Abstract
Background and Objective
Tucatinib is approved for treatment of human epidermal growth factor receptor 2-positive metastatic breast cancer. Understanding potential drug–drug interactions (DDIs) informs proper dosing when co-administering tucatinib with other therapies. The aim of this study was to evaluate DDIs between tucatinib and metabolizing enzymes and transporters in healthy volunteers.
Methods
Parts A–C assessed the impact of itraconazole (cytochrome P450 [CYP] 3A4 inhibitor), rifampin (CYP3A4/CYP2C8 inducer), or gemfibrozil (CYP2C8 inhibitor) on the pharmacokinetics of a single 300 mg dose of tucatinib administered orally and its primary metabolite, ONT-993. Parts D and E assessed the effect of steady-state tucatinib on the pharmacokinetics of repaglinide (CYP2C8 substrate), tolbutamide (CYP2C9 substrate), midazolam (CYP3A4 substrate), and digoxin (P-glycoprotein substrate).
Results
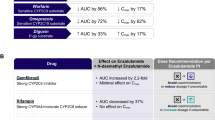
Tucatinib area under the concentration–time curve from time 0 extrapolated to infinity (AUC0–inf) increased by ~ 1.3- and 3.0-fold with itraconazole and gemfibrozil, respectively, and decreased by 48% with rifampin, indicating that tucatinib is metabolized primarily by CYP2C8, and to a lesser extent via CYP3A. Tucatinib was a strong inhibitor of CYP3A (midazolam AUC0–inf increased 5.7-fold), a weak inhibitor of CYP2C8 and P-glycoprotein, and had no impact on CYP2C9-mediated metabolism in humans. Tucatinib was well tolerated, alone and with co-administered drugs.
Conclusion
The potential DDIs identified here may be mitigated by avoiding concomitant use of tucatinib with strong CYP3A inducers, moderate CYP2C8 inducers, CYP3A substrates with a narrow therapeutic window (modifying substrate dose where concomitant use is unavoidable), and strong CYP2C8 inhibitors (decreasing tucatinib dose where concomitant use is unavoidable), or by reducing the dose of P-glycoprotein substrates with a narrow therapeutic window.
Trial Registration
This trial (NCT03723395) was registered on October 29, 2018.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Tucatinib inhibited CYP3A4, CYP2C8, and P-gp-mediated elimination, and was impacted by both CYP3A4 and CYP2C8 inhibition and induction in healthy volunteers. |
Tucatinib was well tolerated when administered either alone or concomitantly with other medications in healthy volunteers. |
In clinical practice, concomitant administration with strong CYP3A inducers, moderate CYP2C8 inducers, CYP3A substrates with a narrow therapeutic window, and strong CYP2C8 inhibitors should be avoided. |
If concomitant administration of medications which have the potential to act as CYP2C8 inhibitors is unavoidable, tucatinib dosage should be modified accordingly, and if concomitant administration of CYP3A substrates (where minimal concentration changes may lead to serious or life-threatening toxicities) or P-gp substrates is unavoidable, the substrate dosage should also be modified. |
1 Introduction
Human epidermal growth factor receptor 2 (HER2) gene overexpression or amplification is an oncogenic driver in various cancers, with multiple therapies having been developed to target HER2 [1]. However, despite the increased survival offered by these therapies, issues of resistance and toxicities have necessitated the development of additional effective and tolerable systemic therapies to extend survival in patients with HER2-positive (HER2+) cancers [2, 3].
Tucatinib is a highly selective tyrosine kinase inhibitor of the HER2 receptor. Tucatinib is approved in combination with trastuzumab and capecitabine for treatment of adult patients with advanced, unresectable, or metastatic HER2+ breast cancer (MBC), including those with brain metastases, based on demonstrated efficacy and favorable risk–benefit profile observed in the pivotal HER2CLIMB clinical trial [4,5,6]. Tucatinib is also being investigated in earlier lines of therapy for HER2+ MBC and in other HER2+ tumors [7].
Understanding potential drug–drug interactions (DDIs) helps inform appropriate dosing when co-administering tucatinib with other therapies [8]. In vitro metabolism studies in human liver microsomes suggest that the drug metabolizing enzymes cytochrome P450 (CYP) 2C8 and CYP3A4 contribute to tucatinib metabolism [5, 9]. Although there is no major metabolite in humans, the primary metabolite ONT-993, which accounts for < 10% of total pharmacological activity in humans, is formed through oxidation by CYP2C8 [9]. Concomitant medications that are inhibitors or inducers of CYP2C8 and CYP3A4 may affect tucatinib plasma concentrations in clinical practice.
In vitro, tucatinib exhibited competitive inhibition of CYP2C8, CYP2C9, CYP3A4, and P-glycoprotein (P-gp), and time/metabolism-dependent inactivation of CYP3A [5, 9]. These enzymes are involved in the metabolism of approximately 48% of therapeutic drugs that are metabolized by cytochrome P450 isoforms [10], creating a potential for clinically meaningful DDIs between tucatinib and concomitant medications.
