Abstract
Background and Objectives
Irinotecan sometimes causes lethal septic shock but the risk factors remain unclear. This retrospective case-control study explored the potential risk factors for septic shock following irinotecan treatment.
Methods
All women who received irinotecan-containing chemotherapy for gynecologic malignancies at Shizuoka General Hospital from October 2014 to September 2020 were investigated. The clinical backgrounds and blood test results of those who developed septic shock after irinotecan-containing chemotherapy were compared with those who did not. Odds ratios (ORs) for developing septic shock after receiving irinotecan were calculated with 95% confidence intervals (CIs), using univariable logistic regression analysis.
Results
During the study period, 147 women received irinotecan-containing chemotherapy. Three women developed septic shock due to neutropenic enterocolitis after irinotecan treatment, and 144 did not. The three patients with septic shock had recurrent cervical cancer, heterozygous variants in the uridine diphosphate glucuronosyltransferase 1A1 (UGT1A1) gene (two patients had *1/*6, one had *1/*28 variants), a history of concurrent chemoradiation therapy, 50–60 Gy of pelvic irradiation, and platinum-combined chemotherapy. A history of pelvic irradiation was identified as a possible risk factor for developing septic shock after irinotecan-containing chemotherapy (OR 63.0, 95% CI 5.71–8635; p < 0.001). The OR of UGT1A1 polymorphism for septic shock was 9.09 (95% CI 0.86–1233; p = 0.070) in the complete case analysis.
Conclusion
Medical personnel involved in cancer therapy should consider the possible risk of septic shock developing due to neutropenic enterocolitis when administering irinotecan-containing chemotherapy in patients with a history of pelvic irradiation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This retrospective case-control study was designed to explore the potential risk factors for developing septic shock following irinotecan-containing chemotherapy. |
We found that a history of pelvic irradiation might be a risk factor for irinotecan-induced septic shock (odds ratio 63.0, 95% confidence interval 5.71–8635; p < 0.001). |
All medical personnel involved in cancer therapy should be aware of the possible risk of developing septic shock due to neutropenic enterocolitis when administering irinotecan in patients with a history of pelvic irradiation. |
1 Introduction
Irinotecan is used in chemotherapy for gynecological cancers, including cervical cancer and ovarian cancer, sometimes in combination with other cytotoxic agents, such as nedaplatin and cisplatin [1, 2]. Irinotecan is metabolized into SN38, which is an active metabolite of carboxylesterases. SN38 is glucuronidated in the liver by uridine diphosphate glucuronosyltransferase 1A1 (UGT1A1) and is inactivated by the formation of SN38 glucuronide (SN38-G). The UGT1A1*6 and UGT1A1*28 polymorphisms affect the pharmacokinetics and toxicity of SN38. Homozygous UGT1A1 variants (*6/*6, *28/*28), double heterozygous (*6/*28), and heterozygous variants (*1/*6 and *1/*28) are associated with reduced UGT1A1 glucuronidation activity, compared with the wild-type allele (*1/*1), resulting in increased risk for severe irinotecan-induced toxicity [3,4,5]. It has been reported that some patients may develop lethal septic shock following irinotecan treatment [6,7,8]; however, not all patients with homozygous or heterozygous UGT1A1 variants experience such severe adverse effects. Therefore, the risk factors for developing lethal adverse effects following irinotecan therapy remain unclear.
We experienced several clinical cases of septic shock with severe myelosuppression after irinotecan administration (see the representative case in Sect. 1.1). All patients were admitted to the intensive care unit (ICU) and one of them eventually died. Their clinical course was severe and they deteriorated rapidly. We have never experienced this course when using other anticancer agents, therefore we conducted a retrospective case-control study to explore the potential risk factors, other than UGT1A1 polymorphisms, that might induce life-threatening complications in patients receiving irinotecan.
