disease duration was adjusted using its logarithm as an independent variable. PASI and ACR response rates by age of PsA onset were also visualized by plotting differences in proportions via spydergrams.
2.4.3 Safety Analyses for Ustekinumab for jPsA
Safety for ustekinumab for jPsA was extrapolated from the established safety profile of ustekinumab in the 154 pediatric patients with PsO in CADMUS and CADMUS Jr, including seven patients who had PsO and jPsA [23, 24]. As previously reported, AEs were monitored through weeks 60 and 56, respectively, in these trials. Extensive safety data have also been collected in ustekinumab clinical trials for multiple indications in adults and pediatric patients [38]. In company-sponsored interventional studies, 12,228 participants have been exposed to ustekinumab, including 5750 adult and pediatric participants with PsO and 1045 adult participants with PsA. Ustekinumab clinical trial exposure also includes 44 pediatric patients with Crohn’s disease aged, 2 to <18 years, who received ustekinumab in a randomized, dose-ranging study [39]. As with IV golimumab, ustekinumab safety comparisons focused on the types and patterns of AEs rather than on direct comparisons of AE frequency due to differences in study populations and designs.
3 Results
3.1 IV Golimumab for Polyarticular JIA
3.1.1 PK Matching for IV Golimumab for Polyarticular JIA
The PK analysis set for patients with pc-JIA included 127 patients who received ≥ one golimumab infusion in GO-VIVA and had sufficient PK samples for analysis. Golimumab PK exposures (Ctrough,ss and AUCss) at week 28 in these pediatric patients were similar across pediatric age categories (Fig. 3). Median Ctrough,ss at week 28 in pediatric patients with pc-JIA (range 0.31–0.48 µg/mL) were similar to those at weeks 20 (0.21 µg/mL) and 36 (0.31 µg/mL) in adults with RA who received ≥ one IV golimumab infusion in GO-FURTHER (Fig. 3a). Model-predicted AUCss at week 28 in patients with pc-JIA (range 387–424 µg·day/mL) was 50–64% higher than AUCss in adults with RA (248 µg·day/mL) (Fig. 3b).
Exposure matching for IV golimumab for polyarticular JIA a observed Ctrough,ss golimumab concentrations in patients with pc-JIA (GO-VIVA) at week 28 and adults with RA (GO-FURTHER) at weeks 20 and 36, and b model-predicted serum golimumab AUCss over an 8-week dosing interval at week 28 in patients with pc-JIA (GO-VIVA) and adults with RA (GO-FURTHER). Horizontal line within box = median; lower edge of box = first quartile; upper edge of box = third quartile; ends of whiskers represent ± 1.5 \(\times\) IQR. AUCss steady-state area under the concentration-time curve, Ctrough,ss steady-state trough concentration, IQR interquartile range, IV intravenous, JIA juvenile idiopathic arthritis, pc-JIA polyarticular-course juvenile idiopathic arthritis, RA rheumatoid arthritis
3.1.2 Exposure-Response for IV Golimumab for Polyarticular JIA
Week 20 JIA ACR30 response rates among pc-JIA patients in GO-VIVA were greater than ACR20 response rates at week 20 in GO-FURTHER (adults with RA) and at week 24 in GO-LIVE (adults with RA), across serum golimumab Ctrough,ss in adults (Fig. 4a). In addition, median improvements in JIA ACR and ACR component scores (i.e., tender joints, swollen joints, patient assessment of disease activity, physician assessment of disease activity, and patient assessment of physical function) at these timepoints were similar or greater in patients with pc-JIA versus adults with RA, regardless of Ctrough,ss in adults (Fig. 4b–f). Results were consistent when efficacy was evaluated by Cavg,ss and cumulative AUC (data not shown), although PK exposures were slightly higher in pediatric patients with pc-JIA versus adults with RA.