This DDI study evaluated the magnitude of potential enzyme and transporter interactions for tucatinib (as a victim and as a perpetrator), and the safety of healthy volunteers when tucatinib was administered concomitantly with established inhibitors, inducers, and substrates of drug-metabolizing enzymes.
2 Methods
2.1 Phase I Clinical Study
The study protocol and amendments were reviewed and approved by a central institutional review board. All participants provided written informed consent for participation and publication. This study was conducted in compliance with the principles of the Declaration of Helsinki and in accordance with the International Conference on Harmonisation Guidelines for Good Clinical Practice.
2.2 Participants
Healthy adults aged 18–65 years, with a body mass index of 18.0–32.0 kg/m2, were included. Exclusion criteria included use of tobacco or other nicotine-containing products within 3 months prior to study initiation; consumption of alcohol within 48 h prior to study initiation and throughout the study; routine or chronic use of acetaminophen at a dose of > 3 g/day; and use of prescribed or over-the-counter medication, health supplements, or herbal remedies within 28 days prior to study initiation through to follow-up.
2.3 Study Design
This phase I, multicenter, open-label, fixed-sequence study (ClinicalTrials.gov identifier: NCT03723395) was conducted in five parts (A–E; Fig. 1). Participants were confined to the clinical research center on the day before initiating treatment until the day of clinic discharge.
Study schematics for assessing A the effect of comedications on tucatinib plasma exposure, and B the effect of steady-state tucatinib on the plasma exposure of co-administered drugs. BID twice daily, D day, ITZ itraconazole, MDZ midazolam, PK pharmacokinetics, QD once daily, RIF rifampin, TUC tucatinib
Part A evaluated the effect of the strong CYP3A4 inhibitor, itraconazole, on the single-dose pharmacokinetics of tucatinib. Participants received a single 300 mg dose of tucatinib administered orally 2 h after breakfast on days 1 and 6. A 200 mg dose of itraconazole was administered orally twice daily immediately after a meal on day 3 and once daily immediately after breakfast on days 4–7 (Fig. 1A). Participants were discharged from the clinic on day 8 and were assessed at a follow-up visit on day 12 (±1 day).
Part B evaluated the effect of rifampin, a strong inducer of CYP3A4 and CYP2C8, on the single-dose pharmacokinetics of tucatinib. Participants received a single, 300 mg dose of tucatinib administered orally on days 1 and 10, following an overnight fast of at least 8 h. A 600 mg dose of rifampin was administered orally once daily on days 3–11, following an overnight fast of at least 8 h (Fig. 1A). Participants were discharged from the clinic on day 12 and were assessed at a follow-up visit on day 16 (± 1 day).
Part C evaluated the effect of the strong CYP2C8 inhibitor gemfibrozil on the single-dose pharmacokinetics of tucatinib. Participants received a single 300 mg dose of tucatinib administered orally on days 1 and 7, following an overnight fast of at least 8 h. A 600 mg dose of gemfibrozil was administered orally twice daily on days 3–8, following an overnight fast of at least 8 h in the morning and approximately 30 minutes prior to the evening meal (Fig. 1A). Participants were discharged from the clinic on day 9 and were assessed at a follow-up visit on day 13 (± 1 day).
Part D evaluated the effects of steady-state tucatinib on the pharmacokinetics of substrate probes of CYP2C8 (repaglinide), CYP2C9 (tolbutamide), and CYP3A4 (midazolam). Participants received a single 0.5 mg dose of repaglinide administered orally on days 1 and 11, following an overnight fast. A 500 mg dose of tolbutamide and a 2 mg dose of midazolam were co-administered orally on days 2 and 12, following an overnight fast. A 300 mg dose of tucatinib was administered orally twice daily, at least 12 h apart, on days 4–13. On days 4, 10, 11, and 12, the morning dose was given after an overnight fast of at least 8 h. On days 11 and 12, the morning dose was given immediately after administration of repaglinide and tolbutamide/midazolam, respectively (Fig. 1B). Participants were discharged from the clinic on day 14 and were assessed at a follow-up visit on day 21 (±1 day).
Part E evaluated the effect of steady-state tucatinib on the pharmacokinetics of a substrate probe of P-gp (digoxin). Participants received a single, 0.5 mg dose of digoxin administered orally on days 1 and 15, following an overnight fast of at least 8 h. Tucatinib 300 mg was administered orally twice daily, at least 12 h apart, on days 8–21. On days 8, 14, and 15, the morning dose was given after an overnight fast of at least 8 h. On day 15, the morning dose was administered immediately after digoxin (Fig. 1B). Participants were discharged from the clinic on day 22 and were assessed at a follow-up visit on day 29 (± 1 day).