1.1 Representative Case
A 60-year-old patient had a peritoneal recurrence of cervical cancer. She had received concurrent chemoradiation therapy as first-line therapy for stage IVA squamous cell carcinoma and six cycles of carboplatin plus paclitaxel. Salvage chemotherapy with irinotecan and nedaplatin was planned for the metastases. UGT1A1 genotyping revealed a heterozygous variant in UGT1A1 (UGT1A1*6). Irinotecan (60 mg/m2) and nedaplatin (80 mg/m2) were administered on day 1. On day 8, irinotecan (60 mg/m2) was administered since myelosuppression was absent (neutrophil count 3182/μL). On day 10, the patient was admitted to hospital because of severe diarrhea. Myelosuppression was not severe at this point (neutrophil count 1851/μL). On day 12, the patient suddenly developed severe myelosuppression with neutrophil counts of 181/μL. She had no fever and her diarrhea improved with loperamide treatment.
On day 13, the patient’s vital signs suddenly worsened: body temperature 37.4 °C, pulse 121 beats/minute, blood pressure 80/49 mmHg, and SpO2 87% (room air). Laboratory data showed that her neutrophil was undetectable. Septic shock was strongly suspected and appropriate treatment was started immediately. The patient was transferred to the ICU and further treatments, including continuous hemodiafiltration and intubation, were continued. Blood culture was positive for Enterobacter species, Klebsiella pneumoniae, Enterococcus faecalis, and Pseudomonas aeruginosa, which strongly suggested that the focus of the infection was the intestine. Intestinal edema was also observed on computed tomography (CT) (Fig. 1). Neutropenic enterocolitis was strongly suspected based on the patient’s symptoms (severe diarrhea), blood culture result, and CT findings [9, 10]. Despite the repeated use of granulocyte colony-stimulating factor, the neutrophil count remained below 50/μL. On day 20, the patient died of multiple organ failure due to septic shock.
2 Methods
We conducted a retrospective case-control study to explore the risk factors for septic shock following irinotecan administration. All women who received irinotecan-containing chemotherapy for gynecologic malignancies at Shizuoka General Hospital between October 2014 and September 2020 were investigated in this study. Data were retrospectively collected from clinical records.
The clinical background and blood test results before chemotherapy in patients who developed septic shock after irinotecan-containing chemotherapy were compared with those of patients who did not develop septic shock. To explore the risk factors for septic shock due to irinotecan administration, odds ratios (ORs) for developing septic shock after receiving irinotecan were calculated with 95% confidence intervals (CIs) using univariable logistic regression analysis for the following possible risk factors: age, body mass index (BMI), neutrophil count, hemoglobin, platelet count, serum creatinine level, serum total bilirubin level, UGT1A1 polymorphism [3, 5, 11], history of pelvic irradiation [10], administration of hangeshashinto (a Japanese herbal medicine used to treat irinotecan-associated diarrhea) [12], platinum combination therapy, history of chemotherapy [13], and history of abdominal surgery. Abdominal surgery was defined as gastrointestinal surgery and hysterectomy. Less invasive surgeries, including cesarean section, oophorectomy, cystectomy without hysterectomy, or exploratory laparotomy, were excluded. For blood tests and BMI, the data collected within 7 days before irinotecan administration were used. Univariable logistic regression analysis with Firth correction was performed to estimate ORs with 95% CIs using the R package ‘logistf’ version 1.24. Statistical analysis was performed using R version 3.6.0 (The R Foundation for Statistical Computing, Vienna, Austria).
The Institutional Review Board of Shizuoka General Hospital approved this study (reference number: SGHIRB#2021015).
3 Results
A total of 147 women with cervical, endometrial, ovarian, vaginal, or vulvar cancer received irinotecan-containing chemotherapy in our hospital during the study period. Three women developed septic shock after the first cycle of irinotecan-containing chemotherapy and all three were admitted to the ICU.
The irinotecan dose was 100 mg/m2 in irinotecan monotherapy and 60 mg/m2 in platinum combined chemotherapy, and for platinum combined chemotherapy, the doses of nedaplatin and cisplatin were 80 mg/m2 and 60 mg/m2, respectively. The irinotecan dose was reduced by 50% in patients with homozygous UGT1A1 variants (*6/*6, *28/*28) and double heterozygous variants (*6/*28).
3.1 Characteristics and Clinical Course of the Three Patients with Septic Shock
All women who developed septic shock were patients with recurrent cervical cancer who carried heterozygous variants in UGT1A1 (two with UGT1A1*1/*6, one with UGT1A1*1/*28) and received platinum combined chemotherapy (irinotecan plus nedaplatin). Moreover, all patients had a history of concurrent chemoradiation therapy and received 50–60 Gy of pelvic irradiation within a year. Chemoradiation therapy was conducted as the initial treatment for cervical cancer in two patients, while one patient underwent a modified radical hysterectomy as the initial treatment for cervical cancer. Chemotherapy without radiation therapy (six cycles of carboplatin plus paclitaxel) was conducted for the recurrence in Case 1, but not in the other two patients.