Efficacy responses by golimumab steady-state trough concentration quartiles in adults with RA from GO-FURTHER (week 20) and GO-LIVE (week 24) and pediatric patients with pc-JIA from GO-VIVA (week 20) a ACR20 and JIA ACR30 response rates, and percent change from baseline in b tender joint count, c swollen joint count, d patient assessment of disease activity, e physician assessment of disease activity, and f patient assessment of physical function. Circle within box = median; lower edge of box = first quartile; upper edge of box = third quartile; ends of whiskers represent ± 1.5 × IQR. ACR20 ≥ 20% improvement from baseline in tender and swollen joint counts and ≥ 20% improvement in three of the five other core set measures. JIA ACR30 = ≥ 30% improvement from baseline in three components, without worsening of ≥ 30% in > one of the remaining JIA core measures. Patients missing data for all components of the composite endpoint were considered nonresponders. Last observation carried forward was used to impute the composite endpoint when ≥ one of the component values was missing. ACR American College of Rheumatology, Ctrough,ss steady-state trough concentration, JIA juvenile idiopathic arthritis, pc-JIA polyarticular-course juvenile idiopathic arthritis, Q quartile, RA rheumatoid arthritis
3.1.3 Safety for IV Golimumab for Polyarticular JIA
Detailed safety results through 1 year of IV golimumab treatment in GO-VIVA have been previously reported [19]. Briefly, through 1 year, 85% of pediatric patients with pc-JIA experienced ≥ one AE, with infections being the most common type; 7% experienced ≥ one serious AE, 65% experienced ≥ one infection, and 6% experienced ≥ one serious infection, including one patient with a serious opportunistic infection. The most commonly reported AEs were upper respiratory tract infection (21%) and nasopharyngitis (18%). Serious AEs were disseminated herpes zoster, infective exacerbation of bronchiectasis, sepsis, varicella, mycosis fungoides, suicidal ideation, cellulitis, pneumonia, streptococcal pneumonia, and pleural effusion (streptococcal pneumonia and pleural effusion were reported in the same patient). Mild, new-onset, anterior uveitis in both eyes was reported in one patient but did not require treatment. No cases of active tuberculosis, demyelination events, or anaphylactic or serum sickness reactions were reported. Systemic lupus erythematosus was reported in one patient, but was considered nonserious. No deaths were reported through week 52, but one death due to septic shock (likely due to constipation leading to bacterial translocation through the gut wall) was reported at week 78 (last IV golimumab dose at week 76) in this ongoing study.
Comparison of safety data from GO-VIVA to the established safety profile for golimumab from studies conducted in adults did not identify any new AEs. In addition, the types of AEs observed in GO-VIVA through week 52 were comparable to those observed with IV golimumab in adults with rheumatic disease [20,21,22, 35] and with SC golimumab in patients with pc-JIA [36]. Furthermore, no new safety concerns were identified relative to the safety profile observed across the TNFi class in either adult or pediatric indications [40,41,42,43].
3.2 IV Golimumab for jPsA
3.2.1 PK Matching for IV Golimumab for jPsA
Among the five patients with pc-JIA in GO-VIVA with jPsA, four had evaluable PK samples at weeks 28 and 52 and were included in the PK analysis set. The observed serum golimumab Ctrough,ss values were similar among patients with jPsA, pc-JIA (excluding jPsA), and pc-JIA (overall) at weeks 28 and 52 (Fig. 5a). In addition, golimumab Ctrough,ss at week 28 in patients with jPsA was similar to Ctrough,ss at week 36 in adults with PsA from GO-VIBRANT with overlapping steady-state trough serum golimumab concentration ranges (Fig. 5b). Similar results were observed at week 52.
Exposure matching for IV golimumab for jPsA. a Observed steady-state serum trough golimumab concentrations in patients from GO-VIVA with jPsA, pc-JIA (excluding jPsA), and pc-JIA (overall) at weeks 28 and 52, and b observed steady-state serum trough golimumab concentrations in patients with jPsA (GO-VIVA) and adults with PsA (GO-VIBRANT) at weeks 28 (jPsA), 36 (adult PsA), and 52 (both populations). *pc-JIA population excluding patients with jPsA. †Week 28 for jPsA and week 36 for adult PsA. Horizontal line within box = median; lower edge of box = first quartile; upper edge of box = third quartile; whiskers represent fifth and 95th percentiles. Ctrough,ss steady-state trough concentration, IV intravenous, jPsA juvenile psoriatic arthritis, pc-JIA polyarticular-course juvenile idiopathic arthritis, PsA psoriatic arthritis, W week
3.2.2 Response Analyses for IV Golimumab for jPsA
The proportions of patients with jPsA achieving JIA ACR30 responses through week 52 were consistent with the proportions of adults with PsA achieving ACR20 through week 52 (Fig. 6a). Efficacy as assessed by JIA ACR50/70/90 and ACR50/70/90 response rates was consistently seen in both pediatric and adult patients, respectively, through week 52 (Fig. 6b–d).
Clinical response rates among patients with jPsA (GO-VIVA) and adults with PsA (GO-VIBRANT) through week 52 a JIA ACR30 versus ACR20, b JIA ACR50 versus ACR50, c JIA ACR70 versus ACR70, and d JIA ACR90 versus ACR90. Adult PsA population included only adults with baseline methotrexate use. Proportions of JIA ACR and ACR responders are based on imputed data using last observation carried forward and nonresponder imputation. ACR20/50/70/90 = ≥ 20%/50%/70%/90% improvement from baseline in ACR criteria. JIA ACR30/50/70/90 = ≥ 30%/50%/70%/90% improvement from baseline in three components, without worsening of ≥ 30%/50%/70%/90% in > one of the remaining JIA core measures. ACR American College of Rheumatology, JIA juvenile idiopathic arthritis, jPsA juvenile psoriatic arthritis, PsA psoriatic arthritis
3.2.3 Safety for IV Golimumab for jPsA
The AEs observed in the five patients with jPsA who received IV golimumab in GO-VIVA were similar to those in the overall GO-VIVA population and to those in adults with PsA in GO-VIBRANT. Seven AEs occurred in four patients with jPsA through week 52 (pyoderma, gastroenteritis, nausea, upper respiratory tract infection, increased blood pressure, furuncle, and double-stranded DNA antibody positive). No serious AEs were reported. All AEs were singular events, and none resulted in discontinuation of golimumab. Furthermore, the overall safety profile of IV golimumab in patients with pc-JIA in GO-VIVA, which included patients with jPsA, was consistent with the safety profile of SC golimumab in patients with pc-JIA in GO-KIDS, which also included patients with jPsA [36].