Foods and beverages containing poppy seeds, grapefruit, or Seville oranges were not allowed from 7 days prior to day −1 until the follow-up visit or early study termination. While confined to the study site, participants received a standardized diet at scheduled times that did not conflict with other study-related activities. All oral study drugs were administered with 240 mL of room-temperature water. When drugs were administered concurrently, only 240 mL of water was administered in total for all drugs. Participants were dosed upright in a seated position.
2.4 Pharmacokinetic and Pharmacodynamic Assessments
Blood samples for tucatinib and probe drug pharmacokinetics were collected pre-dose and at intervals as indicated in Supplementary Fig. S1 for parts A–E. In parts A–C, blood samples for determination of plasma concentrations of tucatinib and ONT-993 were collected at 0.5, 1, 2, 3, 4, 6, 8, 10, 12, 16, 24, 36, and 48 h post-dose on days 1 and 6 (Part A) or day 10 (Part B) or day 7 (Part C). In Parts B and C, the 48-h post-dose timepoint relevant to day 1 dosing of tucatinib was collected prior to dosing on day 3 of rifampin (Part B) or gemfibrozil (Part C). A single blood sample was collected prior to dosing for determination of trough plasma concentrations on days 4–6 for itraconazole dosing in Part A, on days 8–10 for rifampin dosing in Part B, and on days 5–7 for gemfibrozil in Part C.
In Part D, blood samples for determination of plasma concentrations of repaglinide were collected at 0.5, 1, 1.5, 2, 3, 4, 6, 8, 10, and 12 h post-dose on days 1 and 11. Blood samples for determination of plasma concentrations of midazolam and 1-hydroxymidazolam were collected at 0.5, 1, 2, 3, 4, 6, 8, 10, 12, 16, and 24 h post-dose on days 2 and 12. Blood samples for tolbutamide and 4-hydroxytolbutamide were collected at the same timepoints and also at 36 and 48 h post-dose. The 48-h post-dose timepoint relative to day 2 dosing was collected prior to the morning dose of tucatinib on day 4. In Part E, blood samples for determination of plasma concentrations of digoxin were collected at 0.5, 1, 2, 3, 4, 6, 8, 10, 12, 16, 24, 48, 72, 96, 120, 144, and 168 h post-dose on days 1 and 15. In Parts D and E, blood samples for determination of plasma concentrations of tucatinib and ONT-993 were collected at 0.5, 1, 2, 3, 4, 6, 8, 10, and 12 h after the morning dose of tucatinib on days 4, 10, 11, and 12 (Part D) or days 8, 14, and 15 (Part E). The 12-h post-dose samples were collected prior to administration of the second daily dose of tucatinib.
2.5 Quantitative Assays
Plasma concentrations of tucatinib, ONT-993, itraconazole, rifampin, gemfibrozil, repaglinide, tolbutamide, 4hydroxytolbutamide, midazolam, 1-hydroxymidazolam, and digoxin were determined using validated bioanalytical procedures, performed by Covance (Madison, WI, USA).
Protein precipitation was used for extraction of tucatinib, ONT-993, itraconazole, gemfibrozil, rifampin, tolbutamide, and 4-hydroxytolbutamide; liquid-liquid extraction for midazolam, 1-hydroxymidazolam, and digoxin; and supported-liquid extraction for repaglinide. Analyte detection and quantification was carried out by liquid chromatography with tandem mass spectrometry (LC-MS/MS) as described in the Data Supplement. Details of the reference analytes and internal standards are given in Supplementary Table S1 (see electronic supplementary material [ESM]).
2.6 Laboratory Evaluations and Safety Assessments
Blood and urine samples were collected, after at least an 8-h fast, for clinical laboratory evaluations at specific times during the study for Parts A–E. Clinical chemistry, hematology, and urinalysis evaluations were performed at screening, check-in, and follow-up, and regularly at protocol-specified timepoints in all parts of the study. Assays for cystatin C and urine albumin-to-creatinine ratio were performed at all these timepoints except screening in Part D, and for all but the first six patients enrolled in Part E, following a protocol amendment.
Safety assessments included recording of all treatment-emergent adverse events (TEAEs), clinical laboratory parameters, vital signs, 12-lead electrocardiogram, and physical examination.
2.7 Statistical Analysis
Pharmacokinetic analysis was conducted by Covance Early Clinical Biometrics using WinNonlin Version 8.1 (Certara L.P., Princeton, NJ, USA). Pharmacokinetic parameters were determined, as appropriate, from the plasma concentrations of tucatinib, concomitant drugs, and metabolites using non-compartmental methods.