The clinical courses of these three women were similar (Table 1). On day 1, irinotecan and nedaplatin were administered and on day 8 irinotecan was administered according to the treatment protocol since no severe adverse effects were observed. On days 10‒14, the women developed severe diarrhea and severe myelosuppression, and subsequently developed neutropenic enterocolitis and septic shock, which resulted in death or prolonged hospitalization. Prominent intestinal edema was observed on CT in Case 1 (Fig. 1a, b) and Case 2. The blood cultures were positive in two cases: Enterobacter species, Klebsiella pneumoniae, Enterococcus faecalis, and Pseudomonas aeruginosa in Case 1, and Candida albicans in Case 2.
3.2 Univariable Logistic Regression Analysis
The calculated ORs for developing septic shock after receiving irinotecan-containing chemotherapy are shown in Table 2. A history of pelvic irradiation was suggested as a risk factor for developing septic shock after irinotecan-containing chemotherapy (OR 63.0, 95% CI 5.71–8635; p < 0.001). Pelvic irradiation was conducted in 17 women (cervical cancer, n = 15; vaginal cancer, n = 1; vulvar cancer, n = 1) before irinotecan-containing chemotherapy, and three women developed septic shock. In 15 women, pelvic irradiation was conducted as the initial treatment. All 17 women with a history of pelvic irradiation received platinum combined therapy.
A history of chemotherapy was also suspected to be a risk factor (OR 10.7, 95% CI 1.01–1442; p = 0.049). UGT1A1 polymorphism was not assessed in 22 cases, as prior to 2014 this test was conducted only when severe toxicity was observed. Excluding cases with missing data from the UGT1A1 polymorphism test, the OR of the UGT1A1 polymorphism for septic shock was 9.09 (95% CI 0.86–1233; p = 0.070). A history of abdominal surgery was present in 62 women. The OR of a history of abdominal surgery for septic shock was 0.81 (95% CI 0.07–6.28; p = 0.84).
4 Discussion
In this study, a history of pelvic irradiation was suggested to be a risk factor for irinotecan-induced septic shock. Although this result was obtained by univariable analysis, and multivariable analysis was not conducted due to the small number of events, the estimated OR was as high as 63.0 (95% CI 5.71–8635; p < 0.001).
UGT1A1 polymorphism affects the risk of irinotecan-related severe toxicity [3, 5, 11]. A dose reduction of irinotecan is recommended for patients with homozygous variants [14], while there is no consensus on the need for dose reduction in patients with heterozygous variants [5]. In our analysis, the point estimate OR of UGT1A1 polymorphism for septic shock was 9.09 but its 95% CI crossed 1 (0.86–1233; p = 0.070) when we excluded 22 cases with missing data for the UGT1A1 polymorphism test. This may be because, before 2015, UGT1A1 polymorphism was evaluated only when severe toxicity was observed. It should be noted that the OR of the UGT1A1 polymorphism might be underestimated since patients with missing data on UGT1A1 were more likely to be wild-type than those without missing data on UGT1A1, resulting in selection bias.
A history of pelvic irradiation can also plausibly increase the risk of septic shock after irinotecan administration. All three cases of septic shock in our study were diagnosed with neutropenic enterocolitis. A similar case has also been reported previously [9]. Neutropenic enterocolitis is a life-threatening complication in immunosuppressed patients and is diagnosed by clinical symptoms and signs, including fever, abdominal pain, and CT or ultrasound findings [10]. Neutropenic enterocolitis is induced by mucosal injury and myelosuppression caused by cytotoxic drugs [10]. We assume that neutropenic enterocolitis was induced in our patients due to the combined effect of intestinal mucosal injury by irinotecan and previous pelvic irradiation.