3.3 Ustekinumab for jPsA
3.3.1 PK Matching for Ustekinumab for jPsA
The PK analysis set for ustekinumab in jPsA included four pediatric patients with PsO and jPsA and 91 pediatric patients with PsO without jPsA who received standard ustekinumab dosing in CADMUS and CADMUS Jr. Serum ustekinumab concentrations over time were comparable in adults with PsO (PSTELLAR) and adults with PsA (PSUMMIT-1) who received similar ustekinumab dosages, suggesting that extrapolating data between PsO and PsA is feasible (Fig. 7a). Serum ustekinumab concentrations over time were also comparable between pediatric patients with PsO with or without jPsA (CADMUS and CADMUS Jr) who received similar ustekinumab dosages, confirming that extrapolation between these pediatric patient populations was appropriate (Fig. 7b). In addition, PK exposures over time were comparable between pediatric patients with PsO with and without jPsA (CADMUS and CADMUS Jr) and adults with PsA (PSUMMIT-1), supporting the conclusion that extrapolation between these patient groups is appropriate.
Observed serum ustekinumab Ctrough,ss through week 52 in a adults with PsO (PSTELLAR) or PsA (PSUMMIT-1) and b adults with PsA (PSUMMIT-1) and pediatric patients with PsO with or without jPsA (CADMUS and CADMUS Jr). Horizontal line within box = median; diamond = mean; lower edge of box = first quartile; upper edge of box = third quartile; ends of whiskers represent ±1.5 × IQR. Adult PsO and PsA populations included only adults who received the ustekinumab 45 mg dose regimen. Pediatric PsO with or without jPsA populations included only pediatric patients assigned to the standard dose treatment group and who received the standard dose regimen at 0.75 mg/kg or 45 mg. Ctrough,ss steady-state trough concentration, jPsA juvenile psoriatic arthritis, PsA psoriatic arthritis, PsO psoriasis, w/o without
3.3.2 Response Analyses for Ustekinumab for jPsA
PASI75 response rates in four pediatric patients with PsO and jPsA who received ustekinumab standard dosing were comparable with those in adults with PsA (PSUMMIT-1) (Fig. 8). PASI90 and PASI100 response rates were generally similar between the patient populations (OSM Fig. S1a–b).
PASI75 response rates through week 52 in pediatric patients with PsO and jPsA (CADMUS and CADMUS Jr) and in adults with PsA (PSUMMIT-1). Pediatric patients with PsO and jPsA (CADMUS and CADMUS Jr) included patients in the randomized set (CADMUS) or full analysis set (CADMUS Jr) assigned to the standard dose regimen (0.75 mg/kg or 45 mg). Data for this population were imputed using last observation carried forward or nonresponder imputation after treatment failure rules were applied. Adults with PsA (PSUMMIT-1) included patients in the randomized set as per study protocol who received ustekinumab 45 mg. In this population, PASI response was evaluated only in patients with ≥ 3% of body surface area affected by PsO at baseline, and data were imputed using nonresponder imputation on PASI response parameters after treatment failure rules were applied. Treatment failure rules for all studies were initiation of therapies not allowed per protocol or discontinuation of study drugs due to inadequate efficacy or adverse event of worsening disease. PASI75 = ≥ 75% improvement from baseline in PASI score. jPsA juvenile psoriatic arthritis, NE not evaluated, PASI Psoriasis Area and Severity Index, PsA psoriatic arthritis, PsO psoriasis
PASI and ACR response rates were similar between adults with PsA from PSUMMIT-1 and PSUMMIT-2 who were diagnosed with PsA at < 18 years of age (pediatric onset of PsA) versus > 18 years of age (adult onset of PsA) when adjusted by PsO (OSM Fig. S2a) or PsA (OSM Fig. S2b) disease duration. Although wider confidence intervals were observed in the pediatric-onset group due to a small sample size, odds ratios for PASI and ACR responses for ustekinumab versus placebo were similar between the pediatric and adult-onset groups. When analyzed as a spydergram, adult and pediatric responses mirrored each other, with wider confidence intervals again observed in the pediatric-onset group due to the small sample size (OSM Fig. S2c).
