Abstract
Background and Objective
Systematic reviews of discrete-choice experiments (DCEs) are being increasingly conducted. The objective of this scoping review was to identify and describe the methodologies that have been used to summarize results across DCEs.
Methods
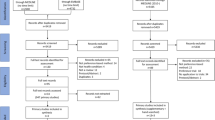
We searched the electronic databases MEDLINE and EMBASE from inception to March 18, 2021, to identify English-language systematic reviews of patient preferences that included at least two DCEs and extracted data on attribute importance. The methods used to summarize results across DCEs were classified into narrative, semi-quantitative, and quantitative (meta-analytic) approaches and compared. Approaches to characterize the extent of preference heterogeneity were also described.
Results
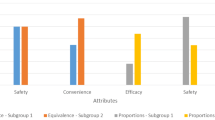
From 7362 unique records, we identified 54 eligible reviews from 2010 to Mar 2021, across a broad range of health conditions. Most (83%) used a narrative approach to summarize findings of DCEs, often citing differences in studies as the reason for not formally pooling findings. Semi-quantitative approaches included summarizing the frequency of the most important attributes, the frequency of attribute statistical significance, or tabulated comparisons of attribute importance for each pair of attributes. One review conducted a meta-analysis using the maximum acceptable risk. While reviews often commented on the heterogeneity of patient preferences, few (6%) addressed this systematically across studies.
Conclusion
While not commonly used, several semi-quantitative and one quantitative approach for synthesizing results of DCEs were identified, which may be useful for generating summary estimates across DCEs when appropriate. Further work is needed to assess the validity and usefulness of these approaches.

Similar content being viewed by others
References
Ho M, Saha A, McCleary KK, Levitan B, Christopher S, Zandlo K, et al. A framework for incorporating patient preferences regarding benefits and risks into regulatory assessment of medical technologies. Value Health. 2016;19(6):746–50.
Medical device Innovation Consortium (MDIC). Medical device Innovation Consortium (MDIC) patient centered benefit-risk project report: a framework for incorporating information on patient preferences regarding benefit and risk into regulatory assessments of new medical technology; 2015.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–13.
Soekhai V, de Bekker-Grob EW, Ellis AR, Vass CM. Discrete choice experiments in health economics: past, present and future. Pharmacoeconomics. 2019;37(2):201–26.
Yu T, Enkh-Amgalan N, Zorigt G. Methods to perform systematic reviews of patient preferences: a literature survey. BMC Med Res Methodol. 2017;17(1):166.
Durand C, Eldoma M, Marshall DA, Bansback N, Hazlewood GS. Patient preferences for disease-modifying antirheumatic drug treatment in rheumatoid arthritis: a systematic review. J Rheumatol. 2020;47(2):176–87.
Gonzalez JM. Evaluating risk tolerance from a systematic review of preferences: the case of patients with psoriasis. Patient. 2018;11(3):285–300.
Purnell TS, Joy S, Little E, Bridges JF, Maruthur N. Patient preferences for noninsulin diabetes medications: a systematic review. Diabetes Care. 2014;37(7):2055–62.
Selva A, Sola I, Zhang Y, Pardo-Hernandez H, Haynes RB, Martinez Garcia L, et al. Development and use of a content search strategy for retrieving studies on patients’ views and preferences. Health Qual Life Outcomes. 2017;15(1):126.
van Hoorn R, Kievit W, Booth A, Mozygemba K, Lysdahl KB, Refolo P, et al. The development of PubMed search strategies for patient preferences for treatment outcomes. BMC Med Res Methodol. 2016;29(16):88.
Wessels M, Hielkema L, van der Weijden T. How to identify existing literature on patients’ knowledge, views, and values: the development of a validated search filter. J Med Libr Assoc. 2016;104(4):320–4.
Al-Omari B, McMeekin P, Bate A. Systematic review of studies using conjoint analysis techniques to investigate patients’ preferences regarding osteoarthritis treatment. Patient Prefer Adherence. 2021;15:197–211.
Malde S, Umbach R, Wheeler JR, Lytvyn L, Cornu JN, Gacci M, et al. A systematic review of patients’ values, preferences, and expectations for the diagnosis and treatment of male lower urinary tract symptoms. Eur Urol. 2021;79(6):796–809.