The pharmacokinetic parameters were area under the plasma concentration–time curve from time 0 to the last available measurement (AUC0–last), area under the plasma concentration–time curve from time 0 to infinity (AUC0–inf), and maximum observed plasma concentration (Cmax) for tucatinib, repaglinide, tolbutamide, midazolam, and digoxin. A linear mixed-model analysis was applied to analyze the natural log-transformed pharmacokinetic parameters, which included treatment as a fixed effect and subject as a random effect. The impact of drug co-administration on the pharmacokinetic parameters for each part of the study was assessed by deriving estimates of geometric mean ratios, together with the corresponding 90% confidence intervals (CIs), for comparison between reference and test timepoints (days 1 and 6 in Part A, days 1 and 10 in Part B, days 1 and 7 in Part C, days 1 and 11 for repaglinide and days 2 and 12 for tolbutamide and midazolam in Part D, and days 1 and 15 for digoxin in Part E). Exploratory analyses of the geometric mean ratios and 90% CIs of AUC0–inf, AUC0–last, and Cmax for metabolites ONT-993, 4-hydroxytolbutamide, and 1-hydroxymidazolam were evaluated as required.
Other pharmacokinetic parameters estimated by noncompartmental analysis included time to Cmax, terminal elimination half-life, apparent total clearance (tucatinib, repaglinide, tolbutamide, midazolam, and digoxin), apparent total clearance at steady state (tucatinib in Parts D and E only), metabolic ratio based on AUC0–inf, and metabolic ratio based on Cmax.
3 Results
3.1 Study Participants
Parts A, B, and C each enrolled 28 participants, all of whom were evaluable for safety and pharmacokinetics. In Part D, all 17 participants enrolled were evaluable for safety and pharmacokinetics. In Part E, of the 15 participants enrolled, 2 were withdrawn from the study on day 8 due to non-treatment-related upper respiratory infections and did not receive tucatinib, leaving 13 participants evaluable for safety and pharmacokinetics. Participant demographics are summarized in Supplementary Table S2 (see ESM).
3.2 Impact of Inducers and Inhibitors of Metabolizing Enzymes on Tucatinib
The CYP3A4 inhibitor itraconazole, in combination with tucatinib, increased the plasma exposure of tucatinib approximately 1.3-fold based on AUC0–last, AUC0–inf, and Cmax compared with tucatinib alone (Fig. 2, Table 1). This effect was statistically significant based on 90% CI values. Consistent with this, mean clearance was lower and mean terminal elimination half-life was longer for tucatinib in combination with itraconazole than for tucatinib alone (Supplementary Table S3, see ESM). Plasma exposure of ONT-993, indicated by the geometric least squares mean ratios for AUC0–inf and Cmax, also was increased by coadministration of itraconazole (1.6 and 2.0, respectively). However, this is most likely due to the increased plasma exposure of tucatinib in the presence of itraconazole. The metabolic ratios for ONT-993 were similar or slightly higher in the presence of itraconazole as compared with tucatinib alone (Supplementary Table S3, see ESM).
Tucatinib plasma concentration profiles (A, D, G), AUC0–inf values (B, E, H), and Cmax values (C, F, I) in the absence and presence of steady-state itraconazole (A–C), rifampin (D–F), or gemfibrozil (G–I). Solid lines inside the box plots represent the median. The boxes represent the 25th and 75th percentile and the whiskers represent the minimum and maximum values. AUC0–inf area under the concentration–time curve from time 0 extrapolated to infinity, Cmax maximum observed concentration, CYP cytochrome P450, GEM gemfibrozil, ITZ itraconazole, RIF rifampin
The strong CYP3A4 inducer and moderate CYP2C8 inducer rifampin, in combination with tucatinib, decreased the plasma exposure of tucatinib approximately 48% based on AUC0–last and AUC0–inf, and 37% based on Cmax, compared with tucatinib alone (Fig. 2, Table 1). This effect was statistically significant, based on 90% CI values. Consistent with this, mean clearance for tucatinib was increased in combination with rifampin as compared with tucatinib alone, while terminal half-life was similar (Supplementary Table S4, see ESM). Co-administration of rifampin decreased the plasma exposure and increased the Cmax of ONT-993 (Supplementary Table S4, see ESM). The metabolic ratios for AUC0–inf and Cmax of ONT-993 were 1.4-fold and 3.3-fold higher, respectively, in the presence of rifampin than with tucatinib alone (Supplementary Table S4, see ESM).
The strong CYP2C8 inhibitor gemfibrozil, in combination with tucatinib, increased plasma exposure of tucatinib approximately 3.0-fold based on AUC0–last and AUC0–inf, and 1.6-fold based on Cmax, compared with administration of tucatinib alone (Fig. 2, Table 1). This effect was statistically significant, based on 90% CI values. Coadministration of gemfibrozil decreased the plasma exposure of ONT-993, with a statistically significant effect on Cmax (Supplementary Table S5, see ESM). The metabolic ratios for AUC0–inf and Cmax of ONT-993 were decreased by approximately 71% and 81%, respectively, following administration of gemfibrozil, compared with tucatinib alone (Supplementary Table S5, see ESM).