3.3.3 Safety for Ustekinumab for jPsA
Through 1 year, no new safety signals were observed in the 154 pediatric patients with PsO treated with ustekinumab in CADMUS and CADMUS Jr [23, 24]. Nasopharyngitis, pharyngitis, and upper respiratory tract infection were among the most commonly reported AEs in both studies. Tonsillitis, gastroenteritis, and otitis media occurred more frequently in CADMUS Jr; however, these events are known to be more commonly reported in younger patients [44,45,46] and do not appear to represent newly identified safety concerns in this younger population. The incidence and types of AEs in the CADMUS Jr long-term extension were also consistent with those in the main study. In addition, the overall safety profile of ustekinumab in CADMUS and CADMUS Jr was consistent with the safety profile of ustekinumab in pivotal clinical trials of adult PsO and adult PsA [38].
In addition, no new safety signals were observed in the seven patients with PsO and jPsA who received standard or half-standard ustekinumab dosing in CADMUS or CADMUS Jr, which was not surprising given the small number of patients with PsO and jPsA. Six of these seven patients reported ≥ 1 AE, and none reported serious AEs. The similarity in safety profiles between pediatric PsO and jPsA is supported by the comparable safety profiles observed in phase 3 clinical trials in adults with PsO [47, 48] and adults with PsA who received similar ustekinumab dose regimens [25, 26]. In these studies, there was no clear ustekinumab dose-response relationship in AEs or difference in safety profiles between patients who did or did not receive concomitant methotrexate.
While postmarketing safety data for ustekinumab in pediatric patients with PsO are limited, no safety concerns have been identified to date in patients aged ≥ 6 to < 18 years who received ustekinumab, and the safety profile is similar to that observed for ustekinumab in the adult population.
4 Discussion
With the advent of PREA, in the absence of a waiver, products for which an application is being made to the FDA require pediatric studies. Though this requirement benefits pediatric patients, such studies are fraught with difficulties. Extrapolation provides an elegant solution to address practicalities (such as small sample size) and ethical challenges (including pediatric patients with a progressive disease receiving a placebo) that are barriers to conducting pediatric clinical trials. Indeed, these were the barriers faced when considering IV golimumab for pJIA and jPsA and SC ustekinumab for jPsA.
With a completed IV golimumab PK, efficacy, and safety study in patients with pc-JIA, including jPsA, data in pediatric patients and knowledge about PK exposure, efficacy, and safety were determined by the FDA to be adequate to support extrapolation. IV golimumab PK, efficacy, and safety data in adults with RA or PsA were also determined by the FDA to be suitable for extrapolation to patients with pc-JIA, including pJIA and active PsA. Similarly, with two completed ustekinumab pediatric PsO trials, including patients with jPsA, as well as one completed pediatric Crohn’s disease trial, data in pediatric patients and knowledge about PK exposure, efficacy, and safety were determined by the FDA to be adequate to support extrapolation without enrolling any children into a pediatric PsA-specific clinical trial. Ustekinumab data in adults with PsO or PsA were also determined by the FDA to be adequate for extrapolation to patients with pediatric PsA.
The extrapolation of the robust efficacy demonstrated by the well-controlled clinical trials in adults is supported by known clinical similarities between (1) pJIA and adult RA; (2) jPsA and adult PsA; and (3) pediatric and adult PsO (Fig. 1). The results of the analyses conducted, including overlapping golimumab and ustekinumab PK exposures and consistent efficacy between pediatric and adult patients, further support extrapolation. Although model-predicted AUCss in patients with pc-JIA was substantially higher than AUCss in adults with RA, the differences were within the wide range of expected variability that has been observed with monoclonal antibodies [49,50,51]. In the context of this moderate to high variability, it can be concluded that the PK data are similar enough to support extrapolation.
Similarly, the safety profiles of IV golimumab and SC ustekinumab in pediatric patients were consistent with the safety profiles of these drugs in adult patients with RA, PsO, or PsA. There were no new safety signals in the clinical studies of pediatric patients with pc-JIA [19] or PsO with or without jPsA [23, 24] treated with IV golimumab or SC ustekinumab, respectively. In addition, as expected due to the small patient numbers, no new signals were observed in pediatric patients with jPsA treated with either drug.
The number of pediatric patients was small, particularly for the jPsA analyses for both compounds, making true differences between populations difficult to discern due to the inherent uncertainty. However, as noted in the recently published (April 2022) ICH guidelines for pediatric extrapolation [2], clinical judgment should be utilized to establish the tolerable level of uncertainty associated with the data supporting extrapolation to a target pediatric population. The overlapping serum steady-state drug concentrations over time corroborated similarity of PK exposure and consistent response patterns for pediatric and adult populations. Notably, for jPsA, these analyses of PK data from adjacent, closely related diseases helped to address uncertainty and to support extrapolation of safety and efficacy from the results of pediatric PsO, adult PsO, and adult PsA pivotal trials without the need for trials dedicated to jPsA, which are difficult to conduct due to the rarity of this category of JIA [13, 14]. In addition, the totality of comparable results between these populations supports a favorable benefit-risk profile for IV golimumab and SC ustekinumab in pediatric patients with pJIA and/or jPsA.