Buhn S, Holstiege J, Pieper D. Are patients willing to accept longer travel times to decrease their risk associated with surgical procedures? A systematic review. BMC Public Health. 2020;20(1):253.
Heenan M. An opportunity for improved engagement and transparency: a systematic review of renal dialysis cost effectiveness and discrete choice experiment studies. Healthc Manag Forum. 2020;33(5):200–5.
Lack A, Hiligsmann M, Bloem P, Tunnessen M, Hutubessy R. Parent, provider and vaccinee preferences for HPV vaccination: a systematic review of discrete choice experiments. Vaccine. 2020;38(46):7226–38.
Lepper S, Radke A, Wehrmann H, Michalowsky B, Hoffmann W. Preferences of cognitively impaired patients and patients living with dementia: a systematic review of quantitative patient preference studies. J Alzheimers Dis. 2020;77(2):885–901.
Livingstone A, Agarwal A, Stockler MR, Menzies AM, Howard K, Morton RL. Preferences for immunotherapy in melanoma: a systematic review. Ann Surg Oncol. 2020;27(2):571–84.
Sain N, Willems D, Charokopou M, Hiligsmann M. The importance of understanding patient and physician preferences for psoriasis treatment characteristics: a systematic review of discrete-choice experiments. Curr Med Res Opin. 2020;36(8):1257–75.
Sharma M, Ong JJ, Celum C, Terris-Prestholt F. Heterogeneity in individual preferences for HIV testing: a systematic literature review of discrete choice experiments. EClinicalMedicine. 2020;29–30:100653.
Sugitani Y, Sugitani N, Ono S. Quantitative preferences for lung cancer treatment from the patients’ perspective: a systematic review. Patient. 2020;13(5):521–36.
Tunnessen M, Hiligsmann M, Stock S, Vennedey V. Patients’ preferences for the treatment of anxiety and depressive disorders: a systematic review of discrete choice experiments. J Med Econ. 2020;23(6):546–56.
Visser LA, Louapre C, Uyl-de Groot CA, Redekop WK. Patient needs and preferences in relapsing-remitting multiple sclerosis: a systematic review. Mult Scler Relat Disord. 2020;39:101929.
Barrionuevo P, Gionfriddo MR, Castaneda-Guarderas A, Zeballos-Palacios C, Bora P, Mohammed K, et al. Women’s values and preferences regarding osteoporosis treatments: a systematic review. J Clin Endocrinol Metab. 2019;104(5):1631–6.
Guerra RL, Castaneda L, de Albuquerque RCR, Ferreira CBT, Correa FM, Fernandes RRA, et al. Patient preferences for breast cancer treatment interventions: a systematic review of discrete choice experiments. Patient. 2019;12(6):559–69.
Magliano C, Monteiro AL, de Oliveira Rebelo AR, de Aguiar Pereira CC. Patients’ preferences for coronary revascularization: a systematic review. Patient Prefer Adherence. 2019;13:29–35.
Oedingen C, Bartling T, Muhlbacher AC, Schrem H, Krauth C. Systematic review of public preferences for the allocation of donor organs for transplantation: principles of distributive justice. Patient. 2019;12(5):475–89.
Toroski M, Kebriaeezadeh A, Esteghamati A, Karyani AK, Abbasian H, Nikfar S. Patient and physician preferences for type 2 diabetes medications: a systematic review. J Diabetes Metab Disord. 2019;18(2):643–56.
Vass CM, Georgsson S, Ulph F, Payne K. Preferences for aspects of antenatal and newborn screening: a systematic review. BMC Pregnancy Childbirth. 2019;19(1):131.
Barber S, Pavitt S, Khambay B, Bekker H, Meads D. Eliciting preferences in dentistry with multiattribute stated preference methods: a systematic review. JDR Clin Trans Res. 2018;3(4):326–35.
Clark MD, Szczepura A, Gumber A, Howard K, Moro D, Morton RL. Measuring trade-offs in nephrology: a systematic review of discrete choice experiments and conjoint analysis studies. Nephrol Dial Transplant. 2018;33(2):348–55.
Florek AG, Wang CJ, Armstrong AW. Treatment preferences and treatment satisfaction among psoriasis patients: a systematic review. Arch Dermatol Res. 2018;310(4):271–319.