3.3 Impact of Tucatinib on Substrates of Metabolizing Enzymes and Transporters
Administration of tucatinib in combination with tolbutamide/midazolam significantly increased the plasma exposure of the CYP3A4 substrate, midazolam, 5.3-, 5.7-, and 3.0-fold based on AUC0–last, AUC0–inf, and Cmax, respectively, compared with administration of tolbutamide/midazolam alone (Fig. 3, Table 2). The lower mean clearance and longer mean terminal half-life of midazolam in the presence of tucatinib, as compared with tolbutamide/midazolam administered alone, are consistent with this effect (Supplementary Table S6, see ESM). Although tucatinib had no effect on the exposure of the metabolite 1-hydroxymidazolam, based on AUC0–last and AUC0–inf, Cmax was reduced by approximately 40%. Tucatinib had a strong effect on the metabolism of midazolam, reducing the metabolic ratios for AUC0–inf and Cmax by approximately 83% and 80%, respectively (Supplementary Table S7, see ESM).
Plasma concentration profiles, AUC0–inf values, and Cmax values of midazolam (A–C), repaglinide (D–F), tolbutamide (G–I), or digoxin (J–L) in the absence and presence of steady-state tucatinib. Solid lines inside the box plots represent the median. The boxes represent the 25th and 75th percentile and the whiskers represent the minimum and maximum values. AUC0–inf area under the concentration–time curve from time 0 extrapolated to infinity, Cmax maximum observed concentration, CYP cytochrome P450, MDZ midazolam, P-gp P-glycoprotein, TUC tucatinib
Administration of tucatinib in combination with the CYP2C8 substrate repaglinide increased the plasma exposure of repaglinide approximately 1.6- and 1.7-fold, based on AUC0–inf and Cmax, respectively, compared with administration of repaglinide alone (Fig. 3, Table 2). Consistent with this, mean clearance of repaglinide was lower in the presence of tucatinib than when administered alone (Supplementary Table S7, see ESM).
The plasma exposures of the CYP2C9 substrate tolbutamide were similar after administration of tolbutamide/midazolam in combination with tucatinib and after administration of tolbutamide/midazolam alone (Fig. 3, Table 2). Similar plasma exposures were also observed for the metabolite 4-hydroxytolbutamide before and after tucatinib coadministration (Supplementary Table S8, see ESM). The metabolic ratios for AUC0–inf and Cmax of 4hydroxytolbutamide were similar before and after tucatinib coadministration (Supplementary Table S8, see ESM).
Administration of tucatinib in combination with the P-gp substrate digoxin increased plasma exposure of digoxin approximately 1.5-fold based on AUC0–last and AUC0–inf, and 2.4-fold based on Cmax, compared with administration of digoxin alone (Fig. 3, Table 2). Consistent with this, the mean clearance of digoxin was lower in the presence of tucatinib than when administered alone (Supplementary Table S9, see ESM).
3.4 Safety
Tucatinib was well tolerated in Parts A–E of the study, either after single 300 mg doses alone or when administered in combination with other drugs, or after multiple days of twice-daily dosing either alone or in combination with other drugs. Overall, in Parts A through E, 37 of 114 (32.5%) subjects reported a total of 71 TEAEs. The majority of TEAEs were mild (65 events in total were considered Grade 1) and considered unrelated to tucatinib. No Grade 3 or higher events were reported. There were no deaths or serious adverse events, and all but two TEAEs resolved by end of study. The two TEAEs that had not resolved by end of study were considered unrelated to tucatinib.
TEAEs considered related to tucatinib (Supplementary Table S10, see ESM) were consistent with its known safety profile. Increases in serum creatinine are recognized to occur with tucatinib due to inhibition of renal tubular transport of creatinine without affecting glomerular function [11]. These were observed after dosing of tucatinib alone or in combination with probe drugs, both in the single-dose and the multiple-dose parts of the study. Serum creatinine increases were observed in 14 (50%) participants in Part A, none of which were reported as TEAEs; in one (4%) participant in Part B, which was recorded as a Grade 1 TEAE; in 19 (68%) participants in Part C, none of which were TEAEs; in 12 (71%) participants in Part D, one of which was a Grade 2 TEAE; and in seven (54%) participants in Part E, five of which were Grade 1 TEAEs (Supplementary Table S10, see ESM). Most of these elevations were transient and resolved after cessation of tucatinib dosing. Assessment of renal function by cystatin C levels in Parts D and E did not reveal any elevated values, and no out-of-range urine albumin or urine albumin-to-creatinine ratios were observed, suggesting no corresponding effect on glomerular filtration rate or overall renal function.
Elevations in hepatic transaminases (alanine aminotransferase [ALT] and/or aspartate aminotransferase [AST]), which have been reported previously in subjects receiving tucatinib [4, 12,13,14,15], were noted, especially after multiple dosing of tucatinib in Parts D and E. Overall, five events of ALT elevation and two events of AST elevation were reported as Grade 1 TEAEs during the study in Parts D and E (Supplementary Table S10, see ESM). These were generally transient, reversible, and resolved after cessation of tucatinib dosing. Other tucatinib-related adverse events were limited in Parts A–E of the study and included one participant with diarrhea each in Part A and Part E, one participant with pruritus each in Part D and Part E, one participant with dry skin each in Part B and Part E, one participant with headache each in Part C and Part E, one event of blood bilirubin increase in Part B, one participant with dizziness in part E, and one participant with gout and arthralgia in Part C.