5 Conclusions
Altogether, overlapping clinical presentations across disease states, comparable PK exposure and clinical response, and consistent safety profiles between pediatric patients and adults support extrapolation of the robust efficacy of IV golimumab and SC ustekinumab demonstrated in well-controlled clinical trials in adults to pediatric patients. Based on these analyses, the FDA approved IV golimumab for pJIA and active PsA in patients 2 years and older in September 2020, and SC ustekinumab for pediatric PsA in patients 6 years and older in July 2022. These results highlight how use of exposure matching and clinical response analyses can help streamline drug development for pediatric patient populations in whom larger clinical trials are not feasible.
References
Pediatric Research Equity Act (PREA). 2003:Pub L No. 108-55.
International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use. ICH E11A: Pediatric extrapolation. April 4, 2022. Available at: https://database.ich.org/sites/default/files/ICH_E11A_Document_Step2_Guideline_2022_0404_0.pdf. Accessed 6 Apr 2022.
Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, He X, Maldonado-Cocco J, Orozco-Alcala J, Prieur AM, Suarez-Almazor ME, Woo P, International League of Associations for Rheumatology. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31:390–2.
Ringold S, Angeles-Han ST, Beukelman T, Lovell DJ, Cuello CA, Becker ML, Colbert RA, Feldman BM, Ferguson PJ, Gewanter HL, Guzman J, Horonjeff J, Nigrovic PA, Ombrello M, Passo M, Stoll ML, Rabinovich CE, Schneider R, Halyabar O, Hays K, Shah AA, Sullivan N, Szymanski AM, Turgunbaev M, Turner A, Reston J. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the treatment of juvenile idiopathic arthritis: therapeutic approaches for non-systemic polyarthritis, sacroiliitis, and enthesitis. Arthritis Rheumatol. 2019;71:846–63. https://doi.org/10.1002/art.40884.
European Medicines Agency. Guideline on clinical investigation of medicinal products for the treatment of juvenile idiopathic arthritis. EMA/CHMP/239770/2014 Rev 2. November 19, 2015. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-clinical-investigation-medicinal-products-treatment-juvenile-idiopathic-arthritis_en.pdf. Accessed 29 Mar 2022.
Prakken B, Albani S, Martini A. Juvenile idiopathic arthritis. Lancet. 2011;377:2138–49.
Thierry S, Fautrel B, Lemelle I, Guillemin F. Prevalence and incidence of juvenile idiopathic arthritis: a systematic review. Jt Bone Spine. 2014;81:112–7.
Brunner HI, Schanberg LE, Kimura Y, Dennos A, Co DO, Colbert RA, Fuhlbrigge R, Goldmuntz E, Kingsbury DJ, Patty-Resk C, Mintz S, Onel K, Rider LG, Schneider R, Watts A, von Scheven E, Lovell DJ, Beukelman T, PRCSG Advisory Council and the CARRA Registry Investigators. New medications are needed for children with juvenile idiopathic arthritis. Arthritis Rheumatol. 2020;72:1945–51. https://doi.org/10.1002/art.41390.
Aggarwal R, Ringold S, Khanna D, Neogi T, Johnson SR, Miller A, Brunner HI, Ogawa R, Felson D, Ogdie A, Aletaha D, Feldman BM. Distinctions between diagnostic and classification criteria? Arthritis Care Res (Hoboken). 2015;67:891–7.
Nigrovic PA, Colbert RA, Holers VM, Ozen S, Ruperto N, Thompson SD, Wedderburn LR, Yeung RSM, Martini A. Biological classification of childhood arthritis: roadmap to a molecular nomenclature. Nat Rev. 2021;17:257–69.
Martini A, Ravelli A, Avcin T, Beresford MW, Burgos-Vargas R, Cuttica R, Ilowite NT, Khubchandani R, Laxer RM, Lovell DJ, Petty RE, Wallace CA, Wulffraat NM, Pistorio A, Ruperto N, for the Pediatric Rheumatology International Trials Organization (PRINTO). Toward new classification criteria for juvenile idiopathic arthritis: first steps, pediatric rheumatology international trials organization international consensus. J Rheumatol. 2019;46:190–7.
Stefanska AM, Distlerová D, Musaus J, Olski TM, Dunder K, Salmonson T, Mentzer D, Müller-Berghaus J, Hemmings R, Veselý R. Extrapolation in the development of paediatric medicines: examples from approvals for biological treatments for paediatric chronic immune-mediated inflammatory diseases. Arch Dis Child. 2017;102:952–7.
Stoll ML, Punaro M. Psoriatic juvenile idiopathic arthritis: a tale of two subgroups. Curr Opin Rheumatol. 2011;23:437–43.
Zisman D, Stoll ML, Butbul Aviel Y, Mellins ED. Juvenile psoriatic arthritis: a report from the GRAPPA 2017 annual meeting. J Rheumatol Suppl. 2018;94:11–6.
