Abstract
Background
Although proton pump inhibitors (PPIs) play a pivotal role in the prevention and treatment of gastric acid-related diseases and gastrointestinal adverse events caused by antiplatelet therapies, the safety of long-term use of PPIs has been questioned.
Objective
The aim of this study was to determine the effects of use of PPIs on muscle mass and bone mineral density in heart failure (HF) patients.
Methods
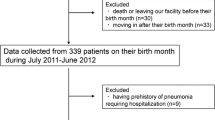
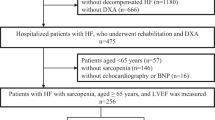
This was a single-center, ambispective (combined retrospective and prospective), observational study. HF patients (n = 747; 72 years of age; males, 54%) who received a dual-energy x-ray absorptiometry scan were enrolled. Muscle wasting was defined as appendicular skeletal muscle mass index (ASMI) < 7.0 kg/m2 in males and <5.4 kg/m2 in females. Propensity scores for the use of PPIs were calculated using a multivariate logistic regression model to minimize selection bias.
Results
Before propensity score matching, ASMI was significantly lower in patients receiving PPIs than in patients not receiving PPIs, resulting in a higher prevalence of muscle wasting in the PPI group. Such a relationship between use of PPIs and muscle wasting remained after propensity score matching. In multivariate Cox regression analyses, use of PPIs was independently associated with presence of muscle wasting (hazard ratio 1.68, 95% confidence interval 1.05–2.69) after adjustment for established risk factors of sarcopenia. On the other hand, there were no differences in bone mineral density between the PPI group and the no-PPI group.
Conclusion
Use of PPIs is associated with a high risk of muscle wasting in HF patients. Caution is warranted when long-term PPI treatment is performed in sarcopenic HF patients and HF patients with several risk factors for muscle wasting.

Similar content being viewed by others
References
Strand DS, Kim D, Peura DA. 25 years of proton pump inhibitors: a comprehensive review. Gut Liver. 2017;11:27–37.
Nehra AK, Alexander JA, Loftus CG, Nehra V. Proton pump inhibitors: review of emerging concerns. Mayo Clin Proc. 2018;93:240–6.
Lai KC, Lam SK, Chu KM, Wong BC, Hui WM, Hu WH, et al. Lansoprazole for the prevention of recurrences of ulcer complications from long-term low-dose aspirin use. N Engl J Med. 2002;346:2033–8.
Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, et al.; ESC Scientific Document Group; ESC Committee for Practice Guidelines (CPG); ESC National Cardiac Societies. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2018;39:213–60.
Steffel J, Collins R, Antz M, Cornu P, Desteghe L, Haeusler KG, External reviewers, et al. European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Europace. 2021;2021(23):1612–76.
Luo H, Fan Q, Xiao S, Chen K. Changes in proton pump inhibitor prescribing trend over the past decade and pharmacists’ effect on prescribing practice at a tertiary hospital. BMC Health Serv Res. 2018;18:537.
Liu Y, Zhu X, Li R, Zhang J, Zhang F. Proton pump inhibitor utilisation and potentially inappropriate prescribing analysis: insights from a single-centred retrospective study. BMJ Open. 2020;10: e040473.
Schoenfeld AJ, Grady D. Adverse effects associated with proton pump inhibitors. JAMA Intern Med. 2016;176:172–4.
Park CH, Kim EH, Roh YH, Kim HY, Lee SK. The association between the use of proton pump inhibitors and the risk of hypomagnesemia: a systematic review and meta-analysis. PLoS ONE. 2014;9: e112558.
Cheungpasitporn W, Thongprayoon C, Kittanamongkolchai W, Srivali N, Edmonds PJ, Ungprasert P, et al. Proton pump inhibitors linked to hypomagnesemia: a systematic review and meta-analysis of observational studies. Ren Fail. 2015;37:1237–41.
Toh JW, Ong E, Wilson R. Hypomagnesaemia associated with long-term use of proton pump inhibitors. Gastroenterol Rep (Oxf). 2015;3:243–53.
Lam JR, Schneider JL, Zhao W, Corley DA. Proton pump inhibitor and histamine 2 receptor antagonist use and vitamin B12 deficiency. JAMA. 2013;310:2435–42.
Lo WK, Chan WW. Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta-analysis. Clin Gastroenterol Hepatol. 2013;11:483–90.
Su T, Lai S, Lee A, He X, Chen S. Meta-analysis: proton pump inhibitors moderately increase the risk of small intestinal bacterial overgrowth. J Gastroenterol. 2018;53:27–36.