Goshua A, Craigie S, Guyatt GH, Agarwal A, Li R, Bhullar JS, et al. Patient values and preferences regarding opioids for chronic noncancer pain: a systematic review. Pain Med. 2018;19(12):2469–80.
Lee SJ, O’Leary MC, Umble KE, Wheeler SB. Eliciting vulnerable patients’ preferences regarding colorectal cancer screening: a systematic review. Patient Prefer Adherence. 2018;12:2267–82.
Regmi K, Kaphle D, Timilsina S, Tuha NAA. Application of discrete-choice experiment methods in tobacco control: a systematic review. Pharmacoecon Open. 2018;2(1):5–17.
Zhang Y, Morgan RL, Alonso-Coello P, Wiercioch W, Bala MM, Jaeschke RR, et al. A systematic review of how patients value COPD outcomes. Eur Respir J. 2018;52(1):1800222.
Bien DR, Danner M, Vennedey V, Civello D, Evers SM, Hiligsmann M. Patients’ preferences for outcome, process and cost attributes in cancer treatment: a systematic review of discrete choice experiments. Patient. 2017;10(5):553–65.
Kleij KS, Tangermann U, Amelung VE, Krauth C. Patients’ preferences for primary health care—a systematic literature review of discrete choice experiments. BMC Health Serv Res. 2017;17(1):476.
Landfeldt E, Edstrom J, Lindgren P, Lochmuller H. Patient preferences for treatments of neuromuscular diseases: a systematic literature review. J Neuromuscul Dis. 2017;4(4):285–92.
Loewen PS, Ji AT, Kapanen A, McClean A. Patient values and preferences for antithrombotic therapy in atrial fibrillation. A narrative systematic review. Thromb Haemost. 2017;117(6):1007–22.
Morrell L, Wordsworth S, Rees S, Barker R. Does the public prefer health gain for cancer patients? A systematic review of public views on cancer and its characteristics. Pharmacoeconomics. 2017;35(8):793–804.
Reen GK, Silber E, Langdon DW. Multiple sclerosis patients’ understanding and preferences for risks and benefits of disease-modifying drugs: a systematic review. J Neurol Sci. 2017;15(375):107–22.
Wilke T, Bauer S, Mueller S, Kohlmann T, Bauersachs R. Patient preferences for oral anticoagulation therapy in atrial fibrillation: a systematic literature review. Patient. 2017;10(1):17–37.
Belinchon I, Rivera R, Blanch C, Comellas M, Lizan L. Adherence, satisfaction and preferences for treatment in patients with psoriasis in the European Union: a systematic review of the literature. Patient Prefer Adherence. 2016;10:2357–67.
Hollowell J, Li Y, Malouf R, Buchanan J. Women’s birth place preferences in the United Kingdom: a systematic review and narrative synthesis of the quantitative literature. BMC Pregnancy Childbirth. 2016;16(1):213.
Mansfield C, Tangka FK, Ekwueme DU, Smith JL, Guy GP Jr, Li C, et al. Stated preference for cancer screening: a systematic review of the literature, 1990–2013. Prev Chronic Dis. 2016;25(13):E27.
Ridyard CH, Dawoud DM, Tuersley LV, Hughes DA. A systematic review of patients’ perspectives on the subcutaneous route of medication administration. Patient. 2016;9(4):281–92.
Schmidt K, Damm K, Prenzler A, Golpon H, Welte T. Preferences of lung cancer patients for treatment and decision-making: a systematic literature review. Eur J Cancer Care (Engl). 2016;25(4):580–91.
Yahanda AT, Lafaro KJ, Spolverato G, Pawlik TM. A systematic review of the factors that patients use to choose their surgeon. World J Surg. 2016;40(1):45–55.
Currie A, Askari A, Nachiappan S, Sevdalis N, Faiz O, Kennedy R. A systematic review of patient preference elicitation methods in the treatment of colorectal cancer. Colorectal Dis. 2015;17(1):17–25.
Eiring O, Landmark BF, Aas E, Salkeld G, Nylenna M, Nytroen K. What matters to patients? A systematic review of preferences for medication-associated outcomes in mental disorders. BMJ Open. 2015;5(4): e007848.