United States Food and Drug Administration. Accelerating drug development for polyarticular juvenile idiopathic arthritis (pJIA). October 2, 2019. https://www.fda.gov/news-events/fda-meetings-conferences-and-workshops/accelerating-drug-development-polyarticular-juvenile-idiopathic-arthritis-pjia-10022019-10022019. Accessed 16 Mar 2022.
Singh R, Ivaturi VD, Penzenstadler J, Liu T, Chen J, Marathe A, Ji P, Glaser R, Nikolov N, Sahajwalla C. Response similarity assessment between polyarticular juvenile idiopathic arthritis and adult rheumatoid arthritis for biologics. Clin Pharm Ther. 2021;110:98–107.
Ruperto N, Brunner HI, Lovell DJ, Martini A, for the Paediatric Rheumatology International Trials Organisation (PRINTO) and the Pediatric Rheumatology Collaborative Study Group (PRCSG). Extrapolation or controlled trials in paediatrics: the current dilemma. Arch Dis Child. 2017;102:949–51.
United States Food and Drug Administration. NDA/BLA multi-disciplinary review and evaluation, BLA 25433, Supplement 30, IV golimumab (Simponi Aria) for pJIA. October 12, 2018. https://www.fda.gov/media/143318/download. Accessed 18 July 2022.
Ruperto N, Brunner HI, Pacheco-Tena C, Louw I, Vega-Cornejo G, Spindler AJ, Kingsbury DJ, Schmeling H, Borzutzky A, Cuttica R, Inman CJ, Malievskiy V, Scott C, Keltsev V, Terreri MT, Viola DO, Xavier RM, Pedrosa Fernandes TA, del Rocío Maldonado Velázquez M, Henrickson M, Clark MB, Bensley KA, Li X, Lo KH, Leu JH, Hsu C-H, Hsia EC, Xu Z, Martini A, Lovell DJ, for the Pediatric Rheumatology Collaborative Study Group (PRCSG) and the Paediatric Rheumatology International Trials Organisation (PRINTO). Open-label phase 3 study of intravenous golimumab in patients with polyarticular juvenile idiopathic arthritis. Rheumatology. 2021;60:4495–507.
Weinblatt ME, Bingham CO III, Mendelsohn AM, Kim L, Mack M, Lu J, Baker D, Westhovens R. Intravenous golimumab is effective in patients with active rheumatoid arthritis despite methotrexate therapy with responses as early as week 2: results of the phase 3, randomised, multicentre, double-blind, placebo-controlled GO-FURTHER trial. Ann Rheum Dis. 2013;72:381–9.
Kremer J, Ritchlin C, Mendelsohn A, Baker D, Kim L, Xu Z, Han J, Taylor P. Golimumab, a new human anti-tumor necrosis factor α antibody, administered intravenously in patients with active rheumatoid arthritis: forty-eight-week efficacy and safety results of a phase III randomized, double-blind, placebo-controlled study. Arthritis Rheum. 2010;62:917–28.
Kavanaugh A, Husni ME, Harrison DD, Kim L, Lo KH, Leu JH, Hsia EC. Safety and efficacy of intravenous golimumab in patients with active psoriatic arthritis. Arthritis Rheumatol. 2017;69:2151–61.
Landells I, Marano C, Hsu M-C, Li S, Zhu Y, Eichenfield LF, Hoeger PH, Menter A, Paller AS, Taieb A, Philipp S, Szapary P, Randazzo B. Ustekinumab in adolescent patients age 12 to 17 years with moderate-to-severe plaque psoriasis: results of the randomized phase 3 CADMUS study. J Am Acad Dermatol. 2015;73:594–603.
Philipp S, Menter A, Nikkels AF, Barber K, Landells I, Eichenfield LF, Song M, Randazzo B, Li S, Hsu M-C, Zhu Y, DePrimo S, Paller AS. Ustekinumab for the treatment of moderate-to-severe plaque psoriasis in paediatric patients (≥6 to <12 years of age): efficacy, safety, pharmacokinetic and biomarker results from the open-label CADMUS Jr study. Br J Dermatol. 2020;183:664–72.
McInnes IB, Kavanaugh A, Gottlieb AB, Puig L, Rahman P, Ritchlin C, Brodmerkel C, Li S, Wang Y, Mendelsohn AM, Doyle MK, on behalf of the PSUMMIT 1 Study Group. Efficacy and safety of ustekinumab in patients with active psoriatic arthritis: 1 year results of the phase 3, multicentre, double-blind, placebo-controlled PSUMMIT 1 trial. Lancet. 2013;382:780–9.
Ritchlin C, Rahman P, Kavanaugh A, McInnes IB, Puig L, Li S, Wang Y, Shen Y-K, Doyle MK, Mendelsohn AM, Gottlieb AB, on behalf of the PSUMMIT 2 Study Group. Efficacy and safety of the anti-IL-12/23 p40 monoclonal antibody, ustekinumab, in patients with active psoriatic arthritis despite conventional non-biological and biological anti-tumour necrosis factor therapy: 6-month and 1-year results of the phase 3, multicentre, double-blind, placebo-controlled, randomised PSUMMIT 2 trial. Ann Rheum Dis. 2014;73:990–9.