Vinke P, Wesselink E, van Orten-Luiten W, van Norren K. The use of proton pump inhibitors may increase symptoms of muscle function loss in patients with chronic illnesses. Int J Mol Sci. 2020;21:323.
von Haehling S, Garfias Macedo T, Valentova M, et al. Muscle wasting as an independent predictor of survival in patients with chronic heart failure. J Cachexia Sarcopenia Muscle. 2020;11:1242–9.
Konishi M, Akiyama E, Matsuzawa Y, et al. Prognostic impact of muscle and fat mass in patients with heart failure. J Cachexia Sarcopenia Muscle. 2021;12:568–76.
Konishi M, Kagiyama N, Kamiya K, et al. Impact of sarcopenia on prognosis in patients with heart failure with reduced and preserved ejection fraction. Eur J Prev Cardiol. 2021;28:1022–9.
Ohori K, Yano T, Katano S, Kouzu H, Honma S, Shimomura K, et al. High percent body fat mass predicts lower risk of cardiac events in patients with heart failure: an explanation of the obesity paradox. BMC Geriatr. 2021;21:16.
Katano S, Yano T, Tsukada T, Kouzu H, Honma S, Inoue T, et al. Clinical risk factors and prognostic impact of osteoporosis in patients with chronic heart failure. Circ J. 2020;84:2224–34.
Tsutsui H, Isobe M, Ito H, Ito H, Okumura K, Ono M, et al. JCS 2017/JHFS 2017 guideline on diagnosis and treatment of acute and chronic heart failure—digest version. Circ J. 2019;83:2084–184.
Ohori K, Yano T, Katano S, Kouzu H, Inoue T, Takamura Y, et al. Independent link between peripheral artery disease and muscle wasting in patients with heart failure. ESC Heart Fail. 2020;7:3252–6.
Kouzu H, Katano S, Yano T, Ohori K, Nagaoka R, Inoue T, et al. Plasma amino acid profiling improves predictive accuracy of adverse events in patients with heart failure. ESC Heart Fail. 2021;8:5045–56.
Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15:95–101.
Katano S, Yano T, Kouzu H, Ohori K, Shimomura K, Honma S, et al. Energy intake during hospital stay predicts all-cause mortality after discharge independently of nutritional status in elderly heart failure patients. Clin Res Cardiol. 2021;110:1202–20.
Katano S, Yano T, Shimizu M, Ohori K, Kouzu H, Koyama M, et al. Does renin-angiotensin system inhibition have impacts on muscle mass and bone mineral density in heart failure patients? ESC Heart Fail. 2021;8:2617–24.
de Baaij JH, Hoenderop JG, Bindels RJ. Magnesium in man: implications for health and disease. Physiol Rev. 2015;95:1–46.
Dominguez LJ, Barbagallo M, Lauretani F, Bandinelli S, Bos A, Corsi AM, et al. Magnesium and muscle performance in older persons: the InCHIANTI study. Am J Clin Nutr. 2006;84:419–26.
Verlaan S, Aspray TJ, Bauer JM, Cederholm T, Hemsworth J, Hill TR, et al. Nutritional status, body composition, and quality of life in community-dwelling sarcopenic and non-sarcopenic older adults: a case-control study. Clin Nutr. 2017;36:267–74.
Ter Borg S, de Groot LC, Mijnarends DM, de Vries JH, Verlaan S, Meijboom S, et al. Differences in nutrient intake and biochemical nutrient status between sarcopenic and nonsarcopenic older adults—results from the Maastricht Sarcopenia Study. J Am Med Dir Assoc. 2016;17:393–401.
Rock E, Astier C, Lab C, Vignon X, Gueux E, Motta C, Rayssiguier Y. Dietary magnesium deficiency in rats enhances free radical production in skeletal muscle. J Nutr. 1995;125:1205–10.
Latham CM, Brightwell CR, Keeble AR, Munson BD, Thomas NT, Zagzoog AM, et al. Vitamin D promotes skeletal muscle regeneration and mitochondrial health. Front Physiol. 2021;12: 660498.
Remelli F, Vitali A, Zurlo A, Volpato S. Vitamin D deficiency and sarcopenia in older persons. Nutrients. 2019;11:2861.
Liu C, Cheung WH, Li J, Chow SK, Yu J, Wong SH, et al. Understanding the gut microbiota and sarcopenia: a systematic review. J Cachexia Sarcopenia Muscle. 2021;12:1393–407.