Irinotecan causes intestinal mucosal injury via the following mechanism: SN38 is converted into the inactive product SN38-G in the liver by UGT1A1, which is then excreted into the bile. In the intestinal compartment, bacterial β-glucuronidase reactivates SN38-G to release SN38 [3, 4]. UGT1A1 variants are associated with reduced UGT1A1 enzyme activity involved in the inactivation of SN38, resulting in increased toxicity to the intestinal mucosa and severe diarrhea in patients with UGT1A1*6 or UGT1A1*28 [3].
Moreover, irradiation is reported to damage the intestinal mucosa [15]. The most common complications in patients with a history of pelvic irradiation are gastrointestinal complications [16]. Considering that damage to the intestine by irradiation has been reported to last for more than 30 years [17], it is plausible that in our patients, irinotecan administration caused further damage to the intestinal mucosa that had already been injured by pelvic irradiation, resulting in loss of the mucosal barrier and ingress of intestinal bacteria. Indeed, blood cultures were positive in two cases: multispecies of intestinal bacteria in Case 1, suggesting bacterial translocation, and Candida albicans in Case 2 (Table 1). Since both bacterial translocation and fungi infection are characteristics of neutropenic enterocolitis, the blood culture results support our hypothesis [10].
Furthermore, a history of pelvic irradiation can also be a risk factor for severe myelosuppression. Irradiation causes bone marrow dysfunction due to direct injury to hematopoietic stem cells and structural functional damage to the stroma or microcirculation [18]. It has been reported that myelosuppression after chemotherapy can be more severe in patients with a history of irradiation [10]. Since the pelvis and vertebrae account for approximately 60% of the functional bone marrow, irradiation of these lesions is more likely to cause severe myelosuppression [19]. Among them, the pelvis is included in the radiation field for cervical cancer [20].
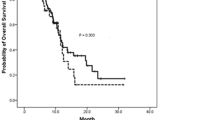
Thus, in our cases, it is possible that pelvic irradiation might have impaired hematopoietic ability and imposed an additive risk for myelosuppression due to chemotherapy [21, 22]. In the representative case, myelosuppression was so severe that the neutrophil count continued to be below 50/μL for 8 days despite daily administration of granulocyte colony-stimulating factor. We assumed that mucosal damage due to irinotecan and previous pelvic irradiation together with severe myelosuppression induced neutropenic enterocolitis and septic shock (Fig. 2).
A history of chemotherapy might also be a risk factor for the development of septic shock (OR 10.7, 95% CI 1.01–1442; p = 0.049). Although the OR of platinum-combined chemotherapy for septic shock was not elevated (0.49, 95% CI 0.04–67.8; p = 0.67), all three patients with septic shock were treated with platinum-combined therapy. Combination chemotherapy including platinum should be administered carefully when patients have homozygous, double heterozygous, or heterozygous UGT1A1 variants and have a history of pelvic irradiation. A history of abdominal surgery was not shown as a risk factor for septic shock (OR 0.81, 95% CI 0.07–6.28) in this study.
Irinotecan is commonly used for various malignancies, including colon cancer, gastric cancer, pancreatic cancer, and gynecologic cancer [4, 6, 7, 14]. In these malignancies, irinotecan is widely used as a platinum combined regimen: FOLFOXIRI for colon cancer, FOLFIRINOX for pancreatic cancer, and irinotecan plus cisplatin for advanced and recurrent small cell lung cancer [4, 23, 24]. Thus, a history of pelvic irradiation, particularly in cases with UGT1A1 variants, should also be considered when administering irinotecan in patients with these cancers, as in patients with gynecologic cancers.
Patients with cervical cancer tend to be relatively young: the median age of diagnosis is reported to be 47 years and almost 50% of cases are diagnosed under the age of 35 years [20]. Concurrent chemoradiotherapy is a standard treatment for cervical cancer and cures a considerable number of these women [25]. It is possible that some of these women with a history of pelvic irradiation may suffer from other malignancies, including colon cancer, gastric cancer, and pancreatic cancer, later in their lives and may then receive irinotecan-containing chemotherapy. Our three cases with septic shock had a history of pelvic irradiation within a year. However, given the long-lasting effects of damage to the intestinal mucosa by irradiation (> 30 years) [17, 18], the effect of pelvic irradiation and the possibility of developing septic shock by irinotecan administration, due to neutropenic enterocolitis, should be kept in mind for a considerably long period after irradiation.