4 Discussion
Interactions between co-administered medications can contribute to morbidity and mortality of patients, particularly if unanticipated or mismanaged [8]. This phase I study evaluated the clinical significance of potential interactions between tucatinib and metabolizing enzymes and transporters identified in studies in vitro.
An absorption, metabolism, and excretion study determined that oxidative metabolism was the predominant clearance route for tucatinib in humans (NCT03758339). In that study, ONT-993 was the most abundant radioactive component in urine and feces, accounting for 1.5% and 37% of the dose, respectively [16]. This, and findings from in vitro studies, indicated the primary role of CYP2C8 in the metabolism of tucatinib [5, 16]. The effect of inducers and inhibitors of metabolizing enzymes on tucatinib pharmacokinetics, as observed in Parts A–C of this DDI study, confirmed that CYP2C8 is the main metabolizing enzyme by which DDIs may affect tucatinib plasma levels, with CYP3A4 playing a lesser role. In clinical practice, if co-administration of tucatinib with concomitant medications that are strong CYP2C8 inhibitors cannot be avoided, potential DDIs may be mitigated by reducing the tucatinib starting dose to 100 mg twice daily [5, 6]. Comedication with drugs that are moderate CYP2C8 inhibitors can be managed by monitoring for tucatinib-related adverse events [5, 6]. Coadministration of tucatinib with moderate CYP2C8 inducers, such as rifampin or St John’s Wort, should also be avoided as it may lead to decreased tucatinib activity [5, 6].
Parts D and E of this study, which investigated the effect of steady-state tucatinib levels on substrates for the metabolizing enzymes CYP3A4, CYP2C8, and CYP2C9, and the transporter P-gp, indicated that tucatinib is a strong CYP3A4 inhibitor, only weakly inhibits CYP2C8 and P-gp, and has no impact on CYP2C9 metabolism in humans. Approximately 30% of all clinically used drugs have been estimated to be metabolized predominantly by CYP3A metabolizing enzymes, and another ~ 18% by CYP2C8 or CYP2C9 [10]. CYP3A4 inhibition can increase plasma levels of substrate drugs and potentially increase the risk of toxicity [10]. The most clinically relevant DDIs are usually considered to be those causing > 5-fold increases in plasma exposure or those where the drug has a narrow therapeutic index [17]. A > 5-fold increase in midazolam AUC0–inf occurred when administered in combination with tucatinib, identifying tucatinib as a strong CYP3A4 inhibitor and indicating the potential for clinically relevant interactions with tucatinib and sensitive CYP3A4 substrates. It is recommended that tucatinib comedication should be avoided with drugs that are CYP3A4 substrates where minimal concentration changes may lead to serious or life-threatening toxicities [5].
This study confirmed the major role of CYP2C8 in the metabolism of tucatinib. Genetic variations in CYP2C8 can impact the overall clearance of a drug: the CYP2C8*2, CYP2C8*3, and CYP2C8*4 single nucleotide polymorphisms have all been associated with changes in metabolizing activity, such as decreased clearance of paclitaxel with CYP2C8*3 and CYP2C8*4 [10]. However, the clinical relevance of these polymorphisms is unclear. In an exploratory genotyping analysis of 84 subjects enrolled in this study, similar tucatinib exposures were observed regardless of phenotype (65 extensive metabolizers, 16 extensive or intermediate metabolizers, two intermediate metabolizers, one unknown, and no poor metabolizers were included in the analysis), hence the impact of CYP2C8 polymorphisms on the exposure of tucatinib and ONT-993 is inconclusive [9].
Consistent with other tucatinib studies, elevated serum creatinine was observed in all parts of this study; these events were mostly transient, largely not recorded as TEAEs, and resolved on cessation of tucatinib dosing [4, 11]. The rapid, reversible, and clinically insignificant elevations in serum creatinine that have been observed with tucatinib administration have been shown to result from inhibition of the multidrug and toxin extrusion 1/2-K (MATE1/2-K) transporter by tucatinib, which increases serum creatinine without affecting glomerular function [4, 11]. Additionally, normal values for cystatin C, urine albumin, and urine albumin-to-creatinine ratios were observed in this study, further depicting that tucatinib had no impact on glomerular filtration rate or overall renal function. Through all parts of the study, tucatinib was well tolerated, and almost all TEAEs were resolved by the end of the study.