Schatz NK, Fabiano GA, Cunningham CE, dosReis S, Waschbusch DA, Jerome S, et al. Systematic review of patients’ and parents’ preferences for ADHD treatment options and processes of care. Patient. 2015;8(6):483–97.
Wilkinson G, Drummond M. Alternative approaches for assessing the socioeconomic benefits of medical devices: a systematic review. Expert Rev Med Devices. 2015;12(5):629–48.
von Arx LB, Kjeer T. The patient perspective of diabetes care: a systematic review of stated preference research. Patient. 2014;7(3):283–300.
Higgins A, Barnett J, Meads C, Singh J, Longworth L. Does convenience matter in health care delivery? A systematic review of convenience-based aspects of process utility. Value Health. 2014;17(8):877–87.
Lizan L, Comellas M, Paz S, Poveda JL, Meletiche DM, Polanco C. Treatment adherence and other patient-reported outcomes as cost determinants in multiple sclerosis: a review of the literature. Patient Prefer Adherence. 2014;8:1653–64.
Whitty JA, Lancsar E, Rixon K, Golenko X, Ratcliffe J. A systematic review of stated preference studies reporting public preferences for healthcare priority setting. Patient. 2014;7(4):365–86.
Wortley S, Wong G, Kieu A, Howard K. Assessing stated preferences for colorectal cancer screening: a critical systematic review of discrete choice experiments. Patient. 2014;7(3):271–82.
MacLean S, Mulla S, Akl EA, Jankowski M, Vandvik PO, Ebrahim S, et al. Patient values and preferences in decision making for antithrombotic therapy: a systematic review: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e1S-23S.
Umar N, Yamamoto S, Loerbroks A, Terris D. Elicitation and use of patients’ preferences in the treatment of psoriasis: a systematic review. Acta Derm Venereol. 2012;92(4):341–6.
Emberton M. Medical treatment of benign prostatic hyperplasia: physician and patient preferences and satisfaction. Int J Clin Pract. 2010;64(10):1425–35.
Marshall D, McGregor SE, Currie G. Measuring preferences for colorectal cancer screening: what are the implications for moving forward? Patient. 2010;3(2):79–89.
Zhang Y, Alonso-Coello P, Guyatt GH, Yepes-Nunez JJ, Akl EA, Hazlewood G, et al. GRADE Guidelines: 19. Assessing the certainty of evidence in the importance of outcomes or values and preferences-Risk of bias and indirectness. J Clin Epidemiol. 2019;111:94–104.
Zhang Y, Coello PA, Guyatt GH, Yepes-Nunez JJ, Akl EA, Hazlewood G, et al. GRADE guidelines: 20. Assessing the certainty of evidence in the importance of outcomes or values and preferences-inconsistency, imprecision, and other domains. J Clin Epidemiol. 2019;111:83–93.
Joy SM, Little E, Maruthur NM, Purnell TS, Bridges JF. Patient preferences for the treatment of type 2 diabetes: a scoping review. Pharmacoeconomics. 2013;31(10):877–92.
National Institutes of Health. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–77.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open. 2016;6(12): e011458.
Yepes-Nunez JJ, Zhang Y, Xie F, Alonso-Coello P, Selva A, Schunemann H, et al. Forty-two systematic reviews generated 23 items for assessing the risk of bias in values and preferences’ studies. J Clin Epidemiol. 2017;85:21–31.
Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1(3):176–84.
Centre for Evidence-Based Medicine (CEBM). Critical Appraisal Tools. Oxford; 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Potential competing interests and disclosures
None.
Author contributions
Planning and conducting the study (GH, DC), data collection (DC, MT, KPB), data interpretation (GH, DC) drafting the manuscript (all authors). All authors have approved the final draft submitted.
Data availability statement
The data extraction form is available from authors on request.
Guarantor of the article
Dr. Glen Hazlewood
Financial support
Dr. Hazlewood is supported by a Canadian Institutes of Health Research New Investigator Award. No financial support was provided for this study.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Writing Assistance
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Choudhary, D., Thomas, M., Pacheco-Barrios, K. et al. Methods to Summarize Discrete-Choice Experiments in a Systematic Review: A Scoping Review. Patient 15, 629–639 (2022). https://doi.org/10.1007/s40271-022-00587-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-022-00587-7