This study had several limitations. First, this was a retrospective study conducted in a single center. Second, there is concern about selection bias due to the limited number of patients included. However, even though this study was simply an exploratory study to find potential risk factors for septic shock after irinotecan treatment, the calculated OR of pelvic irradiation for developing septic shock was remarkably high (63.0, 95% CI 5.71–8635; p < 0.001) and had a plausible etiology.
5 Conclusions
Our study suggests that a history of pelvic irradiation might be a risk factor for lethal complications after irinotecan therapy. In addition to UGT1A1 variants, a history of pelvic irradiation should be acknowledged as a possible risk factor for severe complications following irinotecan-containing chemotherapy. We suggest avoiding the administration of irinotecan, or at least administrating a reduced dose in patients with both UGT1A1 homozygous, double heterozygous, or heterozygous variants and a history of pelvic irradiation. All medical personnel involved in cancer therapy should be aware of the possible risk of developing septic shock due to neutropenic enterocolitis when administering irinotecan in patients with a history of pelvic irradiation. Further studies are required to evaluate this hypothesis.
References
Tsuda H, Hashiguchi Y, Nishimura S, Miyama M, Nakata S, Kawamura N, et al. Phase I-II study of irinotecan (CPT-11) plus nedaplatin (254-S) with recombinant human granulocyte colony-stimulating factor support in patients with advanced or recurrent cervical cancer. Br J Cancer. 2004;91:1032–7.
Machida S, Sato T, Fujiwara H, Saga Y, Takei Y, Taneichi A, et al. Nedaplatin and irinotecan combination therapy is equally effective and less toxic than cisplatin and irinotecan for patients with primary clear cell adenocarcinoma of the ovary and recurrent ovarian carcinoma. Oncol Lett. 2012;4:1017–22.
Takano M, Sugiyama T. UGT1A1 polymorphisms in cancer: impact on irinotecan treatment. Pharmgenomics Pers Med. 2017;10:61–8.
Bailly C. Irinotecan: 25 years of cancer treatment. Pharmacol Res. 2019;148: 104398.
Yang Y, Zhou M, Hu M, Cui Y, Zhong Q, Liang L, et al. UGT1A1*6 and UGT1A1*28 polymorphisms are correlated with irinotecan-induced toxicity: a meta-analysis. Asia Pac J Clin Oncol. 2018;14:e479–89.
Kuehr T, Ruff P, Rapoport BL, Falk S, Daniel F, Jacobs C, et al. Phase I/II study of first-line irinotecan combined with 5-fluorouracil and folinic acid Mayo Clinic schedule in patients with advanced colorectal cancer. BMC Cancer. 2004;4:36.
Kim JH, Lee SC, Oh SY, Song SY, Lee N, Nam EM, et al. Attenuated FOLFIRINOX in the salvage treatment of gemcitabine-refractory advanced pancreatic cancer: a phase II study. Cancer Commun (Lond). 2018;38:32.
Riera P, Salazar J, Virgili AC, Tobena M, Sebio A, Gallano P, et al. Relevance of CYP3A4*20, UGT1A1*37 and UGT1A1*28 variants in irinotecan-induced severe toxicity. Br J Clin Pharmacol. 2018;84:1389–92.
Takaoka E, Kawai K, Ando S, Shimazui T, Akaza H. Neutropenic colitis during standard dose combination chemotherapy with nedaplatin and irinotecan for testicular cancer. Jpn J Clin Oncol. 2006;36:60–3.
Rodrigues FG, Dasilva G, Wexner SD. Neutropenic enterocolitis. World J Gastroenterol. 2017;23:42–7.
Zhang X, Yin JF, Zhang J, Kong SJ, Zhang HY, Chen XM. UGT1A1*6 polymorphisms are correlated with irinotecan-induced neutropenia: a systematic review and meta-analysis. Cancer Chemother Pharmacol. 2017;80:135–49.
Urushiyama H, Jo T, Yasunaga H, Michihata N, Yamana H, Matsui H, et al. Effect of Hangeshashin-To (Japanese Herbal Medicine Tj-14) on tolerability of irinotecan: propensity score and instrumental variable analyses. J Clin Med. 2018;7(9):246.