The dosing of tucatinib in this study was established in prior clinical studies. The recommended therapeutic dose of tucatinib 300 mg BID [5] was used in Parts D and E as it was expected to provide sufficient plasma concentrations to assess the effects of tucatinib on CYP2C8, CYP2C9, CYP3A4, and P-gp. A single 300 mg dose was selected for Parts A, B, and C as it had previously been well tolerated in healthy subject clinical studies [5, 9] and would provide sufficient plasma concentrations to assess the effects of CYP3A4 and CYP2C8 inhibition and induction. Tucatinib can be administered with or without food, as food has no clinically relevant impact on tucatinib exposures [5]. In Part A, tucatinib was administered in the fed state as itraconazole must be taken with food [18]. The exposures of rifampin, gemfibrozil, repaglinide, and digoxin are affected by food [19,20,21,22], so in Parts B–E, tucatinib was administered in the fasted state to avoid any potential food-related interactions.
The substrates, inducers, and inhibitors used in this study are commonly used and well established to investigate drug interactions. For example, itraconazole has been widely used as the standard strong CYP3A4 inhibitor in DDI studies since 2013, when it replaced ketoconazole due to its improved safety profile [23]. Additionally, combinations of multiple drugs, such as midazolam and tolbutamide used in Part D of this study, have been tested in drug cocktail studies to confirm they have no pharmacokinetic or pharmacodynamic interactions that might confound the findings when used in DDI studies [24].
This DDI study was performed in healthy volunteers and helps to inform the drug interaction guidance for tucatinib use in clinical practice. However, we acknowledge that the potential clinical effects of such DDIs in patients with cancer may differ.
5 Conclusion
We have evaluated the impact of potential DDIs of tucatinib, suggested by in vitro studies, with established inhibitors, inducers, and substrates of drug-metabolizing enzymes. Tucatinib plasma concentrations were affected by strong CY3A4 inducers, moderate CYP2C8 inducers, and inhibitors of CYP2C8, whereas inhibition of CYP3A4 metabolism produced a minor effect. Tucatinib was a strong inhibitor of CYP3A4 and a weak inhibitor of P-gp. Medications considered for concomitant administration with tucatinib should therefore be carefully evaluated for their potential to act as strong inducers of CYP3A4 or moderate inducers of CYP2C8, inhibitors of CYP2C8, or to be sensitive substrates of CYP3A4 or P-gp.
References
Siena S, Sartore-Bianchi A, Marsoni S, Hurwitz HI, McCall SJ, Penault-Llorca F, et al. Targeting the human epidermal growth factor receptor 2 (HER2) oncogene in colorectal cancer. Ann Oncol. 2018;29(5):1108–19.
Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro MS, Andre F, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann Oncol. 2020;31(12):1623–49.
Choong GM, Cullen GD, O’Sullivan CC. Evolving standards of care and new challenges in the management of HER2-positive breast cancer. CA Cancer J Clin. 2020;70(5):355–74.
Murthy RK, Loi S, Okines A, Paplomata E, Hamilton E, Hurvitz SA, et al. Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. N Engl J Med. 2020;382(7):597–609.
Seagen Inc. Tukysa (tucatinib) US prescribing information. 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213411s000lbl.pdf. Accessed 18 Jan 2022.
Seagen Inc. Tukysa (tucatinib) European summary of product characteristics. 2021. https://www.ema.europa.eu/en/documents/product-information/tukysa-epar-product-information_en.pdf. Accessed 18 Jan 2022.
Strickler JH, Zemla T, Ou FS, Cercek A, Wu C, Sanchez FA, et al. Trastuzumab and tucatinib for the treatment of HER2 amplified metastatic colorectal cancer (mCRC): Initial results from the MOUNTAINEER trial. Ann Oncol. 2019;30: v200.
Food and Drug Administration. Clinical drug interaction studies—cytochrome P450 enzyme- and transporter-mediated drug interactions: guidance for industry. 2020. https://www.fda.gov/media/134581/download. Accessed 18 Jan 2022.
Food and Drug Administration. Multi-disciplinary review and evaluation-NDA 213411 (tucatinib). 2019. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2020/213411Orig1s000MultidisciplineR.pdf. Accessed 18 Jan 2022.
Zanger UM, Schwab M. Cytochrome P450 enzymes in drug metabolism: regulation of gene expression, enzyme activities, and impact of genetic variation. Pharmacol Ther. 2013;138(1):103–41.
Topletz-Erickson AR, Lee AJ, Mayor JG, Rustia EL, Abdulrasool LI, Wise AL, et al. Tucatinib inhibits renal transporters OCT2 and MATE without impacting renal function in healthy subjects. J Clin Pharmacol. 2021;61(4):461–71.
Metzger Filho O, Leone JP, Li T, Tan-Wasielewski Z, Trippa L, Barry WT, et al. Phase I dose-escalation trial of tucatinib in combination with trastuzumab in patients with HER2-positive breast cancer brain metastases. Ann Oncol. 2020;31(9):1231–9.
Murthy R, Borges VF, Conlin A, Chaves J, Chamberlain M, Gray T, et al. Tucatinib with capecitabine and trastuzumab in advanced HER2-positive metastatic breast cancer with and without brain metastases: a non-randomised, open-label, phase 1b study. Lancet Oncol. 2018;19(7):880–8.