Freedberg DE, Kim LS, Yang YX. The risks and benefits of long-term use of proton pump inhibitors: expert review and best practice advice from the American Gastroenterological Association. Gastroenterology. 2017;152:706–15.
van Diepen S, Majumdar SR, Bakal JA, McAlister FA, Ezekowitz JA. Heart failure is a risk factor for orthopedic fracture: a population-based analysis of 16,294 patients. Circulation. 2008;118:1946–52.
Sennerby U, Melhus H, Gedeborg R, Byberg L, Garmo H, Ahlbom A, et al. Cardiovascular diseases and risk of hip fracture. JAMA. 2009;302:1666–73.
Sattayalertyanyong O, Thitilertdecha P, Auesomwang C. The inappropriate use of proton pump inhibitors during admission and after discharge: a prospective cross-sectional study. Int J Clin Pharm. 2020;42:174–83.
Matsumoto A, Yoshimura Y, Nagano F, Bise T, Kido Y, Shimazu S, et al. Polypharmacy and potentially inappropriate medications in stroke rehabilitation: prevalence and association with outcomes. Int J Clin Pharm. 2022;44:749–61.
von Haehling S, Ebner N, Dos Santos MR, Springer J, Anker SD. Muscle wasting and cachexia in heart failure: mechanisms and therapies. Nat Rev Cardiol. 2017;14:323–41.
Yano T, Katano S, Kouzu H, Nagaoka R, Inoue T, Takamura Y, et al. Distinct determinants of muscle wasting in nonobese heart failure patients with and without type 2 diabetes mellitus. J Diabetes. 2021;13:7–18.
Ishikawa S, Naito S, Iimori S, Takahashi D, Zeniya M, Sato H, et al. Loop diuretics are associated with greater risk of sarcopenia in patients with non-dialysis-dependent chronic kidney disease. PLoS ONE. 2018;13: e0192990.
Hanai T, Shiraki M, Miwa T, Watanabe S, Imai K, Suetsugu A, et al. Effect of loop diuretics on skeletal muscle depletion in patients with liver cirrhosis. Hepatol Res. 2019;49:82–95.
Nakano I, Tsuda M, Kinugawa S, Fukushima A, Kakutani N, Takada S, et al. Loop diuretic use is associated with skeletal muscle wasting in patients with heart failure. J Cardiol. 2020;76:109–14.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interests
Katsuhiko Ohori, Toshiyuki Yano, Satoshi Katano, Ryohei Nagaoka, Ryo Numazawa, Kotaro Yamano, Yusuke Fujisawa, Hidemichi Kouzu, Masayuki Koyama, Nobutaka Nagano, Takefumi Fujito, Ryo Nishikawa, Wataru Ohwada, and Masato Furuhashi declare they have no conflicts of interest.
Funding
This study was supported by Grant-in-Aid for Young Scientists (Katano S) from the Japan Society for the Promotion of Science KAKENHI (grant numbers JP18K17677 and 22K11288), Tokyo, Japan. The funding body played no role in the design of the study; the collection, analysis, and interpretation of data; or writing of the manuscript.
Ethics approval
This study was conducted in strict adherence to the principles of the Declaration of Helsinki and was approved by the Clinical Investigation Ethics Committee of Sapporo Medical University Hospital (Number 302-104).
Consent to participate
Given the retrospective and anonymized nature of this study, the Clinical Investigation Ethics Committee of Sapporo Medical University Hospital waived the need for informed consent from the patients who participated in this study from November 1, 2015 to April 10, 2019. An opt-out option on our website allowed patients to decline the inclusion of their data in this study. In addition, informed consent was obtained from patients who participated in this study from April 11, 2019 to April 30, 2022.
Consent for publication
All authors provide this content.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available because a research agreement from all authors is required for data sharing, but are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author’s contributions
All authors have read and approved the manuscript. In addition, we confirm that all listed authors meet the authorship criteria and that all authors are in agreement with the content of this manuscript. KO, TY, and SK designed the study. KO, TY, SK, RNa, RNu, KY, YF, HK, MK, NN, TF, RNi, and WO collected the patients’ data. KO, TY, SK, and MF analyzed and discussed the data. KO, TY and SK performed the statistical analyses. KO, TY, and MF drafted the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ohori, K., Yano, T., Katano, S. et al. Independent Association Between Use of Proton Pump Inhibitors and Muscle Wasting in Patients with Heart Failure: A Single-Center, Ambispective, Observational Study. Drugs Aging 40, 731–739 (2023). https://doi.org/10.1007/s40266-023-01035-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-023-01035-3