MacManus M, Lamborn K, Khan W, Varghese A, Graef L, Knox S. Radiotherapy-associated neutropenia and thrombocytopenia: analysis of risk factors and development of a predictive model. Blood. 1997;89:2303–10.
Hulshof EC, Deenen MJ, Guchelaar HJ, Gelderblom H. Pre-therapeutic UGT1A1 genotyping to reduce the risk of irinotecan-induced severe toxicity: ready for prime time. Eur J Cancer. 2020;141:9–20.
Rolston KV. Infections in cancer patients with solid tumors: a review. Infect Dis Ther. 2017;6:69–83.
Shafi MA, Bresalier RS. The gastrointestinal complications of oncologic therapy. Gastroenterol Clin N Am. 2010;39:629–47.
Harb AH, Abou Fadel C, Sharara AI. Radiation enteritis. Curr Gastroenterol Rep. 2014;16:383.
Mauch P, Constine L, Greenberger J, Knospe W, Sullivan J, Liesveld JL, et al. Hematopoietic stem cell compartment: acute and late effects of radiation therapy and chemotherapy. Int J Radiat Oncol Biol Phys. 1995;31:1319–39.
Prabhu RS, Cassidy RJ, Landry JC. Radiation therapy and neutropenia. Curr Probl Cancer. 2015;39:292–6.
Cohen PA, Jhingran A, Oaknin A, Denny L. Cervical cancer. The Lancet. 2019;393:169–82.
Kumar T, Schernberg A, Busato F, Laurans M, Fumagalli I, Dumas I, et al. Correlation between pelvic bone marrow radiation dose and acute hematological toxicity in cervical cancer patients treated with concurrent chemoradiation. Cancer Manag Res. 2019;11:6285–97.
Hui B, Zhang Y, Shi F, Wang J, Wang T, Wang J, et al. Association between bone marrow dosimetric parameters and acute hematologic toxicity in cervical cancer patients undergoing concurrent chemoradiotherapy: comparison of three-dimensional conformal radiotherapy and intensity-modulated radiation therapy. Int J Gynecol Cancer. 2014;24:1648–52.
Noda K, Nishiwaki Y, Kawahara M, Negoro S, Sugiura T, Yokoyama A, et al. Irinotecan plus cisplatin compared with etoposide plus cisplatin for extensive small-cell lung cancer. N Engl J Med. 2002;346:85–91.
Loupakis F, Cremolini C, Masi G, Lonardi S, Zagonel V, Salvatore L, et al. Initial therapy with FOLFOXIRI and bevacizumab for metastatic colorectal cancer. N Engl J Med. 2014;371:1609–18.
Rose PG, Ali S, Watkins E, Thigpen JT, Deppe G, Clarke-Pearson DL, et al. Long-term follow-up of a randomized trial comparing concurrent single agent cisplatin, cisplatin-based combination chemotherapy, or hydroxyurea during pelvic irradiation for locally advanced cervical cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2007;25:2804–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflicts of interest
Maki Umemiya, Yoshihide Inayama, Eiji Nakatani, Kenta Ito, Mitsuru Tsuji, Teruki Yoshida, Sae Yu, Rei Gou, Naoki Horikawa, Hirohiko Tani, and Kenzo Kosaka declare they have no conflicts of interest.
Availability of data and material
The minimal datasets that are required to replicate the outcomes of the study will be made available by the corresponding author upon reasonable request. The data are not publicly available due to privacy or ethical restrictions.
Ethics approval
The Institutional Review Board of Shizuoka General Hospital approved this study (reference number: SGHIRB#2021015).
Consent to participate
The need to obtain written informed consent from patients was waived because of the retrospective design of this study. For the representative case, consent for publication was obtained from a family member of the patient.
Author contributions
Conceptualization and design: MU, YI, NH, HT and KK. Investigation: MU, YI, TY, SY, MT and RG. Data curation: MU, YI, EN and KI. Writing of the original draft: MU, YI, EN and KI. Review and editing: TY, SY, MT, RG, NH, HT and KK. Supervision: YI and KK.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Umemiya, M., Inayama, Y., Nakatani, E. et al. Risk Factors for Septic Shock After Irinotecan-Containing Chemotherapy: An Exploratory Case-Control Study. Drugs R D 22, 263–269 (2022). https://doi.org/10.1007/s40268-022-00399-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-022-00399-y