Borges VF, Ferrario C, Aucoin N, Falkson C, Khan Q, Krop I, et al. Tucatinib combined with ado-trastuzumab emtansine in advanced ERBB2/HER2-positive metastatic breast cancer: a phase 1b clinical trial. JAMA Oncol. 2018;4(9):1214–20.
Moulder SL, Borges VF, Baetz T, McSpadden T, Fernetich G, Murthy RK, et al. Phase I study of ONT-380, a HER2 inhibitor, in patients with HER2(+)-advanced solid tumors, with an expansion cohort in HER2(+) metastatic breast cancer (MBC). Clin Cancer Res. 2017;23(14):3529–36.
Sun H, Cardinal K, Wienkers L, Chin A, Kumar V, Neace C, et al. Elimination of tucatinib, a small molecule kinase inhibitor of HER2, is primarily governed by CYP2C8 enantioselective oxidation of gem dimethyl. Cancer Chemother Pharmacol. 2022;89(6):737–50.
Yu J, Wang Y, Ragueneau-Majlessi I. Pharmacokinetic drug-drug interactions with drugs approved by the U.S. Food and Drug Administration in 2020: mechanistic understanding and clinical recommendations. Drug Metab Dispos. 2021;50(1):1–7.
Sanico NV. Itroconazole US prescribing information. 2010. https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022484s000lbl.pdf. Accessed 5 Apr 2022.
Sanofi. Rifadin (rifampin) US prescribing infomration. 2010. https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/050420s073,050627s012lbl.pdf. Accessed 22 Mar 2022.
Inc NN. Prandin (repaglinide) US prescribing information. 2008. https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020741s035lbl.pdf. Accessed 22 Mar 2022.
Pfizer. Lopid (gemfibrozil) US prescribing information. 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/018422s048lbl.pdf. Accessed 22 Mar 2022.
Concordia Pharmaceuticals Inc. Lanoxin (digoxin prescribing infomration). 2016. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/020405s013lbl.pdf. Accessed 22 Mar 2022.
Liu L, Bello A, Dresser MJ, Heald D, Komjathy SF, O’Mara E, et al. Best practices for the use of itraconazole as a replacement for ketoconazole in drug-drug interaction studies. J Clin Pharmacol. 2016;56(2):143–51.
Blakey GE, Lockton JA, Perrett J, Norwood P, Russell M, Aherne Z, et al. Pharmacokinetic and pharmacodynamic assessment of a five-probe metabolic cocktail for CYPs 1A2, 3A4, 2C9, 2D6 and 2E1. Br J Clin Pharmacol. 2004;57(2):162–9.
Acknowledgements
The authors would like to thank the study participants, their families, and the principal investigators involved in this study, Dr. Jennifer Zon and Dr. Hugh Coleman, both of Covance Clinical Research Unit, Inc. Medical writing support was provided by Lucy Smithers, Ph.D., and Charlotte Simpson, Ph.D., and editorial support was provided by Travis Taylor, both of Prime Global, supported by Seagen Inc., according to Good Publication Practice 3 guidelines (https://www.acpjournals.org/doi/10.7326/M15-0288). The sponsor was involved in the study design and collection, analysis and interpretation of data, as well as data checking of information provided in the manuscript. However, ultimate responsibility for opinions, conclusions, and data interpretation lies with the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding for this publication was provided by Seagen Inc. (Bothell, Washington, USA).
Conflict of interest
This study was funded by Seagen Inc. The authors wrote the article with the assistance of a medical writer funded by the sponsor. All the authors had full access to the relevant data, vouch for the completeness and accuracy of the data and for adherence of the trial to the protocol, assume final responsibility for the content of the article, and for the decision to submit the article for publication. A. Topletz-Erickson, A. Lee, E.L. Rustia, H. Sun, J.G. Mayor, L.I. Abdulrasool, L. Walker, and C.J. Endres are employees of Seagen and hold stocks and shares in Seagen. No authors are Fellows of the American College of Clinical Pharmacology.
Ethics approval
WCG IRB, a central institutional review board, reviewed and approved all study materials prior to initiating recruitment and data collection.
Consent to participate
Informed consent was obtained from all participants prior to commencing enrolment.
Consent for publication
All authors provided this consent.
Data sharing
Qualified researchers may request access to certain data and related study documents consistent with the Principles for Responsible Clinical Trial Data Sharing. Interested researchers can use http://www.clinicalstudydatarequest.com to request access to anonymized patient-level data and supporting documents from clinical studies to conduct further research that can help advance medical science or improve patient care.
Code availability
Not applicable.
Author contributions
All authors contributed to the study design, and analysis and interpretation of data. All authors contributed to critical revisions of the article and provided their final approval for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Topletz-Erickson, A., Lee, A., Rustia, E.L. et al. Evaluation of Safety and Clinically Relevant Drug–Drug Interactions with Tucatinib in Healthy Volunteers. Clin Pharmacokinet 61, 1417–1426 (2022). https://doi.org/10.1007/s40262-022-01144-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-022-01144-z