Blauvelt A, Ferris LK, Yamauchi PS, Qureshi A, Leonardi CL, Farahi K, Fakharzadeh S, Hsu MC, Li S, Chevrier M, Smith K, Goyal K, Chen Y, Muñoz-Elías EJ, Callis DK. Extension of ustekinumab maintenance dosing interval in moderate-to-severe psoriasis: results of a phase IIIb, randomized, double-blinded, active-controlled, multicentre study (PSTELLAR). Br J Dermatol. 2017;177:1552–61.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Med Assoc. 2013;310:2191–4.
International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use. Integrated addendum to ICH E6(R1): guideline for Good Clinical Practice E6(R2). 2016. Available at: https://database.ich.org/sites/default/files/E6_R2_Addendum.pdf. Accessed 16 Mar 2022.
Felson DT, Anderson JJ, Boers M, Bombardier C, Furst D, Goldsmith C, Katz LM, Lightfoot R Jr, Paulus H, Strand V, Tugwell P, Weinblatt M, Williams HJ, Wolfe F, Kieszak S. American College of Rheumatology preliminary definition of improvement in rheumatoid arthritis. Arthritis Rheum. 1995;38(6):727–35.
Giannini EH, Ruperto N, Ravelli A, Lovell DJ, Felson DT, Martini A. Preliminary definition of improvement in juvenile arthritis. Arthritis Rheumatol. 1997;40:1202–9.
Oliveira-Ramos F, Eusébio M, Martins FM, Mourão AF, Furtado C, Campanilho-Marques R, Cordeiro I, Ferreira J, Cerqueira M, Figueira R, Brito I, Canhão H, Santos MJ, Melo-Gomes JA, Fonseca JE. Juvenile idiopathic arthritis in adulthood: fulfilment of classification criteria for adult rheumatic diseases, long-term outcomes and predictors of inactive disease, functional status and damage. RMD Open. 2016;2(2): e000304.
Simponi Aria (golimumab injection, for intravenous use). Package insert. Horsham: Janssen Biotech, Inc.; 2021.
Simponi (golimumab for injection). Package insert. Horsham: Janssen Biotech, Inc.; 2019.
Deodhar A, Reveille JD, Harrison DD, Kim L, Lo KH, Leu JH, Hsia EC. Safety and efficacy of golimumab administered intravenously in adults with ankylosing spondylitis: results through week 28 of the GO-ALIVE study. J Rheumatol. 2018;45:341–8 (Erratum in: J Rheumatol. 2018;45:291).
Brunner HI, Ruperto N, Tzaribachev N, Horneff G, Chasnyk VG, Panaviene V, Abud-Mendoza C, Reiff A, Alexeeva E, Rubio-Pérez N, Keltsev V, Kingsbury DJ, del Rocio Maldonado Velázquez M, Nikishina I, Silverman ED, Joos R, Smolewska E, Bandeira M, Minden K, van Royen-Kerkhof A, Emminger W, Foeldvari I, Lauwerys BR, Sztajnbok F, Gilmer KE, Xu Z, Leu JH, Kim L, Lamberth SL, Loza MJ, Lovell DJ, Martini A. Subcutaneous golimumab for children with active polyarticular-course juvenile idiopathic arthritis: results of a multicentre, double-blind, randomised-withdrawal trial. Ann Rheum Dis. 2018;77:21–9.
Fredriksson T, Pettersson U. Severe psoriasis—oral therapy with a new retinoid. Dermatologica. 1978;157:238–44.
Stelara (ustekinumab). Package insert. Horsham: Janssen Biotech, Inc.; 2020.
Rosh JR, Turner D, Griffiths A, Cohen SA, Jacobstein D, Adedokun OJ, Padgett L, Terry NA, O’Brien C, Hyams JS. Ustekinumab in paediatric patients with moderately to severely active Crohn’s disease: pharmacokinetics, safety, and efficacy results from UniStar, a phase 1 study. J Crohn’s Colitis. 2021;15:1931–42.
Humira (adalimumab). Package insert. North Chicago: AbbVie Inc.; 2021.
Enbrel (etanercept). Package insert. Thousand Oaks: Immunex Corporation; 2021.
Remicade (infliximab). Package insert. Horsham: Janssen Biotech, Inc.; 2021.
Cimzia (certolizumab pegol). Package insert. Smyrna: UCB, Inc.; 2019.
Daly KA, Giebink GS. Clinical epidemiology of otitis media. Pediatr Infect Dis J. 2000;19:S31–6.
De Wit MAS, Koopmans MPG, Kortbeek LM, Wannet WJ, Vinjé J, van Leusden F, Bartelds AIM, van Duynhoven YTHP. Sensor, a population-based cohort study on gastroenteritis in the Netherlands: incidence and etiology. Am J Epidemiol. 2001;154:666–74.
Windfuhr JP, Toepfner N, Steffen G, Walsfahrer F, Berner R. Clinical practice guideline: tonsillitis I. Diagnostics and nonsurgical management. Eur Arch Otorhinolaryngol. 2016;273:973–87.
Leonardi CL, Kimball AB, Papp KA, Yeilding N, Guzzo C, Wang Y, Li S, Dooley LT, Gordon KB, PHOENIX 1 study investigators. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 1). Lancet. 2008;371:1665–74.
Papp KA, Langley RG, Lebwohl M, Krueger GG, Szapary P, Yeilding N, Guzzo C, Hsu M-C, Wang Y, Li S, Dooley LT, Reich K, PHOENIX 2 Study Investigators. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 52-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 2). Lancet. 2008;371:1675–84.
Xu Z, Marciniak SJ, Frederick B, Kim L, Zhuang Y, Davis HM, Zhou H. Pharmacokinetic bridging approach for developing biologics-delivery devices: a case study with a golimumab autoinjector. Clin Ther. 2015;37:427–38.
Gill KL, Machavaram KK, Rose RH, Chetty M. Potential sources of inter-subject variability in monoclonal antibody pharmacokinetics. Clin Pharmacokinet. 2016;55:789–805.
Xu Z, Davis HM, Zhou H. Rational development and utilization of antibody-based therapeutic proteins in pediatrics. Pharmacol Ther. 2013;137:225–47.
Acknowledgements
Modeling support was provided by Chyi-Hung Hsu, Yang Chen, and Chuanpu Hu. Statistical support was provided by Kim Hung Lo and Xiaoming Li. Programming support was provided by Renping Zhang and Brijesh Ravi. Medical writing support was provided by Holly Capasso-Harris of Certara Synchrogenix, under the direction of the authors in accordance with Good Publication Practice guidelines (Ann Intern Med 2015;163:461-4), and was funded by Janssen Scientific Affairs, LLC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by Janssen Research & Development, LLC. Janssen Research & Development, LLC had a role in the trial design; collection, analysis, and interpretation of data; writing of the report; and the decision to submit the article for publication.
Conflict of interest
Jocelyn H. Leu, Michael Clark, Karen Bensley, Kathleen G. Lomax, Katherine Berezny, and Zhenhua Xu are employees of Janssen Research & Development, LLC, a subsidiary of Johnson & Johnson, and may own stock in Johnson & Johnson. Honghui Zhou was an employee of Janssen Research & Development, LLC, a subsidiary of Johnson & Johnson, at the time the work was conducted and may own stock in Johnson & Johnson; Dr. Zhou is currently an employee at Elevar Therapeutics, Inc, Salt Lake City, UT, USA. Natalie J. Shiff is an employee of Janssen Scientific Affairs, LLC, a subsidiary of Johnson & Johnson; received salary support from the Childhood Arthritis and Rheumatology Research Alliance within the past 3 years; and owns or has owned stock in AbbVie, Gilead, Iovance, Johnson & Johnson, Novo-Nordisc, and Pfizer within the past 3 years. Robert M. Nelson is an employee of Johnson & Johnson and owns stock in Johnson & Johnson.
Ethics
All trials included in these analyses were conducted and reported in accordance with the ethical principles originating in the Declaration of Helsinki and in accordance with International Council for Harmonisation Good Clinical Practice guidelines, applicable regulatory requirements, and in compliance with the respective protocols.
Consent to participate
All participants or legal guardians of participants in the clinical trials included in these analyses provided written informed consent.
Consent to publication
Not applicable.
Availability of data and material (data transparency)
The data-sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinical-trials/transparency. As noted on this site, requests for access to the trial data can be submitted through Yale Open Data Access (YODA) Project site at http://yoda.yale.edu.
Code availability
Not applicable.
Author contributions
Conceptualization: JHL, NJS, KBen, KGL, KBer, RMN, HZ, ZX. Methodology: JHL, MC, KBen, KGL, KBer, RMN, HZ, ZX. Data collection and/or analysis: JHL, NJS, MC, KBen, KGL, KBer, HZ, ZX. Data interpretation: JHL, NJS, MC, KBen, KGL, KBer, RMN, HZ, ZX. Manuscript preparation, review, and editing: All authors. All authors approved the final version of the manuscript for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Leu, J.H., Shiff, N.J., Clark, M. et al. Intravenous Golimumab in Patients with Polyarticular Juvenile Idiopathic Arthritis and Juvenile Psoriatic Arthritis and Subcutaneous Ustekinumab in Patients with Juvenile Psoriatic Arthritis: Extrapolation of Data from Studies in Adults and Adjacent Pediatric Populations. Pediatr Drugs 24, 699–714 (2022). https://doi.org/10.1007/s40272-022-00533-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-022-00533-y